Hong Kong Med J 2021 Aug;27(4):247–57 | Epub 13 Aug 2021
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE
Impact of appropriate empirical antibiotics on
clinical outcomes in Klebsiella pneumoniae bacteraemia
MY Man, MB, BS, FHKAM (Medicine); HP Shum, MB, BS, MD; KC Li, MB, ChB; WW Yan, MB, BS, FHKAM (Medicine)
Department of Intensive Care, Pamela Youde Nethersole Eastern Hospital, Hong Kong
Corresponding author: Dr MY Man (mayman729@gmail.com)
Abstract
Introduction: Klebsiella pneumoniae infections can cause septic shock, multiorgan failure, and death.
Methods: This retrospective cohort study included
adults with K pneumoniae bacteraemia treated from
1 January 2009 to 30 June 2017. Demographics,
microbiology, and outcomes were analysed. The
primary outcome was 90-day all-cause mortality;
secondary outcomes were intensive care unit (ICU)
and hospital mortalities, ICU and hospital lengths of
stay, and ICU ventilator duration.
Results: In total, 984 patients had K pneumoniae
bacteraemia; of them, 686 received appropriate
empirical antibiotics. Overall, 205 patients required
intensive care. Older age (odds ratio [OR]=1.60;
95% confidence interval [CI]=1.120-2.295; P=0.010),
chronic kidney disease (OR=1.81; 95% CI=1.181-
2.785; P=0.007), mechanical ventilation (OR=1.79;
95% CI=1.188-2.681; P=0.005), pneumonia
(OR=1.50; 95% CI=1.030-2.187; P=0.034), and
carbapenem-resistant or extended-spectrum betalactamase
(ESBL)–producing isolates (OR=12.51;
95% CI=7.886-19.487; P<0.001) were associated with
greater risk of inappropriate empirical treatment.
Ninety-day mortality was significantly higher among
patients with inappropriate empirical treatment;
independent predictors included pneumonia (hazard
ratio [HR]=2.94; 95% CI=2.271-3.808; P<0.001),
gastrointestinal infection (HR=2.77; 95% CI=2.055-3.744; P<0.001), failed empirical antibiotics
(HR=2.45; 95% CI=1.928-3.124; P<0.001), older
age (HR=1.79; 95% CI=1.356-2.371; P<0.001), solid
tumour (HR=1.77; 95% CI=1.401-2.231; P<0.001),
carbapenem-resistant or ESBL-producing isolates
(HR=1.64; 95% CI=1.170-2.297; P=0.004), patients
admitted through the Department of Medicine
(HR=1.39; 95% CI=1.076-1.800; P=0.012), and higher
total Sequential Organ Failure Assessment score
(HR=1.09; 95% CI=1.058-1.112; P=0.023). Among
ICU patients, inappropriate empirical antibiotic
treatment was significantly associated with increased
ventilator duration and 90-day mortality.
Conclusions: Klebsiella pneumoniae bacteraemia
was associated with high 90-day and ICU mortalities;
90-day mortality increased with inappropriate
empirical antibiotic treatment.
New knowledge added by this study
- This large study of Klebsiella pneumoniae bacteraemia among patients in Hong Kong and South East Asia showed that 90-day mortality was significantly higher in patients who received inappropriate empirical treatment.
- Intensive care unit subgroup analysis showed that inappropriate empirical treatment was the strongest predictor of 90-day mortality in critically ill patients.
- Independent predictors for inappropriate empirical treatment were older age, chronic kidney disease, mechanical ventilation, pneumonia, and either carbapenem resistance or extended-spectrum beta-lactamase production.
- Extensive efforts are needed to facilitate early, appropriate use of empirical antibiotics, including the use of a current antibiogram, implementation of multidisciplinary sepsis management guidelines, and establishment of protocols among pharmacists, microbiologists, clinicians, and nurses.
- Careful assessment of empirical antibiotic treatment may be warranted in patients with pneumonia, gastrointestinal infection, failed empirical antibiotics, older age, solid tumour, patients admitted through the Department of Medicine, and/or higher total Sequential Organ Failure Assessment score.
Introduction
Klebsiella pneumonia causes various clinically
important infections. In 2017, K pneumoniae was
the third most common isolate in intensive care
units (ICUs) and second most common isolate in all
patients in the Hong Kong East Cluster.1
The emergence of multidrug-resistant
K pneumoniae infections is an increasing concern.2
There have been outbreaks of extended-spectrum
beta-lactamase (ESBL)–producing strains,
carbapenem-resistant (CR) and carbapenemase-producing
(CP) strains, and hypervirulent
K pneumoniae infections both in Hong Kong and
worldwide.2 3 4 In Greece and Italy, CP K pneumoniae
comprises 68.3% of all K pneumoniae strains.5
The importance of appropriate early empirical
antibiotics has been repeatedly emphasised in
the management of septic shock by the Surviving
Sepsis Campaign 2016.6 Previously, we highlighted
the importance of appropriate early antibiotics for successful patient outcomes.4 To the best of our
knowledge, risk factors for receiving inappropriate
empirical antibiotics have not yet been explored.
Therefore, in the present study, we aimed to evaluate
the impact of appropriate empirical antibiotics
on outcomes in patients with K pneumoniae
bacteraemia; we also performed subgroup analysis
on ICU patients with K pneumoniae bacteraemia.
Methods
Study design and data collection
We conducted a retrospective analysis of adult
patients with K pneumoniae bacteraemia who were
admitted to Pamela Youde Nethersole Eastern
Hospital within the period from 1 January 2009 to
30 June 2017. Pamela Youde Nethersole Eastern
Hospital is a 1700-bed hospital in Hong Kong which
provides extensive services except cardiothoracic
surgery, transplant surgery, and burns. Patients
were excluded if they were aged <18 years or had
incomplete information. Patient medical records
were reviewed, as were data in clinical management
and clinical information systems (IntelliVue Clinical
Information Portfolio; Philips Medical, Amsterdam,
The Netherlands). The clinical management system
is a database that stores patients’ demographics,
laboratory results, and drug administration
records for all public hospitals in Hong Kong. In
the event of missing data, medical records were
reviewed manually. Baseline demographics, clinical
characteristics, and microbiological data for all
included patients were identified from the above
databases and medical records.
Disease severity was quantified using the
maximum Sequential Organ Failure Assessment
(SOFA) score.7 The following clinical outcome data
were investigated: use of invasive organ supports
(eg, inotropic use, mechanical ventilation, and
renal replacement therapies), ICU and hospital
lengths of stay (LOSs), ICU ventilator duration, and
mortality. The primary outcome was 90-day all-cause
mortality; secondary outcomes were ICU and
hospital mortalities, ICU and hospital LOSs, and
ICU ventilator duration.
Definitions
Klebsiella pneumoniae bacteraemia was defined as the growth of K pneumoniae in one or more
blood cultures. If more than one positive blood
culture result was recorded, only the first sample
was included. Empirical antibiotic treatment was
defined as the antibiotic used within 24 hours
after a culture sample was collected. The empirical
antibiotic treatment was considered appropriate if at
least one of the antibiotic agents was consistent with
the in vitro susceptibility results.8 9 10 Community-acquired
infection was defined as K pneumoniae identified in patients upon admission or within
48 hours after admission; hospital-acquired infection
was defined as K pneumoniae identified in patients
at >48 hours after admission.11 Hepatobiliary
sepsis comprised liver abscess, cholangitis, and
cholecystitis; gastrointestinal sepsis comprised
spontaneous bacterial peritonitis, peritonitis caused
by bowel perforation, and intra-abdominal abscesses
(excluding liver abscess). Medical co-morbidities
(eg, diabetes mellitus, cirrhosis, congestive heart
failure, chronic renal impairment, haematological
malignancy and solid tumour) were defined in
accordance with the International Classification
of Disease coding. Prior steroid use was defined
as oral or intravenous steroid consumption within
30 days before the index positive blood culture result.
Chemotherapy use was defined as oral or intravenous
infusion of biological agents or chemotherapy
administered within 30 days before the index
positive blood culture result. Any antibiotics usage
within 30 days before the index hospital admission
was regarded as prior antibiotics usage.
Microbiology
Blood cultures were incubated and processed.
Blood culture results were considered negative
if no positive growth occurred after 5 to 7 days.
Susceptibility interpretation was based on Clinical
and Laboratory Standards Institute interpretive
criteria. The ESBL testing was based on Clinical and
Laboratory Standards Institute testing criteria12 13 14 15 16 17 18
or the double-disk synergy test described by
Jarlier et al.19 Regarding CR K pneumoniae, the
isolates were sent to the Public Health Laboratory
Centre of Hong Kong if further genetic testing was
required to confirm carbapenemase production.
Multiplex real-time polymerase chain reaction
assays were performed to detect Classes A, B, and D
carbapenemase gene targets.
Statistical analysis
We compared the characteristics and clinical
parameters between patients treated with appropriate
and inappropriate empirical antibiotics, as well as
between 90-day survivors and non-survivors. Results
are expressed as the median ± interquartile range
(IQR) or as the number (percentage) of patients, as
appropriate.
Categorical variables were compared by the
Pearson Chi squared test or Fisher’s exact test, as
appropriate for univariate analysis. Continuous
variables were compared by using the Mann–Whitney
U test. Variables with P<0.2 in univariate analysis or
with clinical significance from previous studies were
included in the multivariate analysis. Independent
predictors for 90-day mortality were assessed by Cox
regression analysis. Logistic regression analysis was
used to assess independent predictors for receiving appropriate and inappropriate empirical antibiotics.
Post hoc analysis was performed for patients with
chronic renal failure and resistant organisms.
The Statistical Package for Social Sciences
(Windows version 24.0; IBM Corp, Armonk [NY],
US) was used to perform statistical analyses.
Results
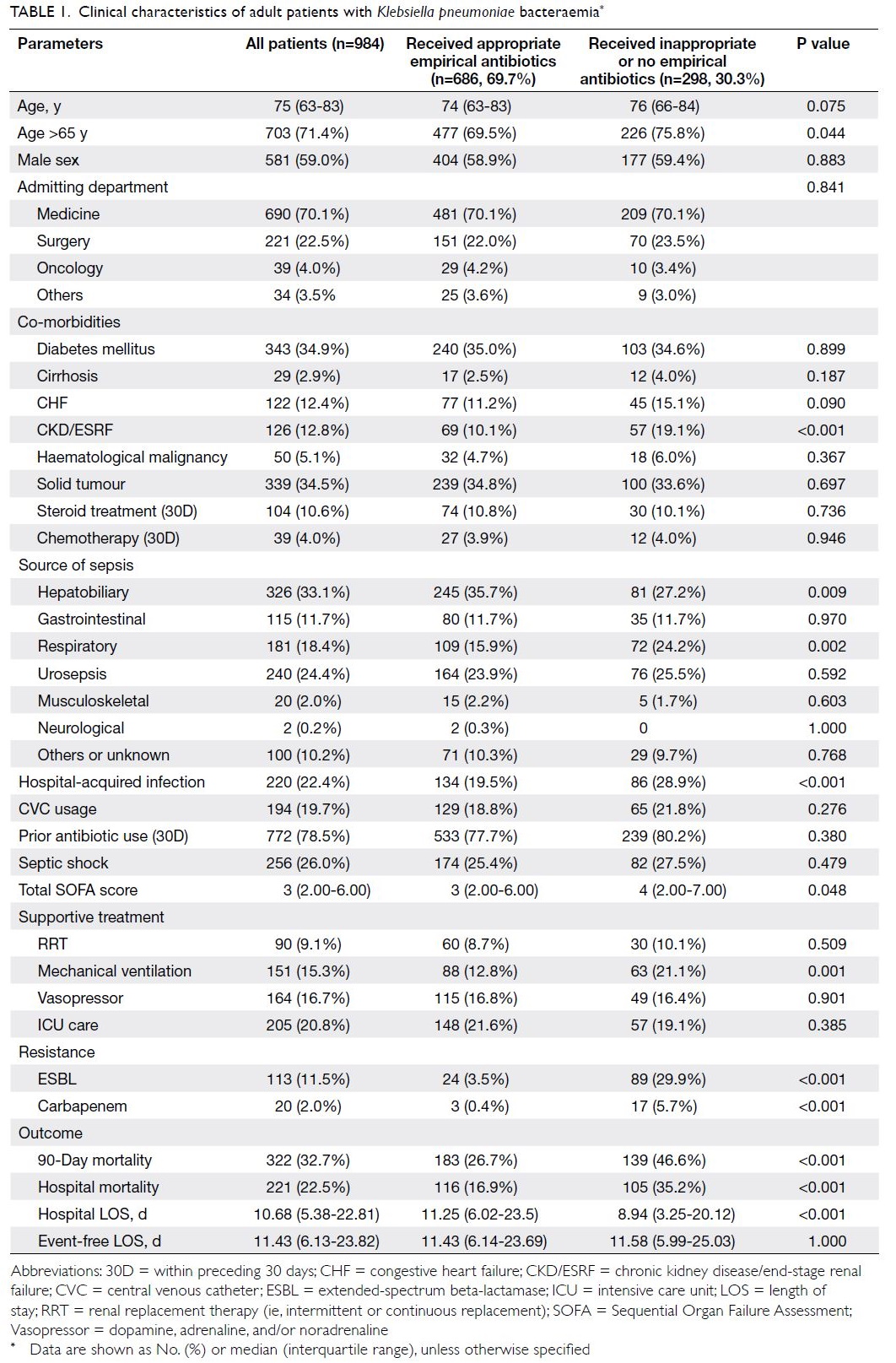
Baseline characteristics
During the 8.5-year study period, we identified 984 patients with K pneumoniae bacteraemia;
of these, 686 (69.7%) and 298 (30.3%) received
appropriate and inappropriate empirical
antibiotics, respectively. Table 1 shows the baseline
demographics of patients who received appropriate
and inappropriate empirical antibiotics. The median
patient age was 75 years (IQR=63-83 years). The most
common types of infection were hepatobiliary tract
infection (33.1%), urosepsis (24.4%), and respiratory
tract infection (18.4%). The overall 90-day mortality
was 32.7%, hospital mortality was 22.5%, and median
hospital LOS was 10.68 days (5.38-22.81 days,
P<0.001).
Appropriateness of empirical antibiotics
Univariate analysis (Table 1) revealed that the
risk factors for receiving inappropriate empirical
antibiotics were age >65 years (P=0.044), chronic
renal impairment (P<0.001), respiratory tract
infection (P=0.002), mechanical ventilation
(P=0.001), CR or ESBL-producing isolates (both
P<0.001), and higher total SOFA score (P=0.048).
Hepatobiliary sepsis was associated with a higher
rate of appropriate empirical antibiotic treatment
(P=0.009).
Table 2 demonstrates the logistic regression
analysis of the predictors for the appropriateness
of empirical antibiotics for all patients and ICU
subgroup. These include older patients (P=0.010),
chronic kidney disease (P=0.007), mechanical
ventilation (P=0.005), respiratory tract infection
(P=0.034), and either carbapenem resistance or ESBL
production (P<0.001). Table 1 shows that the 90-day
and hospital mortalities were significantly higher
in patients with inappropriate empirical treatment
(both P<0.001). Moreover, the hospital LOS was
shorter in patients who received inappropriate
empirical antibiotics (P<0.001).
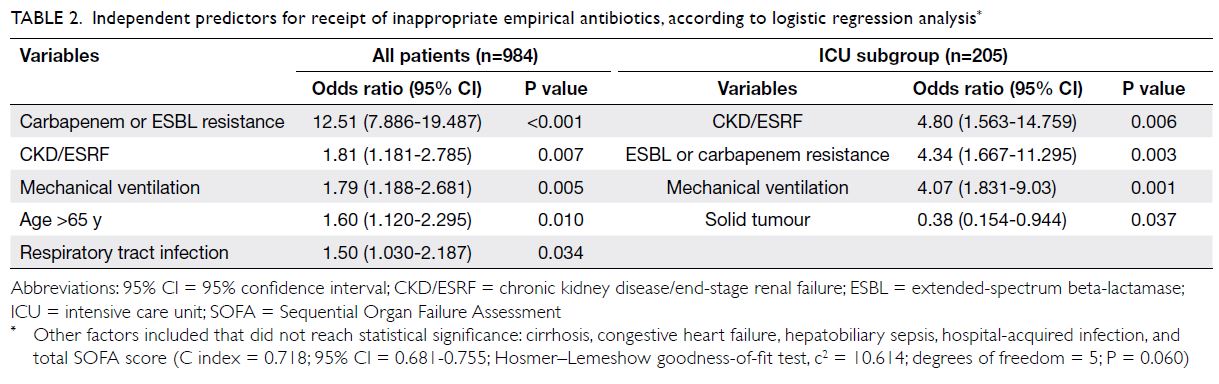
Table 2. Independent predictors for receipt of inappropriate empirical antibiotics, according to logistic regression analysis
Receipt of inappropriate empirical antibiotics
was associated with higher hospital mortality;
this finding was consistent in ICU subgroup (56%
vs 23%). The absolute risk increases in mortality
associated with the receipt of inappropriate empirical
antibiotics were 18.3% and 33% in ICU subgroup.
The number of inappropriate empirical antibiotics
associated with each mortality was five in the ICU
subgroup and three in all patients.
Multidrug-resistant Klebsiella pneumoniae infections
Antibiograms showing the proportions of non-susceptible
K pneumoniae isolates are described in
the Online Supplementary Table 1. Twenty (2.0%) patients
had CR K pneumoniae bacteraemia, but molecular
tests in the Public Health Laboratory Centre of Hong
Kong revealed that none of them had CP strains.
Overall, 113 (11.5%) patients had ESBL-producing
infections.
Post hoc analysis revealed that patients with chronic renal failure were more likely to have
ESBL infections (18.3% vs 10.5%; P=0.011) and CR
infections (0.056% vs 0.015%; P=0.003).
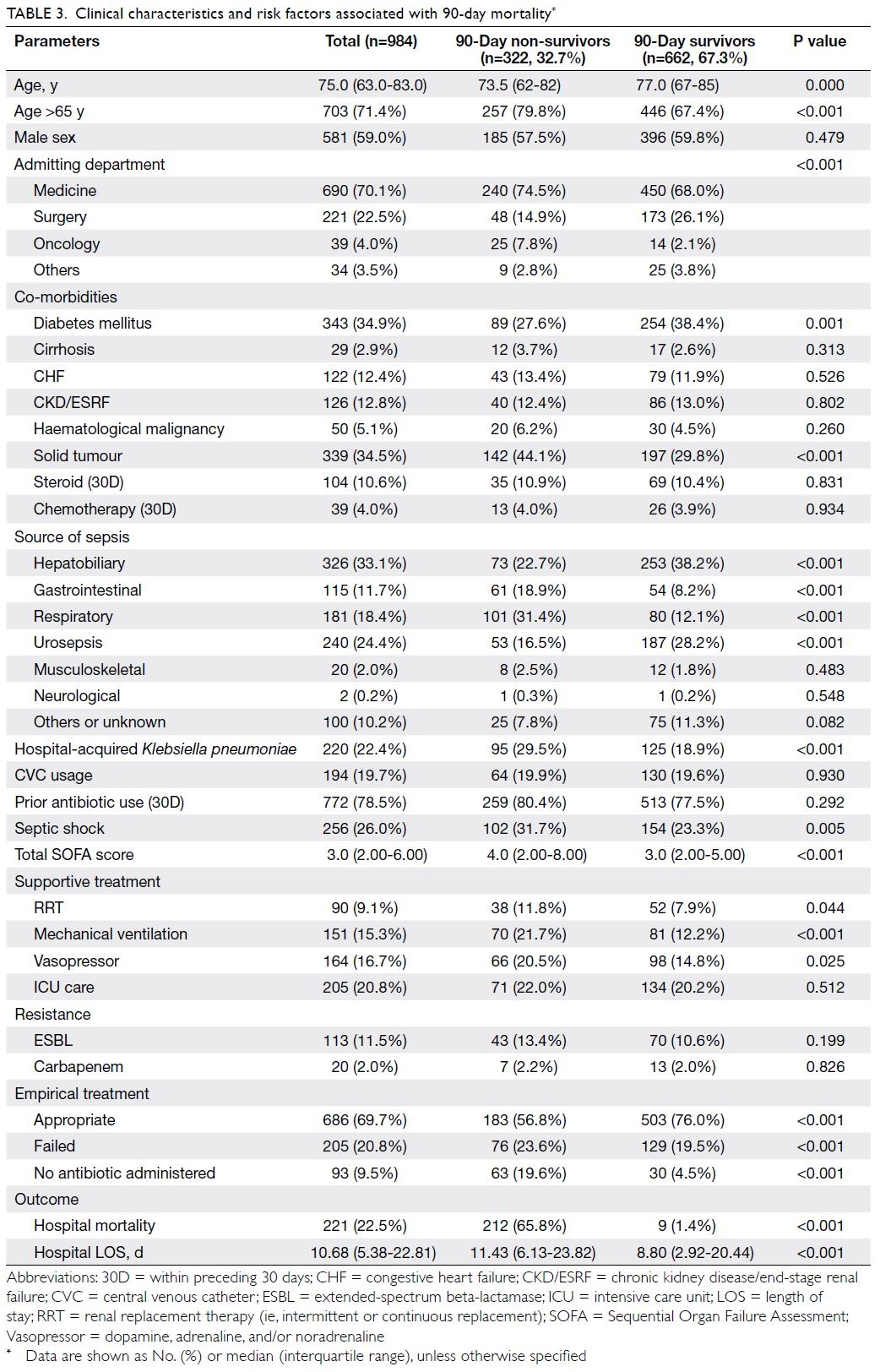
Ninety-day mortality
The 90-day all-cause mortalities were 32.7% in all patients with K pneumoniae bacteraemia and 34.6%
in the ICU subgroup. Univariate analysis (Table 3)
showed that 90-day non-survivors were more likely
to be aged >65 years (P<0.001), admitted through
the Department of Medicine (P<0.001), have septic
shock (P=0.005), have a higher total SOFA score
(P<0.001), receive inappropriate or no empirical
antibiotics (P<0.001 and P<0.001, respectively),
have solid tumour (P<0.001), have respiratory tract
infection (P<0.001), be mechanically ventilated
(P<0.001), have gastrointestinal infections (P<0.001),
and require renal replacement therapy (P=0.044).
Patients with diabetes (P=0.001), hepatobiliary
sepsis (P<0.001), and urosepsis (P<0.001) had lower
90-day mortalities.
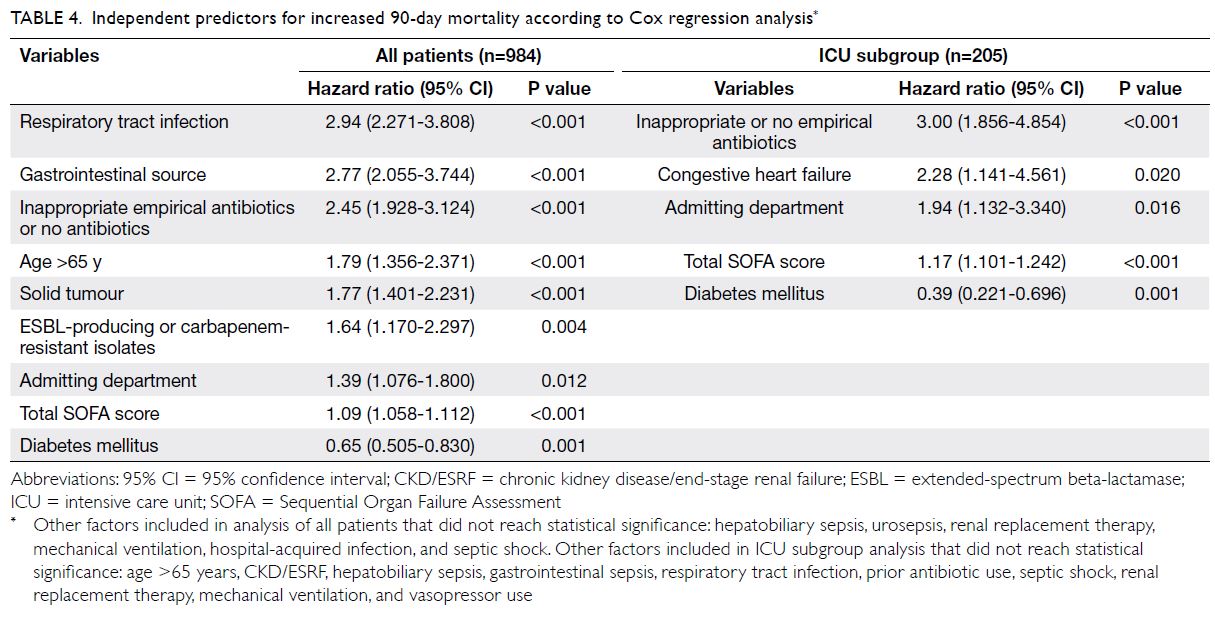
Table 4 shows the Cox regression analysis
of predictors for 90-day mortality. Independent
predictors for increased 90-day mortality were
respiratory tract infection (P<0.001), gastrointestinal
infection (P<0.001), inappropriate empirical
antibiotics (P<0.001), older age (P<0.001), solid
tumour (P<0.001), patients admitted through the
Department of Medicine (P=0.012), and higher total SOFA score (P<0.001). Patients with diabetes had
lower 90-day mortality (P=0.001). The Figure shows
the Kaplan–Meier survival plot and according to log
rank analysis, the results demonstrated a statistically
significant improvement in survival among patients
who received appropriate empirical antibiotics
(P<0.001).
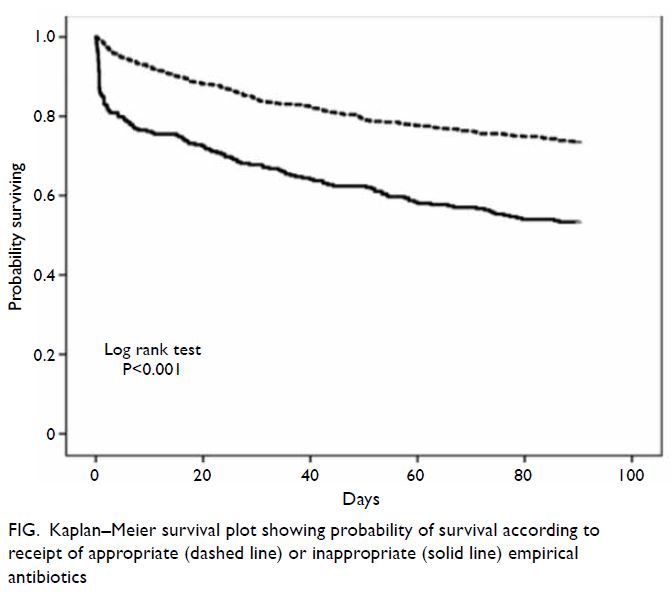
Figure. Kaplan–Meier survival plot showing probability of survival according to receipt of appropriate (dashed line) or inappropriate (solid line) empirical antibiotics
Intensive care unit subgroup analysis
Online Supplementary Table 2 shows the
demographics for inappropriate empirical
antibiotics by logistic regression analysis in ICU
subgroup. Overall, 205 (20.8%) patients required
intensive care; among them, 148 (72.2%) received
appropriate empirical antibiotics, while 57 (27.8%)
received inappropriate or no empirical antibiotics.
The median patient age was 68 years (IQR=58-78
years). The commonest infection was hepatobiliary
infections (42.9%), followed by respiratory tract
(23.4%) and urosepsis (14.6%). Furthermore, 82.4%
of the patients had septic shock, 33.2% received
renal replacement therapy, 60% received mechanical
ventilation, and 78.5% had vasopressor use. The ICU
and overall 90-day mortalities were 18.5% and 34.6%,
respectively. The receipt of inappropriate empirical
antibiotics was significantly associated with higher
90-day mortality (59.6% vs 25.0%; P<0.001), higher
ICU mortality (35.1% vs 12.2%; P<0.001), higher
hospital mortality (56.1% vs 23.0%; P<0.001), and
longer ventilator duration (2 d vs 1 d, P=0.026).
Cox regression analysis showed that the
receipt of inappropriate or no empirical antibiotics
(P<0.001; Table 4) was the strongest independent
predictor of 90-day mortality in critically ill patients
with K pneumoniae bacteraemia. Other independent
predictors were congestive heart failure (P=0.02),
admitted through the Department of Medicine
(P=0.016), and a higher total SOFA score (P<0.001).
Ninety-day non-survivors had longer hospital LOS
(P<0.001).
Discussion
Appropriateness of empirical antibiotics
Among all patients in this study, 686 (69.7%) received
appropriate empirical antibiotics. Furthermore,
148 (72.2%) critically ill patients received appropriate
empirical antibiotics. Importantly, 93 (9.5%) patients
did not receive any empirical antibiotics. The median
hospital LOS for these 93 patients was significantly
shorter than the LOS for all patients in the study.
We performed event-free survival analysis and
found that the LOSs were similar in both groups;
these findings suggested that patients who received
inappropriate antibiotics had more severe disease
and earlier death, leading to a shorter hospital LOS.
Micek et al20 found that prior antibiotic exposure was a risk factor for inappropriate empirical therapy.
Lautenbach et al21 described a positive correlation
between the total cumulative dose of antibiotics and
ESBL K pneumoniae infection. In our cohort, prior
antibiotics exposure was not significantly correlated
with inappropriate empirical antibiotic treatment;
furthermore, prior antibiotics exposure was not
associated with ESBL infections. We examined
the presence of prior antibiotics use 30 days prior
to positive blood culture results, but information
regarding the total cumulative antibiotics exposure
in terms of dosing and duration were not available.
Other information was unavailable regarding
antibiotics prescribed outside hospital settings.
Patients with chronic renal failure are
reportedly more prone to developing resistant
infections.22 They were at greater risk of receiving
inappropriate antibiotics. Additionally, hospital-acquired infection has been associated with a higher
rate of inappropriate empirical antibiotic treatment
and higher 90-day mortality.11
Multidrug-resistant Klebsiella pneumoniae
infection
The rates of CR and CP K pneumoniae bacteraemia
were much lower than the rates reported in other endemic countries.5 A study from Shanghai reported that approximately 22% of all patients
with K pneumoniae bacteraemia had CR infections;
moreover, approximately 59% of the isolates were CR
infections in patients who required intensive care.23
The prevalence of ESBL K pneumoniae
bacteraemia in Hong Kong is low.4 The ESBL
infection rate in our cohort was 11.5%, similar to
previous local studies.1 24 Another study in China
demonstrated a much higher rate of ESBL infections
(approximately 39%).25 Both ESBL and CR infections
were not associated with increased mortality in our
study in either the overall patient population or the
ICU subgroup. However, ESBL and CR infections
were significantly associated with longer hospital
LOS.
The antibiotics sensitivity in our cohorts
was comparable with the antibiogram data in the
IMPACT guideline.1 Ampicillin-sulbactam or
amoxicillin-clavulanate is recommended as the
drug of choice for treatment of K pneumomiae
infections in local guidelines.1 In our cohort, more
than 80% of K pneumomiae isolates were susceptible
to amoxicillin-clavulanate, indicating that it is a
reasonable option for broad empirical coverage.
Add-on therapy with aminoglycoside improves
the coverage of this regimen, because more than
90% of the isolates in our cohort were sensitive to
either gentamicin or amikacin. While combination
therapy improves the chance of successful empirical
therapy, routine use of combination therapy remains
controversial.6
Ninety-day mortality
The 90-day all-cause mortalities in our study were
comparable with the findings in previous studies.24 26
Respiratory tract infections and gastrointestinal
infections have consistently been associated with a
worse outcome and greater mortality.27 28 In contrast,
urosepsis and hepatobiliary sepsis have repeatedly
associated with better survival outcomes.29
These sources of infections may be amendable to
percutaneous, endoscopic, or surgical drainage,
allowing more rapid and definitive control of sepsis,
which leads to better survival.28
A greater proportion of patients with
respiratory tract infection did not receive any
empirical antibiotics, which might explain the worse
outcomes in these patients. The symptoms and
signs of respiratory tract infection may overlap with
other diseases (eg, heart failure) and treatment may
be delayed while waiting for laboratory results and
imaging. Given the greater proportion of patients
with respiratory tract infections who did not receive
any empirical antibiotics, there is a need for early
consideration of empirical antibiotics in patients
with signs and symptoms of respiratory tract
infections.
Consistent with the findings of previous
studies, we found that older age, solid tumour, and
admission through the Department of Medicine were
factors associated with higher 90-day mortality.30 31
Patients with these factors were more likely to have
other pre-existing co-morbidities, worse premorbid
functional status, and be institutionalised. They may
also have received a more conservative approach to
treatment overall.
Diabetes mellitus is well-known to predispose
patients to infections, such that affected patients
are reportedly 4.4-fold more likely to develop
bloodstream infection.32 Similar to the findings by
Peralta et al,32 we did not find increased mortality
among patients with diabetes. In our cohort,
diabetic patients were more likely to had urosepsis
than respiratory tract infections. Greater frequency
of urosepsis and smaller frequency of respiratory
tract infection may have an overall positive effect
on survival. Moreover, advances in diabetes care in
recent decades (eg, newer generations of medication
and integrated multidisciplinary care) have led to
neutral effects of diabetes on short-term mortality in
patients undergoing major operations and patients
with sepsis.34 34 35 Glycaemic status, haemoglobin A1c
levels, and diabetes severity were not available in
the present study; thus, we could not delineate how
diabetes control affected bacteraemia outcomes.
Our results are limited to demonstrating that 90-day
mortality and diabetes have a greater impact on
long-term survival, although this conclusion may
not be apparent in the current study.33
In addition to mortality, we demonstrated
that the inappropriate use of empirical antibiotics
was associated with longer ICU ventilator duration,
which leads to greater costs and more extensive
use of ICU resources. A large retrospective cohort
from the US regarding Enterobacteriaceae infections
showed that each additional day without appropriate
antibiotics was associated with an increased hospital
expenditure of US$750 and an increased risk of
30-day readmission.36
To the best of our knowledge, the
appropriateness of empirical antibiotics has
consistently been identified as one of the strongest
independent predictors of 90-day mortality in all
affected patients and in critically ill patients.37 38 39
Kumar et al8 demonstrated a fivefold increase in
mortality among patients with sepsis who received
inappropriate initial antibiotics. In this study, we
demonstrated a twofold increase in mortality in all
patients with K pneumoniae bacteraemia, as well as a
threefold increase in mortality in critically ill patients
with K pneumoniae bacteraemia. Furthermore,
receipt of inappropriate initial antibiotics was the
strongest independent predictor of 90-day mortality
in the ICU subgroup. Zilberberg et al40 found that
the detrimental effect of inappropriate empirical antibiotic treatment could not be corrected despite
subsequent targeted antibiotic treatments. A meta-analysis
revealed a slower rate of bacterial clearance
and increased treatment failure rate when patients
were administered inappropriate empirical antibiotic
therapy.41 Appropriate early antibiotics allow rapid
reduction of bacterial load and modulate host
defences, thus alleviating some organ dysfunction.42
A more pragmatic approach would be the early
administration of broader-spectrum empirical
antibiotics and timely de-escalation, according
to bacterial sensitivity and the patient’s clinical
progression.
The chain of sepsis management begins during
the first encounter in the Emergency Department
and in general hospital wards, rather than in the
ICU. Early administration of antibiotics within
3 hours of hospital admission and aggressive sepsis
care (beginning in the Emergency Department)
can improve survival.42 Another prospective
observational study demonstrated that the
adequate use of empirical antibiotics prior to
ICU admission was the strongest independent
factor associated with survival.29 Extensive efforts
are needed to facilitate early, appropriate use of
empirical antibiotics, including the use of a current
antibiogram, implementation of multidisciplinary
sepsis management guidelines, and establishment
of protocols among pharmacists, microbiologists,
clinicians, and nurses.
Strengths
To the best of our knowledge, this is the largest study
of K pneumoniae bacteraemia in Hong Kong and in
the Asia-Pacific region. By including both ICU and
general ward patients, we achieved clarity regarding
the diverse characteristics of K pneumoniae
bacteraemia. We also identified many potential
predictors of K pneumoniae bacteraemia–related
mortality, based on our extensive literature review and
previous publications, then tested these predictors
using real-world patient data. By evaluating 90-day
mortality, hospital LOS, and ventilator duration, our
study more comprehensively evaluated immediate
and longer-term complications of bacteraemia; it
also provided information for future studies of cost-effectiveness
in terms of empirical antibiotics and
resource utilisation. Finally, we used the maximum
total SOFA score for severity assessment. This score
has been repeatedly validated in determining disease
severity and predicting mortality in critically ill
patients.43 44 45
Limitations
This retrospective study was subject to potential confounding factors, including selection bias that
could not be completely eliminated from the analysis. Notably, the results of this single-centre study may
not be generalisable to other countries with higher
CR or CP K pneumoniae infections. Furthermore,
this study encompassed a long duration, in which
the definitions of sepsis or septic shock might have
changed.45 The care of patients with sepsis evolved
over time, including advances in source control by
percutaneous and endoscopic means that potentially
improved patient survival. Nonetheless, the role of
empirical antibiotics in patients with sepsis remains
an essential sepsis consideration.
Antibiotic pharmacodynamics also has a
fundamental role in bacteraemia treatment. In this
study, we could not collect information regarding the
timing of first-dose antibiotics, time to appropriate
antibiotics, duration of antibiotics, or time to surgical
treatments. Moreover, antibiotic stewardship and
therapeutic de-escalation efforts, as well as their
impacts on patient outcomes, were not assessed in
the present study. Future studies may be needed
concerning the prolonged infusion of beta-lactam
antibiotics, use of combination therapies, duration
of antibiotics, and serum monitoring of antibiotics.
Conclusion
The receipt of inappropriate empirical antibiotics led to twofold greater 90-day mortality in patients with
K pneumoniae bacteraemia. In critically ill patients,
inappropriate use of empirical antibiotics was
the strongest independent predictor of mortality.
Early identification of high-risk patients and
administration of appropriate empirical antibiotics
can improve patient outcomes.
Author contributions
Concept or design: MY Man, HP Shum.
Acquisition of data: MY Man, HP Shum.
Analysis or interpretation of data: MY Man, HP Shum.
Drafting of the manuscript: MY Man.
Critical revision of the manuscript for important intellectual content: WW Yan.
Acquisition of data: MY Man, HP Shum.
Analysis or interpretation of data: MY Man, HP Shum.
Drafting of the manuscript: MY Man.
Critical revision of the manuscript for important intellectual content: WW Yan.
All authors read and approved the final manuscript. All authors had full access to the data, contributed to the study, approved the final version for publication, and take responsibility for its accuracy and integrity.
Conflicts of interest
All authors have disclosed no conflicts of interest.
Declaration
This research was presented by KC Li as an abstract at the 31st Annual Congress of the European Society of Intensive Care Medicine (ESICM), 21-24 October 2018, Paris, France.
Funding/support
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Ethics approval
This study was approved by the Hong Kong Easter Cluster Ethics Committee of the Hospital Authority (HKECREC-2018-018). The requirement for written informed consent was
waived because of the retrospective nature of the study.
References
1. Ho PL, Wu TC, Chao DV, et al, editors. Reducing bacterial
resistance with IMPACT. Interhospital multi-disciplinary
programme on antimicrobial chemotherapy. 5th edition.
2017. Available from: https://www.chp.gov.hk/files/pdf/reducing_bacterial_resistance_with_impact.pdf. Accessed
7 Jun 2020.
2. Ben-David D, Kordevani R, Keller N, et al. Outcome of
carbapenem resistant Klebsiella pneumoniae bloodstream
infections. Clin Microbiol Infect 2012;18:54-60. Crossref
3. Wong MH, Shum HP, Chen JH, et al. Emergence
of carbapenem-resistant hypervirulent Klebsiella
pneumoniae. Lancet Infect Dis 2018;18:24. Crossref
4. Man MY, Shum HP, Chan YH, et al. Clinical predictors and outcomes of Klebsiella pneumoniae bacteraemia in a
regional hospital in Hong Kong. J Hosp Infect 2017;97:35-41.Crossref
5. Alicino C, Giacobbe DR, Orsi A, et al. Trends in the annual
incidence of carbapenem-resistant Klebsiella pneumoniae
bloodstream infections: a 8-year retrospective study in a
large teaching hospital in northern Italy. BMC Infect Dis
2015;15:415. Crossref
6. Rhodes A, Evans LE, Alhazzani W, et al. Surviving sepsis
campaign: international guidelines for management
of sepsis and septic shock: 2016. Intensive Care Med
2017;43:304-77.Crossref
7. Ferreira FL, Bota DP, Bross A, Mélot C, Vincent JL. Serial evaluation of the SOFA score to predict outcome in
critically ill patients. JAMA 2001;286:1754-8. Crossref
8. Kumar A, Ellis P, Arabi Y, et al. Initiation of inappropriate
antimicrobial therapy results in a fivefold reduction of
survival in human septic shock. Chest 2009;136:1237-48. Crossref
9. Vazquez-Guillamet C, Scolari M, Zilberberg MD, Shorr AF,
Micek ST, Kollef M. Using the number needed to treat to
assess appropriate antimicrobial therapy as a determinant
of outcome in severe sepsis and septic shock. Crit Care
Med 2014;42:2342-9. Crossref
10. Micek ST, Welch EC, Khan J, et al. Empiric combination
antibiotic therapy is associated with improved outcome
against sepsis due to Gram-negative bacteria: a
retrospective analysis. Antimicrob Agents Chemother
2010;54:1742-8. Crossref
11. Juan CH, Chuang C, Chen CH, Li L, Lin YT. Clinical
characteristics, antimicrobial resistance and capsular
types of community-acquired, healthcare-associated,
and nosocomial Klebsiella pneumoniae bacteremia.
Antimicrob Resist Infect Control 2019;8:1. Crossref
12. Clinical and Laboratory Standards Institute. M100-S16
Performance Standards for Antimicrobial Susceptibility
Testing; Sixteenth Informational Supplement. Clinical and
Laboratory Standards Institute, Wayne, PA; January 2006.
13. Clinical and Laboratory Standards Institute. M100-S17
Performance Standards for antimicrobial susceptibility
testing; Seventeenth Informational Supplement. Clinical
and Laboratory Standards Institute, Wayne, PA; January
2007.
14. Clinical and Laboratory Standards Institute. M100-S19
Performance Standards for antimicrobial susceptibility
testing; Nineteenth Informational Supplement. Clinical and
Laboratory Standards Institute, Wayne, PA; January 2009.
15. Clinical and Laboratory Standards Institute. M100-S20
Performance Standards for Antimicrobial Susceptibility
Testing; Twentieth Informational Supplement. Clinical and
Laboratory Standards Institute, Wayne, PA; January 2010.
16. Clinical and Laboratory Standards Institute. M100-S23
Performance Standards for Antimicrobial Susceptibility
Testing; Twenty-Third Informational Supplement. Clinical
and Laboratory Standards Institute, Wayne, PA; January
2013.
17. Clinical and Laboratory Standards Institute. M100-S25
Performance Standards for Antimicrobial Susceptibility
Testing; Twenty-Fifth Informational Supplement. Clinical
and Laboratory Standards Institute, Wayne, PA; January
2015.
18. Clinical and Laboratory Standards Institute. M100-S26
Performance Standards for Antimicrobial Susceptibility
Testing; Twenty-Sixth Informational Supplement. Clinical
and Laboratory Standards Institute, Wayne, PA; January
2016.
19. Jarlier V, Nicolas MH, Fournier G, Philippon A.
Extended broad-spectrum beta-lactamases conferring
transferable resistance to newer beta-lactam agents in
Enterobacteriaceae: hospital prevalence and susceptibility
patterns. Rev Infect Dis 1988;10:867-78. Crossref
20. Micek ST, Hampton N, Kollef M. Risk factors and outcomes
for ineffective empiric treatment of sepsis caused by Gram-negative
pathogens: stratification by onset of infection.
Antimicrob Agents Chemother 2017;62:e01577-17.
21. Lautenbach E, Patel JB, Bilker WB, Edelstein PH, Fishman
NO. Extended-spectrum beta-lactamase-producing
Escherichia coli and Klebsiella pneumoniae: risk factors for
infection and impact of resistance on outcomes. Clin Infect
Dis 2001;32:1162-71. Crossref
22. Eilertson B, Cober E, Richter SS, et al. Carbapenem-resistant
Enterobacteriaceae infections in patients on
renal replacement therapy. Open Forum Infect Dis
2017;4:ofx216.
23. Tian L, Tan R, Chen Y, et al. Epidemiology of Klebsiella
pneumoniae bloodstream infections in a teaching hospital:
factors related to the carbapenem resistance and patient
mortality. Antimicrob Resist Infect Control 2016;5:48. Crossref
24. Pau CK, Ma FF, Ip M, You JH. Characteristics and
outcomes of Klebsiella pneumoniae bacteraemia in Hong
Kong. Infect Dis (Lond) 2015;47:283-8. Crossref
25. Li L, Huang H. Risk factors of mortality in bloodstream
infections caused by Klebsiella pneumonia: a singlecenter
retrospective study in China. Medicine (Baltimore)
2017;96:e7924.
26. Melot B, Colot J, Guerrier G. Bacteremic community-acquired
infections due to Klebsiella pneumoniae: clinical
and microbiological presentation in New Caledonia, 2008-2013. Int J Infect Dis 2015;41:29-31. Crossref
27. Russo A, Falcone M, Gutiérrez-Gutiérrez B, et al. Predictors
of outcome in patients with severe sepsis or septic shock
due to extended-spectrum beta-lactamase-producing
Enterobacteriaceae. Int J Antimicrob Agents 2018;52:577-85.Crossref
28. Zilberberg MD, Shorr AF, Micek ST, Vazquez-Guillamet C,
Kollef MH. Multi-drug resistance, inappropriate initial antibiotic therapy and mortality in Gram-negative severe
sepsis and septic shock: a retrospective cohort study. Crit
Care 2014;18:596. Crossref
29. Garnacho-Montero J, Gutiérrez-Pizarraya A, Escoresca-Ortega A, Fernández-Delgado E, López-Sánchez JM.
Adequate antibiotic therapy prior to ICU admission
in patients with severe sepsis and septic shock reduces
hospital mortality. Crit Care 2015;19:302. Crossref
30. Antonio M, Gudiol C, Royo-Cebrecos C, Grillo S,
Ardanuy C, Carratalà J. Current etiology, clinical features
and outcomes of bacteremia in older patients with solid
tumors. J Geriatr Oncol 2019;10:246-51. Crossref
31. Tseng CP, Wu HS, Wu TH, Lin YT, Fung CP. Clinical
characteristics and outcome of patients with community-onset
Klebsiella pneumoniae bacteremia requiring
intensive care. J Microbiol Immunol Infect 2013;46:217-23. Crossref
32. Peralta G, Sánchez MB, Roiz MP, Garrido JC, Teira R,
Mateos F. Diabetes does not affect outcome in patients with
Enterobacteriaceae bacteremia. BMC Infect Dis 2009;9:94. Crossref
33. Filsoufi F, Rahmanian PB, Castillo JG, Mechanick JI,
Sharma SK, Adams DH. Diabetes is not a risk factor for
hospital mortality following contemporary coronary
artery bypass grafting. Interact Cardiovasc Thorac Surg
2007;6:753-8. Crossref
34. Teo BJ, Chong HC, Yeo W, Tan AH. The impact of diabetes
on patient outcomes after total knee arthroplasty in an
Asian population. J Arthroplasty 2018;33:3186-9. Crossref
35. Stegenga ME, Vincent JL, Vail GM, et al. Diabetes does not
alter mortality or hemostatic and inflammatory responses
in patients with severe sepsis. Crit Care Med 2010;38:539-45. Crossref
36. Zilberberg MD, Nathanson BH, Sulham K, Fan W, Shorr AF.
30-day readmission, antibiotics costs and costs of delay
to adequate treatment of Enterobacteriaceae UTI,
pneumonia, and sepsis: a retrospective cohort study.
Antimicrob Resist Infect Control 2017;6:124. Crossref
37. Gutiérrez-Gutiérrez B, Salamanca E, de Cueto M, et al. Effect of appropriate combination therapy on
mortality of patients with bloodstream infections
due to carbapenemase-producing Enterobacteriaceae
(INCREMENT): a retrospective cohort study. Lancet
Infect Dis 2017;17:726-34. Crossref
38. Cheng WL, Hsueh PR, Lee CC, et al. Bacteremic
pneumonia caused by extended-spectrum beta-lactamase-producing
Escherichia coli and Klebsiella pneumoniae:
appropriateness of empirical treatment matters. J
Microbiol Immunol Infect 2016;49:208-15. Crossref
39. Kohler PP, Volling C, Green K, Uleryk EM, Shah PS,
McGeer A. Carbapenem resistance, initial antibiotic
therapy, and mortality in Klebsiella pneumoniae
bacteremia: a systematic review and meta-analysis. Infect
Control Hosp Epidemiol 2017;38:1319-28. Crossref
40. Zilberberg MD, Shorr AF, Micek ST, Mody SH, Kollef MH.
Antimicrobial therapy escalation and hospital mortality
among patients with health-care-associated pneumonia: a
single-center experience. Chest 2008;134:963-8. Crossref
41. Raman G, Avendano E, Berger S, Menon V. Appropriate
initial antibiotic therapy in hospitalized patients with
gram-negative infections: systematic review and meta-analysis.
BMC Infect Dis 2015;15:395. Crossref
42. Seymour CW, Gesten F, Prescott HC, et al. Time to
treatment and mortality during mandated emergency care
for sepsis. N Engl J Med 2017;376:2235-44. Crossref
43. Moreno R, Vincent JL, Matos R, et al. The use of maximum
SOFA score to quantify organ dysfunction/failure in
intensive care. Results of a prospective, multicentre study.
Working Group on Sepsis related Problems of the ESICM.
Intensive Care Med 1999;25:686-96. Crossref
44. Minne L, Abu-Hanna A, de Jonge E. Evaluation of SOFA-based
models for predicting mortality in the ICU: a
systematic review. Crit Care 2008;12:R161.
45. Singer M, Deutschman CS, Seymour CW, et al. The third
international consensus definitions for sepsis and septic
shock (sepsis-3). JAMA 2016;315:801-10. Crossref