© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
CASE REPORT
Emergency single-port laparoscopic partial
adrenalectomy for adrenal abscess in an adult
with disseminated Streptococcus pyogenes
bacteraemia: a case report
DS Tam, MB, BS; CH Man, FHKAM (Surgery); KW Wong, FHKAM (Surgery); KC Ng, FHKAM (Surgery)
Department of Surgery, Caritas Medical Centre, Hong Kong
Corresponding author: Dr DS Tam (dicksontamds@gmail.com)
Case report
A 55-year-old man with unremarkable past health
who was a chronic smoker and drinker presented
to the emergency department in July 2019 with
2-day history of severe epigastric pain and fever.
On admission, the patient was septic-looking and
clinically unstable (blood pressure 138/94 mm Hg,
pulse 115 bpm, temperature 39.2°C). Physical
examination revealed epigastric tenderness and
guarding. Blood tests showed an elevated white
cell count of 20.89 × 109/L (reference range,
3.70-9.20 × 109/L) and C-reactive protein level of
>294 mg/L (reference range, <5.0 mg/L). Chest and
abdominal plain radiograph showed no free gas
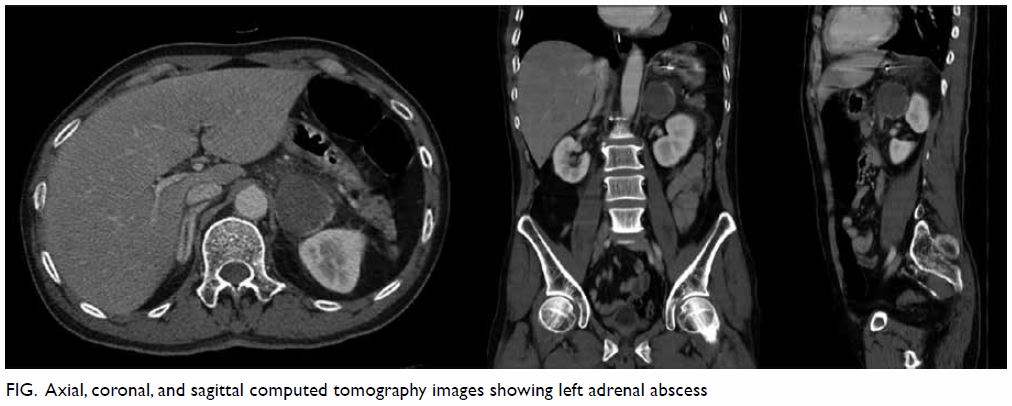
under the diaphragm. Urgent contrast computed
tomography (CT) of the abdomen and pelvis
demonstrated a 4.5 cm × 4 cm × 4 cm minimally
enhancing hypodense lesion in the left adrenal
gland with surrounding infiltrative changes (Fig).
The patient underwent fluid resuscitation and was
prescribed piperacillin/tazobactam. Retroperitoneal
CT-guided drainage of the left adrenal collection
performed the next day yielded 6 mL of pus. The
patient also reported right knee pain for 1 week. Physical examination revealed a right knee effusion.
Right knee tapping yielded straw-coloured joint
fluid, urgent Gram stain of which showed gram-positive
cocci. Emergency right knee arthroscopy
with synovectomy was performed for septic arthritis.
Intraoperatively there was pus within the knee
joint. Adrenal fluid aspirate, joint fluid and blood
culture all grew Streptococcus pyogenes (sensitive to
penicillin). However, his swinging fever persisted.
Extensive workup for other septic foci, including
urine and sputum culture, nasal swab for viruses
and bone marrow examination were all negative as
were autoimmune markers and hepatitis and human
immunodeficiency virus serology. He later developed
sepsis-induced congestive heart failure with acute
pulmonary oedema. Echocardiogram showed no
valvular vegetation. The patient’s haemodynamics
gradually improved with antibiotics.
Sepsis again worsened with septic shock
and desaturation. New chest radiograph revealed
pulmonary congestion and a further CT scan
showed interval shrinkage of the left adrenal abscess
(3.2 cm × 2.9 cm × 2.6 cm). The left adrenal abscess
was suspected as the remaining septic focus. Image-guided drainage was not possible since there was no
safety window. The abscess was small and very close
to the aorta so emergency single-port laparoscopic
left partial adrenalectomy was performed for
definitive drainage.
The patient underwent general anaesthesia and
was placed in a right lateral decubitus position. We
adopted a transperitoneal approach with a 3-cm left
subcostal incision. An OCTO-port was inserted, and
pneumoperitoneum was established. Laparoscopy
showed hyperaemic and inflammatory adhesions
around the left adrenal gland. Splenic flexure was
then taken down. The spleen and anterior surface
of the left kidney were mobilised to enable a clearer
view of the left adrenal gland. Initial tapping yielded
no pus so the left adrenal gland was opened and
the abscess cavity entered. Pus was drained and the
cavity irrigated with normal saline. The superficial
part of the abscess and its overlying adrenal tissue
were then resected. A 15-French silicon drain was
placed at the left adrenal bed. Finally, the fascial
defect and skin were closed with an interrupted 2-0
absorbable suture and skin staples, respectively. The
operating time was 210 minutes. Interval CT on
postoperative day 4 showed disappearance of the left
adrenal abscess. The surgical drain was removed on
day 5. Private positron emission tomography–CT
scan on day 15 showed no adrenal collection. The
patient was discharged on postoperative day 33.
Histopathology was reported as abscess.
Discussion
To the best of our knowledge, this is the first case
of adrenal abscess treated by emergency single-port
laparoscopic partial adrenalectomy. Adrenal
abscesses are uncommon in neonates and much rarer
in adults. In the literature, most adult cases are due to
disseminated infection in an immunocompromised
host or postoperative complications. One rare case
of acute appendicitis complicating adrenal abscess
has been reported.1 Iatrogenic cause due to fine needle aspiration of an adrenal nodule has also been
reported once only.2 Identified pathogens include Escherichia coli, Mycobacterium tuberculosis,
Nocardia, Salmonella, and Streptococcus spp.
Invasive group A streptococcus causing abdominal
or peritoneal infections is rare.3 Adrenal abscess can present as fever, malaise, abdominal, or back pain.
Diagnosis is by imaging, preferably CT. Principles
of management are adequate drainage and systemic
antimicrobials. Percutaneous image-guided drainage
is useful for small and simple abscesses. Those that
are large, multiloculated, lacking a safety window
for needle insertion or in which percutaneous
drainage has failed should be treated with surgical
drainage.
After the first single-port adrenalectomy
reported in 2005, there has been increasing evidence that laparo-endoscopic single-site adrenalectomy
is safe and has a comparable surgical outcome to a
conventional approach but with less wound pain and
better cosmesis.4 Partial adrenalectomy has been
applied for aldosterone-producing adenoma but
is more challenging than total adrenalectomy as it
is more difficult to gain a negative margin, ensure
haemostasis, and minimise damage to the remaining
adrenal tissue.5 The first single-port partial
adrenalectomy was reported in 2010. Currently there
is no solid evidence suggesting the best approach of
surgery. In our centre, we performed our first single-port
adrenalectomy in 2009. Since then, we routinely
perform this technique for left-sided adrenal lesions
and the surgical approach is transperitoneal.
Emergency adrenalectomy is much less well
investigated. The most common indication is
pheochromocytoma multisystem crisis, an acute
severe presentation of catecholamine-induced
hemodynamic instability causing end-organ damage
or dysfunction.6 Emergency surgery is the treatment
of choice, but the definitive timing of surgery is
controversial.
Most reported cases that require surgical
drainage have been treated by open surgery,7 except
two cases where standard laparoscopic drainage
was performed. Our patient is the first case of
adrenal abscess treated by emergency single-port
laparoscopic partial adrenalectomy. Intraoperatively,
initial tapping of the abscess yielded no pus. Hence,
we decided to proceed with partial adrenalectomy,
to resect as little overlying adrenal tissue as possible,
to drain the abscess adequately. At the end of surgery
when inserting the silicon drain, we did not insert
the drain via the same abdominal fascial defect at the
OCTO-port to prevent incisional hernia. The drain
exited the fascia adjacent to the fascial defect of the
OCTO-port, then exited the skin at the same port
site wound via a subcutaneous tunnel. There were no
surgical complications and postoperative recovery
was smooth.
In summary, adrenal abscess is rare in healthy
adults but can cause severe sepsis. Prompt surgery
is important when conservative management
fails. We demonstrate that emergency single-port
laparoscopic partial adrenalectomy is a feasible
approach for surgical drainage. More large-scale
studies and randomised trials are needed to provide
more solid evidence to support use of single-port
adrenalectomy in an emergency setting.
Author contributions
All authors contributed to the concept or design of the study, acquisition of the data, analysis or interpretation of the
data, drafting of the manuscript, and critical revision of the
manuscript for important intellectual content. All authors
had full access to the data, contributed to the study, approved
the final version for publication, and take responsibility for its
accuracy and integrity.
Conflicts of interest
All authors have disclosed no conflicts of interest.
Funding/support
This case report received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Ethics approval
The patient was treated in accordance with the Declaration of Helsinki. The patient gave written informed consent for all
investigations and interventions.
References
1. Dimofte G, Dubei L, Lozneanu LG, Ursulescu C, Grigora Scedil M. Right adrenal abscess—an unusual
complication of acute appendicitis. Rom J Gastroenterol
2004;13:241-4.
2. Masmiquel L, Hernandez-Pascual C, Simo R, Mesa J. Adrenal abscess as a complication of adrenal fine-needle
biopsy. Am J Med 1993;95:244-5. Crossref
3. Nelson GE, Pondo T, Toews KA, et al. Epidemiology of
invasive group A Streptococcal infections in the United
States, 2005-2012. Clin Infect Dis 2016;63:478-86. Crossref
4. Chung SD, Huang CY, Wang SM, Tai HC, Tsai YC,
Chueh SC. Laparoendoscopic single-site (LESS)
retroperitoneal adrenalectomy using a homemade single-access
platform and standard laparoscopic instruments.
Surg Endosc 2011;25:1251-6. Crossref
5. Yu CC, Tsai YC. Current surgical technique and outcomes of laparoendoscopic single-site adrenalectomy. Urol Sci
2017;28:59-62. Crossref
6. Wu R, Tong N, Chen X, et al. Pheochromocytoma crisis
presenting with hypotension, hemoptysis, and abnormal
liver function: a case report. Medicine (Baltimore)
2018;97:e11054. Crossref
7. Jackson C, McCullar B, Joglekar K, Seth A, Pokharna H. Disseminated nocardia farcinica pneumonia with left
adrenal gland abscess. Cureus 2017;9:e1160. Crossref