Hong
Kong Med J 2021 Jun;27(3):222.e1–2
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
PICTORIAL MEDICINE
Tattoo-associated uveitis
CY Mak, MB, BS, MRCSEd (Ophth)1; Mary Ho, FCOphth HK, FHKAM (Ophthalmology)1; Angela Z Chan, MB, BS2; Lawrence PL Iu, FRCSEd (Ophth), FHKAM (Ophthalmology)1; Christina MT Cheung, FHKCP, FHKAM (Medicine)3; Marten E Brelen, BMBCh (Oxon), FRCOphth1; Paul CL Choi, FRCPA, FHKAM (Pathology)2; Alvin L Young, FRCOphth, FHKAM (Ophthalmology)1
1 Department of Ophthalmology and Visual Sciences, Prince of Wales Hospital, Hong Kong
2 Department of Anatomical and Cellular Pathology, Prince of Wales Hospital, Hong Kong
3 Division of Dermatology, Department of Medicine and Therapeutics, Prince of Wales Hospital, Hong Kong
Corresponding author: Prof Alvin L Young (youngla@ha.org.hk)
A 19-year-old man with extensive body tattooing
presented with recurrent episodes of reduced vision,
bilateral photophobia and concomitant swelling of
body tattoos. He had multiple tattoos over his entire
body with mainly black pigment and occasional red
and yellow pigment, performed over a period of 3
years prior to the presentation of ocular symptoms.
He enjoyed good past health with no history of
autoimmune diseases. There was no joint pain, skin
rash or chest symptoms.
Ophthalmological examination revealed
bilateral injection, anterior chamber cells, posterior
synechiae (Fig 1) and marked vitritis, consistent
with anterior and intermediate uveitis. There were
no mutton-fat keratic precipitates or iris nodules.
Presenting visual acuity was 20/200 in both eyes.
Dermatological examination showed prominent
induration of skin with mild tenderness in areas
of body tattoo containing black pigment (Fig 2).
Non-tattooed skin was unremarkable with no signs
of inflammation. Incisional skin biopsy was taken
from an area of prominently indurated tattoo.
Histopathology showed marked non-caseating
granulomatous reaction within the dermis and
abundant black pigment deposition (Fig 3). Periodic
acid-Schiff staining showed no fungal elements. Chest
radiograph was clear with no hilar lymphadenopathy
and interferon-gamma releasing assay was negative.
Syphilis and human immunodeficiency virus serology
was negative. Immune markers including antinuclear antibodies, antineutrophil cytoplasmic antibodies
and anti-extractable nuclear antigens antibody
were negative. The patient declined a blood test for
angiotensin-converting enzyme level due to the
associated cost. Serum calcium was not elevated.
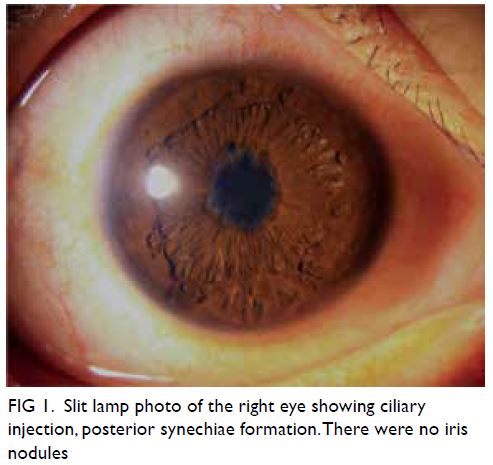
Figure 1. Slit lamp photo of the right eye showing ciliary injection, posterior synechiae formation. There were no iris nodules

Figure 2. Prominent induration of part of a tattoo containing black pigment. Surrounding non-tattooed skin was unremarkable
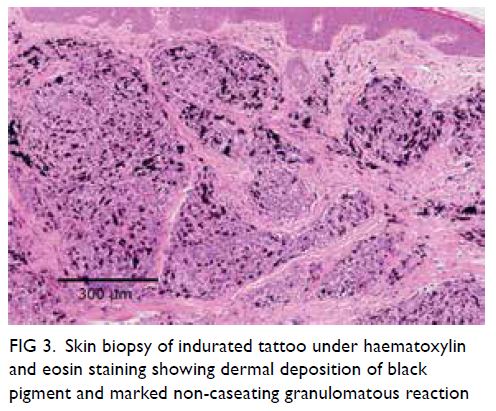
Figure 3. Skin biopsy of indurated tattoo under haematoxylin and eosin staining showing dermal deposition of black pigment and marked non-caseating granulomatous reaction
He was treated with topical prednisolone and
oral prednisolone 60 mg daily after exclusion of
infectious uveitides. Body tattoo swelling subsided
rapidly after systemic steroid and the uveitis was
brought under control gradually with significant improvement in bilateral vision. He was maintained
on mycophenolate mofetil 1g twice a day as a steroid-sparing
agent for uveitis control. His oral prednisolone
was tapered to below 15 mg daily. His visual acuity
improved and maintained at 20/30 bilaterally. There
were no features of systemic sarcoidosis. Overall
clinicopathological features were compatible
with tattoo-associated uveitis, a rare dermato-ophthalmological
complication of body tattooing.
Systemic sarcoidosis, a rare disease in Asians,
can occasionally cause tattoo granuloma and
uveitis.1 Tattoo-associated uveitis without systemic
sarcoidosis is a rare entity first described in a case
series half a century ago.2 The disease is characterised
by recurrent episodes of uveitis in conjunction
with raised and indurated tattoo, while histology
of affected skin demonstrates florid non-caseating
granulomatous reaction indistinguishable from
tattoo granuloma in systemic sarcoidosis.3 The exact
pathogenesis is unknown, but it was believed to be
a type of delayed hypersensitivity reaction to tattoo
pigments.3 Treatment is mainly to control ocular
inflammation by topical and systemic steroid, with
or without steroid-sparing agent. Tattoo excision has
been reported to be useful in limiting recurrences.1 3
However, the extensive tattoo involvement in our
patient rendered excision impractical.
In summary, the clinical photos illustrate a rare
case of tattoo-associated uveitis, highlighting the
importance of inquiry into tattoo history and skin
examination of tattoos in a patient with recurrent
uveitis.
Author contributions
Concept or design: CY Mak, ME Brelen, AL Young.
Acquisition of data: CY Mak, AZ Chan, CMT Cheung.
Analysis or interpretation of data: CY Mak, M Ho, LPL Iu, PCL Choi.
Drafting of the manuscript: CY Mak, M Ho, AZ Chan.
Critical revision of the manuscript for important intellectual content: All authors.
Acquisition of data: CY Mak, AZ Chan, CMT Cheung.
Analysis or interpretation of data: CY Mak, M Ho, LPL Iu, PCL Choi.
Drafting of the manuscript: CY Mak, M Ho, AZ Chan.
Critical revision of the manuscript for important intellectual content: All authors.
All authors had full access to the data, contributed to the study, approved the final version for publication, and take
responsibility for its accuracy and integrity.
Conflicts of interest
All authors have disclosed no conflicts of interest.
Funding/support
This pictorial medicine paper received no specific grant from any funding agency in the public, commercial, or not-forprofit
sectors.
Ethics approval
This patient was treated in accordance with the Declaration of Helsinki. The patient provided written informed consent for
all treatments and procedures and for publication of clinical
photos.
References
1. Kluger N. Tattoo-associated uveitis with or without systemic sarcoidosis: a comparative review of the
literature. J Eur Acad Dermatol Venereol 2018;32:1852-61. Crossref
2. Rorsman H, Brehmer-Andersson E, Dahlquist I, et al. Tattoo granuloma and uveitis. Lancet 1969;2:27-8. Crossref
3. Ostheimer TA, Burkholder BM, Leung TG, Butler NJ, Dunn JP, Thorne JE. Tattoo-associated uveitis. Am J
Ophthalmol 2014;158:637-43.e1. Crossref

