Hong
Kong Med J 2021 Feb;27(1):58–9.e1–2
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
PICTORIAL MEDICINE
Popliteal artery entrapment syndrome: a rare
diagnosis for calf pain
Stephanie C Woo, MB, BS, FRCR; TS Chan, FHKCR, FHKAM (Radiology); NY Pan, FHKCR, FHKAM (Radiology); Johnny KF Ma, FRCR (UK), FHKAM (Radiology)
Department of Radiology, Princess Margaret Hospital, Hong Kong
Corresponding author: Dr SC Woo (stephaniecheriwoo@gmail.com)
An 18-year-old man presented with a long history
of occasional right calf pain and fullness. He also
complained that over the last year his right foot
An 18-year-old man presented with a long history
of occasional right calf pain and fullness. He also
complained that over the last year his right foot became pale and numb after exercising for few
minutes. There was no history of trauma and the
patient had no constitutional symptoms. On physical
examination, the right calf was non-tender with no
mass although right posterior tibial and dorsalis
pedis pulses were weaker than the left. Radiograph
of the right knee showed static right proximal
tibial exostosis, which had been monitored since
the patient was aged 10 years. Magnetic resonance
arteriogram showed almost complete occlusion
of the right popliteal artery and distal superficial
femoral artery at the level of the right popliteal
fossa (Fig 1). Collateral branches were seen feeding
the distal right leg arteries trifurcation. Magnetic
resonance imaging scan of the knee revealed the
medial head of the gastrocnemius inserting at a
more lateral position than usual (Fig 2). The popliteal
artery was separated from the popliteal vein, passing
medial to and underneath the medial head of
the gastrocnemius, and was severely compressed
between the medial head of the gastrocnemius and
distal femur. Loss of normal flow-related signal void
was noted in the right popliteal artery distal to the
compression.
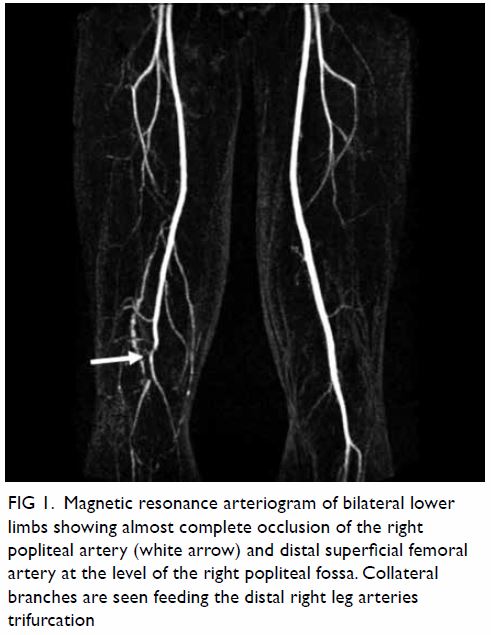
Figure 1. Magnetic resonance arteriogram of bilateral lower limbs showing almost complete occlusion of the right popliteal artery (white arrow) and distal superficial femoral artery at the level of the right popliteal fossa. Collateral branches are seen feeding the distal right leg arteries trifurcation
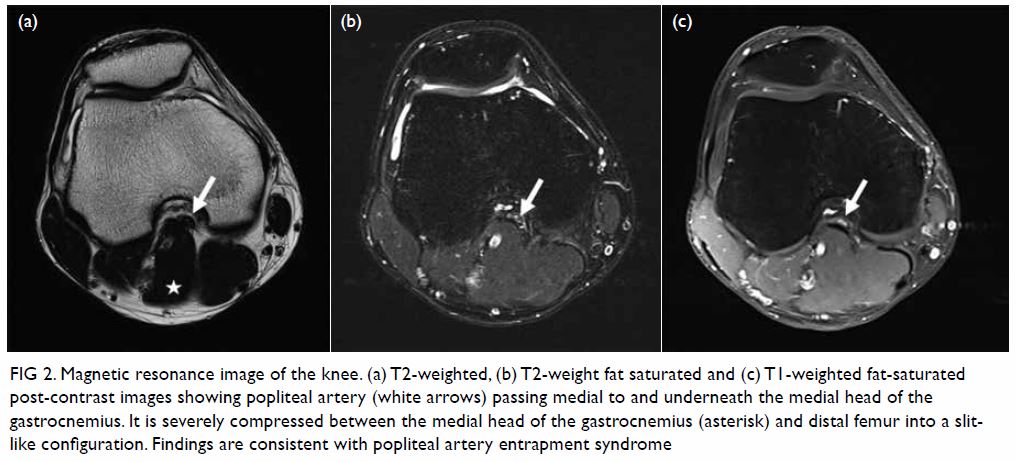
Figure 2. Magnetic resonance image of the knee. (a) T2-weighted, (b) T2-weight fat saturated and (c) T1-weighted fat-saturated post-contrast images showing popliteal artery (white arrows) passing medial to and underneath the medial head of the gastrocnemius. It is severely compressed between the medial head of the gastrocnemius (asterisk) and distal femur into a slitlike configuration. Findings are consistent with popliteal artery entrapment syndrome
Popliteal artery entrapment syndrome (PAES)
is a rare1 and frequently underdiagnosed disease
entity. It typically affects young male athletes who
commonly have hypertrophied musculature without
significant cardiovascular risk factors. The classic presentation of PAES is of symptoms related to
vascular compression, which is intermittent lower
limb claudication. Other symptoms can include
numbness, pain, discoloration, or even paralysis.2
Symptoms in the early stages typically occur during
or following physical activity but can progress to
symptoms at rest if complications develop.
In addition to a careful history, proper physical
examination aids in diagnosis. Usual findings include
calf muscle hypertrophy,2 and reduced posterior tibial
and dorsalis pedis pulses on passive dorsiflexion or
active plantar flexion of the foot.3 In addition, resting
ankle-brachial index tests will usually be normal
but will show a decrease with exercise.4 Differential
diagnoses include other vascular diseases such as
atherosclerosis, exertional syndrome, and cystic
adventitial disease. Further diagnostic testing is
usually needed to make a confident diagnosis of PAES.
Doppler ultrasonography is one of the first-line
imaging modalities. It may demonstrate popliteal
artery stenosis, increased velocity, or reduced peak
systolic velocity during stress manoeuvres. However,
it plays a limited role since imaging findings with
this modality are non-specific and show only the
consequences of the abnormal anatomy.4
Conventional angiography has been long used
for the diagnosis of PAES.1 Typical findings include
medial deviation of the proximal segment, occlusion
in the middle segment, and post-stenotic dilatation
at the distal segment.5 However, it is invasive and
is unable to demonstrate surrounding soft tissue
structures leading to the occlusion of the popliteal
artery. It has recently been replaced by diagnostic
modalities that are non-invasive such as computed
tomography angiography and magnetic resonance
imaging with magnetic resonance arteriogram.
Computed tomography angiography offers
good soft tissue contrast and can provide diagnostic
evaluation of surrounding muscular anomalies.4 It
may also be used to evaluate the contralateral limb
to exclude bilateral entrapment.
Magnetic resonance imaging and MR
angiography are promising imaging modalities
for the diagnosis of PAES6 due to their superior
capability to demonstrate surrounding anatomy and
soft tissue compared with computed tomography
angiography, with no ionising radiation required.
In this case, timely diagnosis was made and
treatment given. However, delay in diagnosis and
management may lead to irreversible effects of lower
limb ischaemia. This case illustrates the importance
of considering this rare diagnosis when encountering young patients with lower limb claudication or calf
pain symptoms. This will facilitate early surgical
intervention to minimise the risk of complications.
Author contributions
All authors contributed to the design, acquisition of data, analysis of data, drafting of the manuscript, and critical
revision of the manuscript for important intellectual content.
All authors had full access to the data, contributed to the
study, approved the final version for publication, and take
responsibility for its accuracy and integrity.
Conflicts of interest
All authors have disclosed no conflicts of interest.
Funding/support
This pictorial medicine received no specific grant from any funding agency in the public, commercial, or not-for-profit
sectors.
Ethics approval
The patient was treated in accordance with the Declaration of Helsinki. The patient provided written informed consent for
the treatment/procedures, and consent for publication.
References
1. Thanila AM, Johnson CM, Hallett JW Jr, Breen JF. Popliteal artery entrapment syndrome: role of imaging in
the diagnosis. AJR Am J Roentgenol 2003;181:1259-65. Crossref
2. Davis DD, Shaw PM. Popliteal Artery Entrapment
Syndrome. In: StatPearls [Internet]. Treasure Island
(FL): StatPearls Publishing; 10 May 2019. Available from:
https://www.ncbi.nlm.nih.gov/books/NBK441965/.
Accessed 1 Apr 2020.
3. Tercan F, Oğuzkurt L, Kizilkiliç O, Yeniocak A, Gülcan O. Popliteal artery entrapment syndrome. Diagn Interv
Radiol 2005;11:222-4.
4. Eliahou R, Sosna J, Bloom AI. Between a rock and a hard place: clinical and imaging features of vascular
compression syndromes. Radiographics 2012;32:33-49. Crossref
5. Zhong H, Liu C, Shao G. Computed tomographic
angiography and digital subtraction angiography findings
in popliteal artery entrapment syndrome. J Comput Assist
Tomogr 2010;34:254-9. Crossref
6. Atilla S, Ilgit ET, Akpek S, Yücel C, Tali ET, Işik S. MR imaging and MR angiography in popliteal artery
entrapment syndrome. Eur Radiol 1998;8:1025-9. Crossref

