Hong Kong Med J 2021 Apr;27(2):148–9 | Epub 7 Apr 2021
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
COMMENTARY
Formulation of a departmental COVID-19
contingency plan for contact tracing and facilities management
ST Mak, FRCSEd (Ophth), FHKAM (Ophthalmology)1,2,3; Kitty SC Fung, FHKAM (Pathology)4; Kenneth KW Li, FRCOphth, FHKAM (Ophthalmology)1,2
1 Department of Ophthalmology, United Christian Hospital, Hong Kong
2 Department of Ophthalmology, Tseung Kwan O Hospital, Hong Kong
3 Quality and Safety Office, Kowloon East Cluster, Hospital Authority, Hong Kong
4 Department of Pathology, United Christian Hospital, Kwun Tong, Hong Kong
Corresponding author: Dr ST Mak (dr.makst@gmail.com)
In February 2020, the ophthalmology unit of Kowloon
East Cluster, in collaboration with the infection
control team, formulated this contingency plan with
a main aim of facilitating the contact tracing of staff
and patients to control the spread of coronavirus
disease 2019 (COVID-19).1 The plan also provided
guidance to our staff on facilities management.
Contact tracing
We followed the definition of contacts described
by the Chief Infection Control Officer Office of the
Hospital Authority of Hong Kong. Contact tracing
was conducted for all staff identified as a ‘close
contact’ or a ‘probable case’. ‘Close contacts’ were
defined as healthcare workers who had cared for
patient with confirmed COVID-19 (ie, within 14 days
[the incubation period of COVID-192] of symptom
onset or the date of diagnosis for asymptomatic
patients) without wearing appropriate personal
protective equipment (PPE). Appropriate PPE was
considered as surgical masks for routine patient
handling in the ophthalmology setting, or full
PPE including N95 respirators and face shields for
aerosol-generating procedures, such those involving
the use of transnasal drills or cautery.3 Staff who
developed fever or respiratory symptoms after
exposure to a patient with COVID-19 were managed
as ‘probable cases’. In case of doubt, the exposure
situation was discussed with the Chief Infection Control Officer Office of the Hospital Authority or the Centre of Health Protection.
In United Christian Hospital, Hong Kong,
allocation of patients to consultation rooms is
managed using proprietary in-house computer
software called ‘UQ Web’. The system allows
tracking of patient movement among the different
consultation rooms, facilitating tracing of doctors,
nursing staff, and allied health workers who had come
into contact with patients later confirmed to have
COVID-19. The system can also generate a list of
patients who attended the same consultation room, allowing for contact tracing. Identified patients are
informed individually and advised to report any
relevant symptoms. In-patients are monitored by
the hospital infection control team and out-patients
are monitored by the Centre for Health Protection.
The risk assessment depends on the duration, proper
wearing of a surgical mask, and the closeness of
contact with the patient with confirmed COVID-19
during the exposure. (Fig)
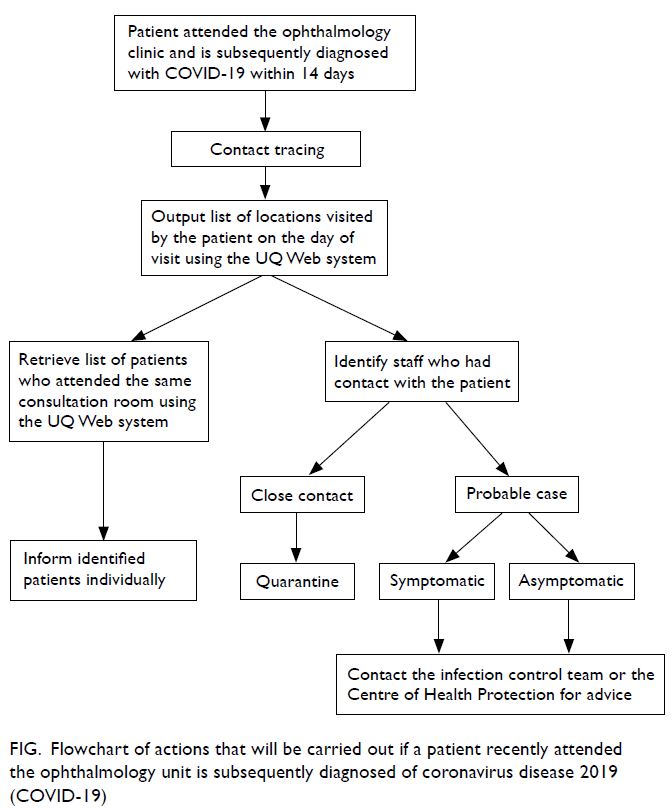
Figure. Flowchart of actions that will be carried out if a patient recently attended the ophthalmology unit is subsequently diagnosed of coronavirus disease 2019 (COVID-19)
In addition, the contingency plan considers
facilities management. Patients with confirmed
COVID-19 requiring urgent ophthalmology
attendance are arranged as the final scheduled
appointment of the day, to minimise service
disruption, if possible. The patients are examined in
a designated room with a high-efficiency particulate
air filtration system capable of capturing sub-micron
particulate as small as 0.1 μm.4 All staff assessing
the patients wear appropriate PPE. The consultation
room and all instruments are disinfected with 1:49
diluted bleach or 70% alcohol, respectively. The room
is vacated for 48 hours, taking reference from the
hospital’s practice of operating theatre air sampling.
With six air changes per hour in general hospital
setting, a minimum of 69 minutes is adequate to
remove 99.9% of airborne contaminants. The plan
also includes contingency for backup rooms. For
example, our clinic has two investigation rooms for
checking visual acuity and intraocular pressure. All
tests were conducted in one room, and if it had to
be closed for terminal disinfection, the other room
could be used.
Split teams
The majority of healthcare activities require direct
patient contact, and most staff cannot work from
home. In anticipation of the need for quarantine or
isolation of our staff, our department implemented
a split team arrangement to ensure adequate
manpower at all times. In this arrangement, staff were allocated to teams that worked on alternate
work sites or work schedules. The teams were
physically segregated to minimise exposure and
cross-contamination, reducing potential disruption
to patient care. Because our team serves two hospitals
(United Christian Hospital and Tseung Kwan O
Hospital), our doctors routinely visit both hospitals,
sometimes on the same day. Administrative staff also
provide clerical support to the eye clinics of both
hospitals. To achieve split teams, our administrative
staff were split into two teams with each working in
one hospital only. During the peak of the COVID-19
outbreak in February 2020, administrative staff
worked from home. We also considered splitting
our doctors to work at one hospital only without
the need to provide service at both hospitals. This
split team arrangement for doctors and allied health
staff was successfully implemented in August and
September 2020, and December 2020 to February 2021.
Conclusion
We have regularly updated the contingency plan to reflect the latest available scientific evidence on
COVID-19. This system has been used for tracing
patients 3 times, with approximately 40 patients
successfully traced each time. We encourage fellow
departments and clinics to develop their own
contingency plans to prepare for the next wave of
COVID-19 or other future outbreaks or epidemics.
Author contributions
Concept or design: All authors.
Acquisition of data: ST Mak, KKW Li.
Analysis or interpretation of data: ST Mak, KKW Li.
Drafting of the manuscript: ST Mak, KKW Li.
Critical revision of the manuscript for important intellectual content: All authors.
Acquisition of data: ST Mak, KKW Li.
Analysis or interpretation of data: ST Mak, KKW Li.
Drafting of the manuscript: ST Mak, KKW Li.
Critical revision of the manuscript for important intellectual content: All authors.
All authors had full access to the data, contributed to the study, approved the final version for publication, and take responsibility for its accuracy and integrity.
Conflicts of interest
As an editor of the journal, KKW Li was not involved in the
peer review process. The other authors have no conflicts of
interest to disclose.
Funding/support
This commentary received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
References
1. Hellewell J, Abbott S, Gimma A, et al. Feasibility of
controlling COVID-19 outbreaks by isolation of cases and
contacts. Lancet Glo Health 2020;8:e488-96. Crossref
2. Linton NM, Kobayashi T, Yang Y, et al. Incubation period
and other epidemiological characteristics of 2019 novel
coronavirus infections with right truncation: a statistical
analysis of publicly available case data. J Clin Med 2020
17;9:538. Crossref
3. Workman AD, Jafari A, Welling DB, et al. Airborne aerosol
generation during endonasal procedures in the Era of
COVID-19: risks and recommendations. Otolaryngol
Head Neck Surg 2020 May 26. Epub ahead of print. Crossref
4. Perry JL, Agui JH, Vigayakumar R. Submicron and
nanoparticulate matter removal by HEPA-rated media
filters and packed beds of granular materials. NASA
technical report 2016: NASA/TM-2016-218224,
M-1414. Available from: https://ntrs.nasa.gov/search.
jsp?R=20170005166. Accessed 2 Jul 2020.

