© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
CASE REPORT
Combined interstitial laser cauterisation
of placental anastomosis and intrauterine intracardiac transfusion following monochorionic co-twin demise: a case report
PW Hui, MD, FRCOG; Mimi TY Seto, MB, BS, FHKAM (Obstetrics and Gynaecology); KW Cheung, MB, BS, FHKAM (Obstetrics and Gynaecology
Department of Obstetrics and Gynaecology, Queen Mary Hospital, Hong Kong
Corresponding author: Dr PW Hui (apwhui@hku.hk)
Case report
Single fetal demise in monochorionic pregnancy is
associated with significant morbidity and mortality
of the co-twin. We report the case of a 36-year-old
nulliparous woman with unexpected single fetal
demise in a monochorionic twin pregnancy
diagnosed at 15 weeks and 4 days. She had been well
since her last normal scan at 13 weeks and 3 days
and no discordance in crown rump length or nuchal
translucency thickness had been evident. Non-invasive
prenatal testing for common aneuploidy
screening was negative.
Ultrasound showed demise of one twin and
scalp oedema and ascites in the surviving co-twin.
Cardiothoracic ratio was elevated to 0.59 and
tricuspid regurgitation was seen. Peak systolic
velocity (PSV) of the middle cerebral artery (MCA)
was increased to 2.18 multiples of median (MoM;
45.1 cm/s) and diastolic flow in the umbilical artery
was absent. Cord insertion was velamentous and
an arterial anastomosis was identified along the
placental surface from the surviving twin to the
placental cord insertion of the miscarried twin
(Fig 1a and b).
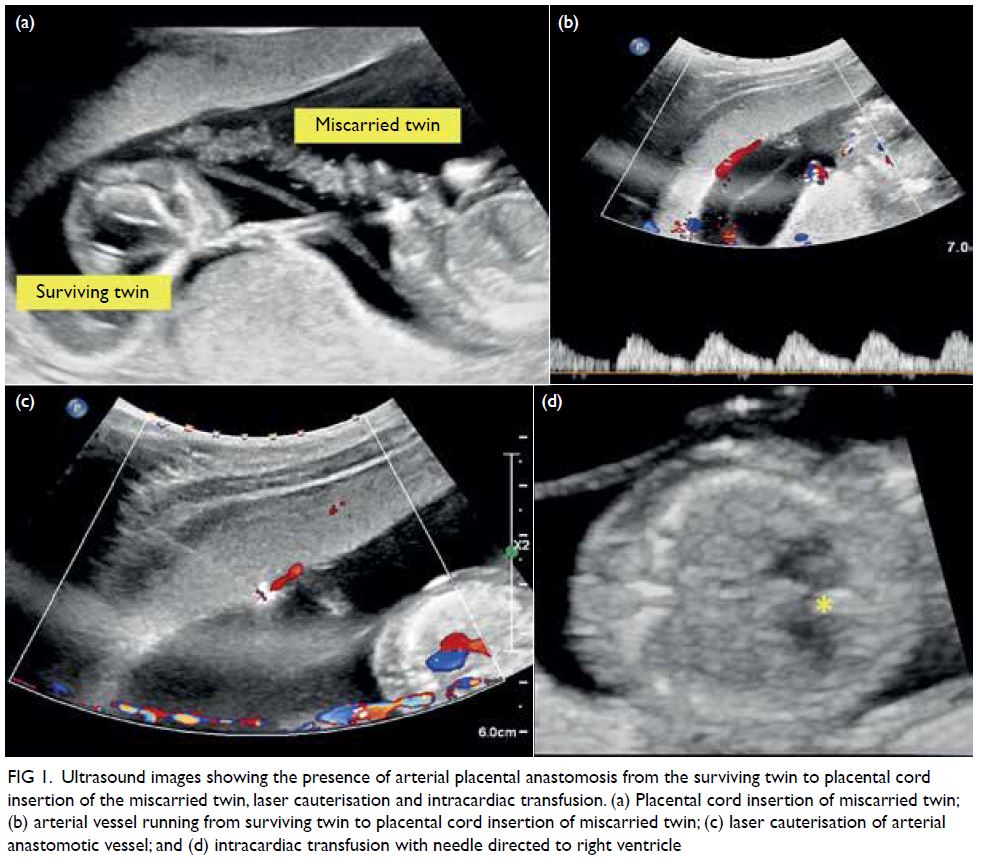
Figure 1. Ultrasound images showing the presence of arterial placental anastomosis from the surviving twin to placental cord insertion of the miscarried twin, laser cauterisation and intracardiac transfusion. (a) Placental cord insertion of miscarried twin; (b) arterial vessel running from surviving twin to placental cord insertion of miscarried twin; (c) laser cauterisation of arterial anastomotic vessel; and (d) intracardiac transfusion with needle directed to right ventricle
The couple were counselled extensively on
management options that included termination
of pregnancy, conservative management, or active
intrauterine interventions. Within 24 hours, the
patient opted to undergo rescue transfusion for fetal
anaemia and interstitial laser cauterisation of the
placental anastomosis. Interstitial laser cauterisation
was performed using an 18G spinal needle inserted
transplacentally under ultrasound guidance to the
anastomotic artery close to the cord insertion of the
miscarried twin. A 780-μm laser fibre was advanced
to 3 mm beyond the needle tip. Cauterisation was
started with a 20-W diode laser and stepped up to
40 W for 100 s. Fetal heart pulsation was checked
intermittently and was normal throughout.
Cessation of blood flow was confirmed by colour
Doppler ultrasonography (Fig 1c).
Intracardiac transfusion was performed the next day via a 22G needle directed to the fetal
right ventricle (Fig 1d). Before the transfusion,
haemoglobin was 4.2 g/dL and haematocrit was
10.5%. Transfusion of 4.5-mL O positive blood
with haematocrit of 80% and irradiated for
cytomegalovirus was uneventful. No bradycardia or
pericardial effusion occurred. After the transfusion,
haemoglobin was 12.6 g/dL and haematocrit was
37.2%. The MCA PSV was 48.7 cm/s (2.35 MoM)
before the laser cauterisation and 50 cm/s
(2.39 MoM) before the transfusion. It was reduced
to 0.9 MoM after the transfusion. Other workup for
fetal hydrops was negative.
The patient was monitored by weekly
ultrasound for level of MCA PSV MoM and
resolution of hydrops. Ascites disappeared 5 days
after transfusion and MCA PSV was 1.3 MoM.
Subcutaneous oedema subsided 1 week later and
cardiothoracic ratio improved to 0.56. Fetal magnetic
resonance imaging and detailed echocardiography at
22 weeks of gestation showed no abnormality. A loop
of prominent bowel was noticed after 23 weeks of
gestation. This was progressively dilated to 1.72 cm
at 33 weeks of gestation. Peristalsis was present and
bowel atresia was suspected. The patient went into
preterm labour at 34 weeks and 2 days, delivering a
baby boy weighing 1960 g. An area of cauterisation
on the placental surface was evident next to the cord
insertion of the miscarried twin (Fig 2).
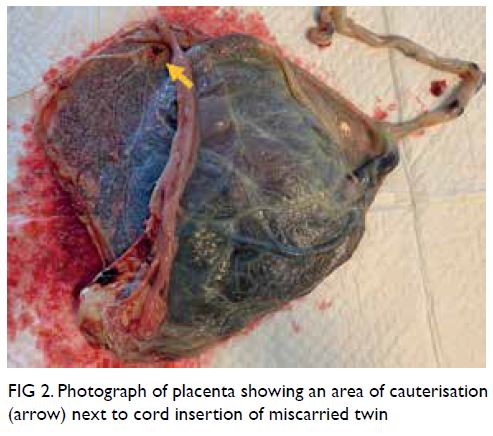
Figure 2. Photograph of placenta showing an area of cauterisation (arrow) next to cord insertion of miscarried twin
Neonatal laparotomy on day 1 showed
type 4 intestinal atresia. Resection of multiple
atretic segments of the small bowel and primary
anastomosis were performed. A second laparotomy
was required on day 34 for resection of rectal atresia.
Bowel function returned to normal afterwards. The
baby had grade 1 intraventricular haemorrhage that
resolved spontaneously and at age 5 months he had
reached the appropriate developmental milestones.
Discussion
Single twin demise occurs in monochorionic
pregnancies with twin-twin transfusion syndrome (TTTS) and selective intrauterine growth restriction
but may also occur unexpectedly in pregnancies with
no obvious complications.1 Feto-fetal haemorrhage through the placenta anastomosis leads to acute
hypovolaemia and results in fetal anaemia, cerebral
damage or death of the co-twin.1 2 Bowel and renal
complications have also been reported.3 4 The
present case illustrates successful intervention with
a combination of interstitial laser to a placental
anastomosis and intracardiac transfusion for a fetus
at 15 weeks of gestation following monochorionic
co-twin demise. The risk of co-twin demise and
neonatal death is increased significantly in cases
of single intrauterine fetal death in monochorionic
pregnancies before 28 weeks.5 The surviving fetus
is also at risk of other morbidity secondary to feto-fetal
haemorrhage and hypoperfusion. Neurological
damage affects almost 20% of co-twin survivors
especially in fetuses demonstrating signs of fetal
anaemia.1 6 This can be assessed by measuring
MCA PSV.7 A value >1.55 MoM is suggested to be
associated with a fivefold increase in the relative risk
of cerebral injury.1
Rescue intrauterine transfusion has been
proposed for an anaemic monochorionic survivor.8
The optimal timing of transfusion and impact on overall long-term outcome remain debatable. Feto-fetal
haemorrhage may continue after intrauterine
transfusion. It is, therefore, rational to conduct a
sonographic search for placental anastomosis and
perform cauterisation to cease further feto-fetal
haemorrhage prior to intrauterine transfusion. In this
case, an arterial vessel running towards the placental
cord insertion of the miscarried twin was identified.
With the presence of this anastomosis, rescue
transfusion for the surviving fetus was unlikely to be
effective as fetal anaemia could persist. Interstitial
laser has been reported in cauterisation of feeding
vessels in chorioangioma, fetal hyperechogenic lung
lesion, and sacrococcygeal teratoma.9 Adopting the
principle of intrauterine laser ablation in TTTS,
a laser fibre was inserted via a 18G spinal needle
transplacentally to cauterise this vessel under
ultrasound guidance. A fetoscopic approach was
not considered in view of the early gestation with an
anterior placenta and absence of polyhydramnios.
The energy requirement was guided by generation of
an echogenic area around the fibre tip encompassing
the vessel and cessation of blood flow on Doppler
ultrasound.
Intracardiac fetal transfusion was performed
because of the early gestation and difficult
intravascular assess. This technique was first
introduced in the late 1980s.10 Experience was
gathered mainly from transfusing fetuses that
were anaemic due to rhesus isoimmunisation or
parvovirus infection reported as early as 16 weeks
of gestation.11 12 13 Transient fetal bradycardia,
haemopericardium, pericardial tamponade, and
asystole are known complications.10 11 12
To the best of our knowledge, this is the
first report of successful rescue of an anaemic
co-twin survivor in a monochorionic pregnancy
by combining laser to placental anastomosis and
intracardiac transfusion as early as 15 weeks of
gestation. Time was required for blood product
preparation and also allowed the fetus to establish a
new circulatory equilibrium following laser therapy
when the ongoing transfusion was completed. It is
of interest to note that fetal ascites may be an early
presentation of bowel complications secondary
to in-utero anaemia.3 Mesenteric ischaemia in
monochorionic twins has been postulated to be
related to haemodynamic alteration in case of co-twin
demise, hypoperfusion, and/or hyperviscosity
in TTTS or thromboembolic phenomenon after
laser ablation. Ascites might also be an indication
of circulatory insufficiency even in the absence of
severe fetal anaemia. Evidence of transient cardiac
failure has been reported after single fetal death in
monochorionic twins and immediate intrauterine
transfusion has been advocated to restore the
circulatory volume.2
This case did not have features of TTTS although ascites, cardiomegaly, and tricuspid
regurgitation were noted after co-twin demise
and before intrauterine intervention. Although
fetal anaemia was ascertained and hypovolaemic
shock was likely present, it is not always possible
to determine whether the ascites is secondary to
circulatory insufficiency or bowel complications. As
well as treating fetal anaemia, intrauterine transfusion
may also correct circulatory insufficiency and
restore cardiac function. The prompt intervention
in this fetus led to complete resolution of the
ultrasound abnormalities and possibly improved the
neurological outcomes. The fetus required further
monitoring for bowel complications that might only
become obvious at a later stage of gestation.
In managing co-twin demise in a
monochorionic pregnancy, assessment of the
survivor requires detailed ultrasound examination
to search for placental anastomosis, as well as an
immediate assessment for signs of fetal anaemia and
bowel or haemodynamic complications. Early laser
cauterisation of placental anastomosis to control
feto-fetal haemorrhage is an option combined with
rescue intrauterine transfusion to prevent anaemia
and circulatory insufficiency in the surviving twin.
Author contributions
All authors contributed to the concept of the study, acquisition
of the data, and analysis of the data, and critical revision of
the manuscript for important intellectual content. PW Hui
drafted the manuscript. All authors had full access to the
data, contributed to the study, approved the final version
for publication, and take responsibility for its accuracy and
integrity.
Conflicts of interest
All authors have disclosed no conflicts of interest.
Funding/support
This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Ethics approval
The patient was treated in accordance with the Declaration of Helsinki and provided informed consent for all procedures.
References
1. Lanna MM, Consonni D, Faiola S, et al. Incidence of
cerebral injury in monochorionic twin survivors after
spontaneous single demise: long-term outcome of a large
cohort. Fetal Diagn Ther 2020;47:66-73. Crossref
2. Iwagaki S, Takahashi Y, Chiaki R, Asai K, Matsui M,
Katsura D. Case of resuscitation from cardiac failure
by intrauterine transfusion after single fetal death in
monochorionic twin pregnancy. J Obstet Gynaecol Res
2019;45:2105-10. Crossref
3. Tan LN, Cheung KW, Philip I, Ong S, Kilby MD. Isolated
ascites in a monochorionic twin after fetoscopic laser
ablation is not necessarily secondary to recurrence or anaemia: bowel complications in twin-to-twin transfusion
syndrome after fetoscopic laser ablation. Fetal Diagn Ther
2019;45:285-94. Crossref
4. Genova L, Sueters M, van Steenis A, Oepkes D, Steggerda SJ,
Lopriore E. Renal failure after single fetal demise in
monochorionic twins: incidence and description of a case.
Fetal Diagn Ther 2014;35:302-5. Crossref
5. Mackie FL, Rigby A, Morris RK, Kilby MD. Prognosis of
the co-twin following spontaneous single intrauterine fetal
death in twin pregnancies: a systematic review and metaanalysis.
BJOG 2019;126:569-78. Crossref
6. Mackie FL, Morris RK, Kilby MD. Fetal brain injury in
survivors of twin pregnancies complicated by demise of
one twin: a review. Twin Res Hum Genet 2016;19:262-7. Crossref
7. Senat MV, Loizeau S, Couderc S, Bernard JP, Ville Y. The
value of middle cerebral artery peak systolic velocity in the
diagnosis of fetal anemia after intrauterine death of one
monochorionic twin. Am J Obstet Gynecol 2003;189:1320-4. Crossref
8. Quarello E, Stirnemann J, Nassar M, et al. Outcome of anaemic monochorionic single survivors following early
intrauterine rescue transfusion in cases of feto-fetal
transfusion syndrome. BJOG 2008;115:595-601. Crossref
9. Mathis J, Raio L, Baud D. Fetal laser therapy: applications
in the management of fetal pathologies. Prenat Diagn
2015;35:623-36. Crossref
10. Westgren M, Selbing A, Stangenberg M. Fetal
intracardiac transfusions in patients with severe rhesus
isoimmunisation. Br Med J (Clin Res Ed) 1988;296:885-6. Crossref
11. von Kaisenberg CS, Grebe S, Schleider S, Kuhling-von
Kaisenberg H, Venhoff L, Meinhold-Heerlein I. Successful
intrauterine intracardiac transfusion in monochorionic
twins affected by parvovirus B19. Fetal Diagn Ther
2007;22:420-4. Crossref
12. Mackie FL, Pretlove SJ, Martin WL, Donovan V, Kilby MD.
Fetal intracardiac transfusions in hydropic fetuses with
severe anemia. Fetal Diagn Ther 2015;38:61-4. Crossref
13. Yinon Y, Visser J, Kelly EN, et al. Early intrauterine
transfusion in severe red blood cell alloimmunization.
Ultrasound Obstet Gynecol 2010;36:601-6. Crossref

