© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
REMINISCENCE: ARTEFACTS FROM THE HONG KONG MUSEUM OF
MEDICAL SCIENCES
Electroconvulsive therapy machine
HK Cheung, FRCPsych (UK), Hon FHKCPsych
Guest author, Education and Research Committee, Hong Kong Museum of Medical Sciences Society
Electroconvulsive therapy (ECT) is a psychiatric
treatment in which seizure is electrically induced
in patients, typically with muscular convulsions
subdued by muscle relaxant and anaesthesia. This
ECT machine was generously donated to the Hong
Kong Museum of Medical Sciences by Dr John
Chung, son of the late Dr Cho-man Chung (Fig).
The ECT machine is an Ectonus Mark 3 model
manufactured by Ectron Ltd.
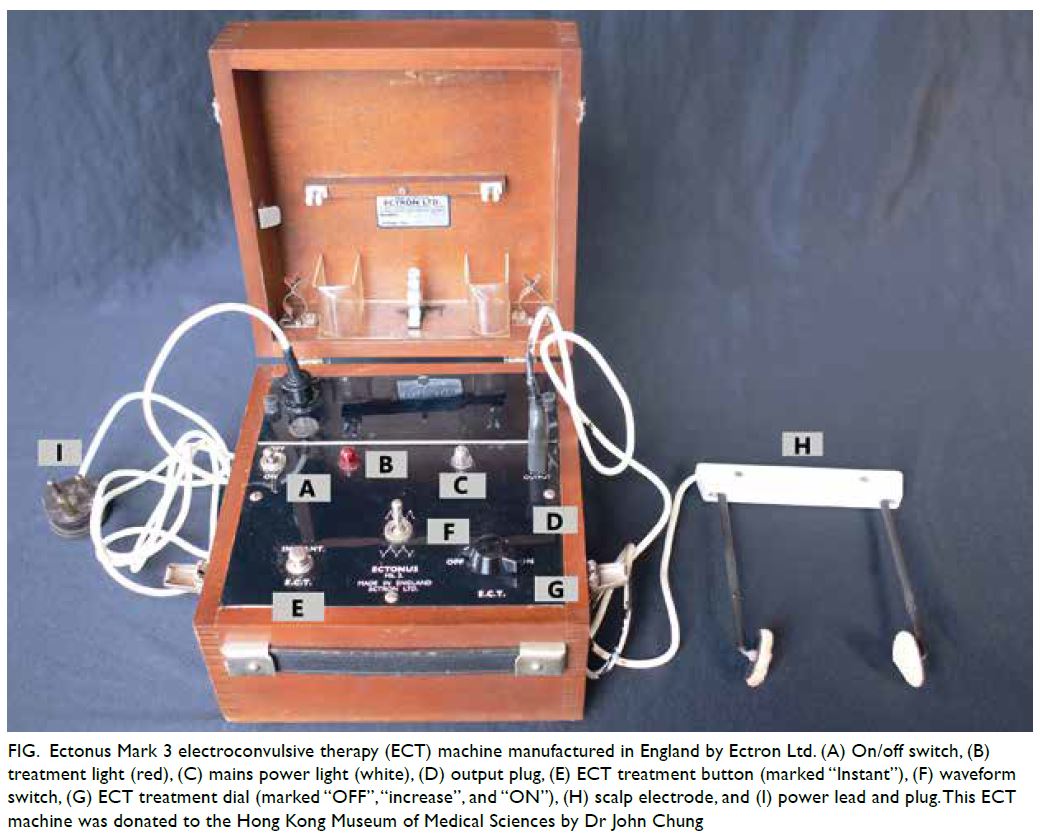
Figure. Ectonus Mark 3 electroconvulsive therapy (ECT) machine manufactured in England by Ectron Ltd. (A) On/off switch, (B) treatment light (red), (C) mains power light (white), (D) output plug, (E) ECT treatment button (marked “Instant”), (F) waveform switch, (G) ECT treatment dial (marked “OFF”, “increase”, and “ON”), (H) scalp electrode, and (I) power lead and plug. This ECT machine was donated to the Hong Kong Museum of Medical Sciences by Dr John Chung
Convulsive therapy was first introduced in
1934 by Ladislas Joseph Meduna, a Hungarian
neuropsychiatrist who believed that schizophrenia
and epilepsy were antagonistic disorders. He induced
seizures first with camphor and then metrazol. In
1938, Ugo Cerletti, an Italian neuropsychiatrist and
his assistant Lucio Bini developed the idea of using
electricity as a substitute for metrazol in convulsive
therapy.1 Soon, ECT replaced metrazol therapy
worldwide, and Cerletti and his assistant Lucio Bini were nominated for a Nobel Prize. Later, the two
Italian inventors had a disagreement over the patent
of the ECT device, damaging their relationship.
Since the original Cerletti–Bini ECT apparatus,
there have been continuous modifications and
refinements in the ECT machines. All modifications
have had the same goal of maximising therapeutic
effect while minimising adverse consequences
(mainly confusion and amnesia). Many parameters
have been considered, including waveform, pulse
width, resistance (constant voltage or constant
current), electric charge, electrodes (unilateral
or bilateral), and dose (titration or fixed). In
addition, modern machines have added capabilities
to monitor physiological parameters such as
electroencephalogram, electrocardiogram, blood
oxygen level, and motion, as well as software that can
provide the clinician with detailed monitoring and
feedback.
In the 1940s, ECT was given in “unmodified”
form—without muscle relaxants—resulting in a fullscale
convulsive seizure, and sometimes inflicting
injury to the patient, including (rarely) fracture or
dislocation of the long bones. In order to modify
the convulsions, psychiatrists began to experiment
with curare, a poison from South America.
Unmodified ECT was introduced to Hong Kong in
the 1940s. Known colloquially as “straight ECT”,
it was performed by a psychiatrist without the use
of anaesthesia, muscle relaxant, or any machine-provided
physiological monitoring, and often
without proper informed consent from the patient.
In 1951, the introduction of suxamethonium
(succinylcholine), a safer synthetic alternative to
curare, led to the more widespread use of modified
ECT. Anaesthetics are unnecessary for ECT, as the
electric shock is capable of immediately rendering
the patient unconscious. Moreover, ECT can cause
retrograde amnesia, so the patient also has no
negative memory of the experience. Nevertheless,
muscle relaxants can invoke a feeling of suffocation,
so a short-acting anaesthetic was usually given in
addition to the muscle relaxant in order to spare the
patients this terrifying ordeal.
In the United States, ECT devices are
manufactured by two companies, Somatics and
MECTA. In the United Kingdom, the market for
ECT devices was long monopolised by Ectron Ltd.
In Hong Kong, following the British medical training
and tradition, Ectron machines were the only ones in
use for >50 years. It was not until the past 20 years
that non-British models were introduced into Hong
Kong.
The Ectonus Mark 3 ECT apparatus at the
Hong Kong Museum of Medical Sciences was one
of the first-generation models manufactured by
Ectron Ltd. The apparatus was housed in a square
wooden box with a lid that is hinged at the back, has
two clasps on the left and right sides near the front
and an attached leather handle on the front; the base
houses the motor of the apparatus and is covered
with a panel that with an on/off switch, an ECT
treatment button, a waveform switch, and an ECT
treatment dial, as well as various connectors and
indicator lights (Fig). At the time the apparatus was
manufactured and used, likely in the 1960s, current
would have been delivered in sine-wave form, with
a switch allowing the clinician to choose between
unidirectional or bidirectional sine waves. At that
time, it was believed that the unidirectional wave
produced fewer adverse effects but the bidirectional wave was more effective. A fixed dose of electricity
predetermined by the manufacturer could be
delivered by pressing a separate treatment button
(labelled “instant”). Alternatively, the operator
could choose to deliver a dose of variable strength
and/or duration by using the treatment dial. No
physiological monitoring or other software was
provided by the machine.
Despite improvements in technique and
equipment, the use of ECT declined from the 1950s
owing to declining public acceptance influenced
by negative depictions of ECT in the mass media,
as well as the emergence of alternative treatments.
Modern psychopharmacotherapy, including
effective antidepressants, antipsychotics, mood
stabilisers, tranquillisers, rendered ECT unnecessary
in most cases. There are also less-invasive cerebral
modulation interventions, such as repetitive
transcranial magnetic stimulation, which, although
not as effective as ECT, is acceptable to doctor
and patient because it does not require general
anaesthesia nor the induction of a seizure.
In Hong Kong, until the late 1970s, all ECT
procedures (including the general anaesthesia)
were carried out by psychiatrists. Typically, two
psychiatrists worked as a team, treating tens of
patients daily, with multiple ECT procedures each
hour. After this, anaesthetists participated in the
treatment. By the 2000s, taking the figures of Castle
Peak Hospital as an illustration, ECT was performed
in only two sessions per week, with one psychiatrist
and one anaesthetist. Typically only one or two
patients were treated per session, with no patients at
all in some sessions.
A modern course of ECT usually consists
of four to 12 treatments delivered 2 to 3 times per
week. Neuroimaging studies in people who have had
ECT, investigating differences between responders
and non-responders, find that responders have
decreased blood flow and metabolism in the frontal
lobes, and increased perfusion and metabolism in the
medial temporal lobe (such as the hippocampus).2
The general physical risks (and mortality) of ECT
are similar to those of a brief general anaesthesia.
The most common adverse effects are confusion
and transient memory loss. It is safe in pregnancy.
Despite the decline in use, ECT remains an
important backup treatment for patients with major
depressive disorder and other mental disorders,
including mania, catatonia, and treatment-resistant
schizophrenia, in whom other therapies have proved
ineffective.
References
1. Cerletti U. Electroshock therapy. In: Marti-Ibanez F, Sackler AM, Sackler MD, Sackler RR, editors. The Great
Physiodynamic Therapies in Psychiatry: an Historical Reappraisal. New York: Hoeber-Harper; 1956: 91-120.
2. Abbott CC, Gallegos P, Rediske N, Lemke NT, Quinn DK. A review of longitudinal electroconvulsive therapy:
neuroimaging investigations. J Geriatr Psychiatry Neurol 2014;27:33-46. Crossref

