© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
CASE REPORT
Multidisciplinary staged management of
iliofemoral venous thrombosis caused by huge
uterine fibroid: a case report
H Zhang, MD1; HL Li, MD, PhD1; YC Chan, MB, BS, BSc1,2; DZ Cui, MD1; SW Cheng, MB, BS, MS1,2
1 Division of Vascular Surgery, Department of Surgery, The University of Hong Kong–Shenzhen Hospital, Shenzhen, Guangdong, China
2 Division of Vascular and Endovascular Surgery, Department of Surgery, The University of Hong Kong Medical Centre, Queen Mary Hospital, Hong Kong
Corresponding author: Prof YC Chan (ycchan88@hkucc.hku.hk)
Case report
A 45-year-old woman was admitted with a 2-day
history of sudden-onset swelling and pain of her
left thigh and calf. There was no history of trauma
or prolonged immobilisation. The patient had a
history of menorrhagia and a large uterine fibroid
treated conservatively. Physical examination showed
that the left leg was grossly swollen and tender,
with palpable pedal pulses, with a large pelvic mass
15 cm in diameter. Emergency ultrasound duplex
scan revealed a left iliofemoral venous thrombosis
(Fig 1a). There were no symptoms of pulmonary
embolism (PE). Blood D-dimer level was elevated
at 9.49 μg/mL. Pulmonary computed tomographic
angiography was unremarkable.
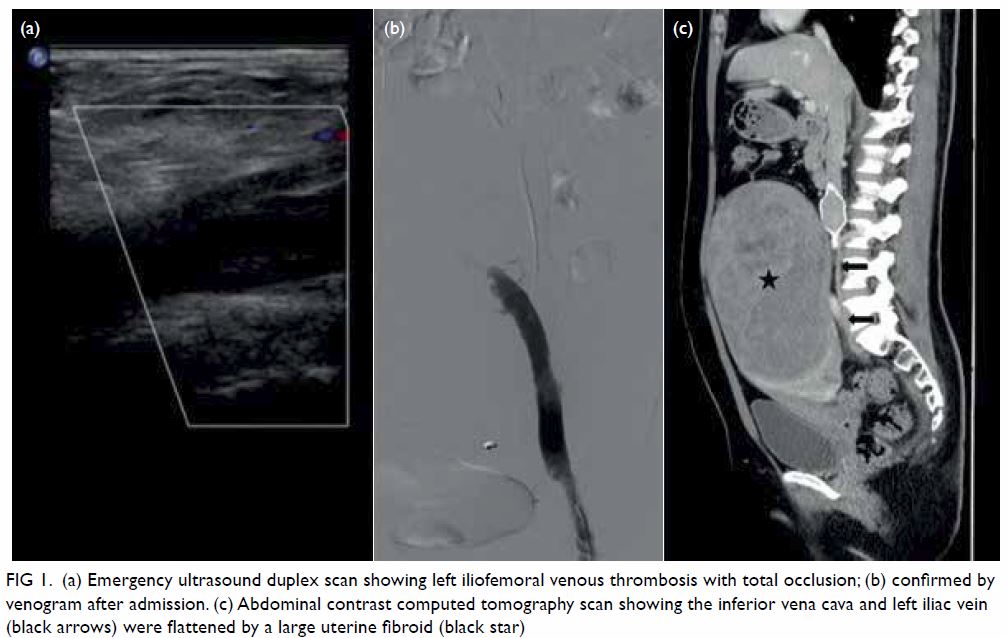
Figure 1. (a) Emergency ultrasound duplex scan showing left iliofemoral venous thrombosis with total occlusion; (b) confirmed by venogram after admission. (c) Abdominal contrast computed tomography scan showing the inferior vena cava and left iliac vein (black arrows) were flattened by a large uterine fibroid (black star)
Anticoagulation with low-molecular-weight heparin (Enoxaparin [Sanofi, France], 6000 IU, once
every 12 hours) was given immediately. Venogram
on the second day after admission revealed a left
iliofemoral deep venous thrombosis (DVT) with
total occlusion (Fig 1b). A retrievable inferior vena
cava filter (Lifetech; Shenzhen, China) was placed via
the right femoral vein. Left popliteal vein puncture
was performed under ultrasound guidance with the
patient in a prone position, and a 6F sheath inserted.
A 0.035” wire was passed through the left thrombosed
femoral and iliac vein, and an AngioJet catheter
(Boston Scientific, United States) passed over the
wire. After injection of 200 000 IU of urokinase
through the AngioJet catheter for 15 minutes,
mechanical thrombectomy was performed under
fluoroscopy. Completion venography confirmed that the femoral veins and iliac veins were completely
recanalised, but with some residual stenosis noted
at the proximal left common iliac vein. Venoplasty
with a 10-mm × 80-mm balloon (Advance 35LP
Low-Profile PTA Balloon Dilatation Catheter; Cook,
United States) was performed but the left common iliac vein collapsed after withdrawal. In view of
her history of giant uterine fibroid, an abdominal
contrast computed tomography scan was performed
and demonstrated a large uterine fibroid measuring
160 mm × 100 mm × 180 mm. The inferior vena cava
and left iliac vein were compressed and flattened
(Fig 1c).
After urgent multidisciplinary consultation
involving vascular surgeons and gynaecologists,
a transabdominal hysterectomy and bilateral
salpingectomy was performed 1 week later. The
oncologist was also involved in the diagnosis and
management of this case and decided against
radiotherapy or chemotherapy following surgery.
Anticoagulation with low-molecular-weight
heparin was administered perioperatively. Although
the gynaecologist encountered some difficulties
dissecting the uterus that was too large with the
anterior wall tightly adherent to the bladder, the
operation was completed with no complications.
Postoperatively, left leg swelling was much improved
but repeated duplex ultrasound showed residual,
albeit minimal, iliac vein thrombosis.
Repeat left iliac vein angioplasty and
stenting was performed 1 week later. Left proximal
common iliac vein stenosis was identified on
venogram, not improved by venoplasty alone with a
12-mm × 80-mm balloon (Cook) [Fig 2a] but
resolved following deployment of a self-expanding
14-mm × 80-mm Zilver stent (Cook) [Fig 2b]. The
vena cava filter was not retrieved as there was a large
thrombus lodged in the caval filter, demonstrated by
a filling defect at the apex of the filter. Subsequently,
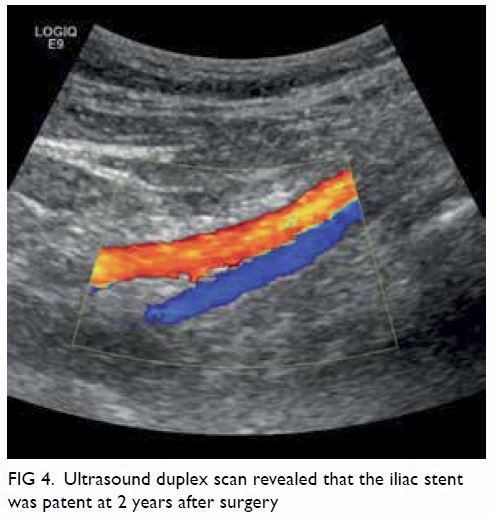
left leg swelling significantly improved (Fig 3a and b) and the patient was prescribed anticoagulation with
rivaroxaban for 1 year after surgery. The patient
remained asymptomatic during regular out-patient
follow-up examinations (Fig 3c and d) and the iliac
stent remained patent on ultrasound scan at 2 years
after surgery (Fig 4).
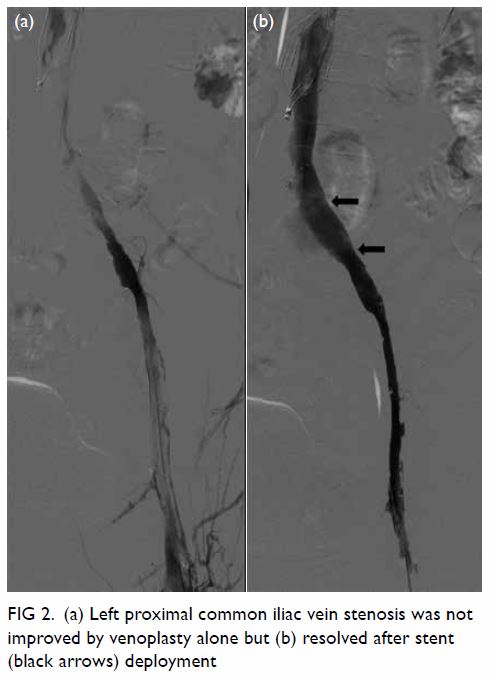
Figure 2. (a) Left proximal common iliac vein stenosis was not improved by venoplasty alone but (b) resolved after stent (black arrows) deployment

Figure 3. (a) Swollen left leg on admission, (b) improvement 1 week after thrombectomy and stenting, and complete resolution at (c) 3 months and (d) 2 years after surgery
Discussion
Uterine fibroids are common and benign but can
cause external compression on the iliac veins leading
to venous stasis and DVT formation, akin to a
subclinical May-Thurner phenomenon. Owing to
the complexity of the pathogenesis and the severity
of complications, patients with extensive DVT
secondary to fibroid uterus should be managed
urgently with a multidisciplinary approach.
Iatrogenic manipulation of the iliac veins
during surgery for hysterectomy may lead to
dislodgement of thrombi and increased risk of
pulmonary embolus.1 It is therefore advisable to have
a caval filter in situ and to continue with systemic
anticoagulation perioperatively. A caval filter during
thrombolysis should also be used routinely to
reduce the risk of embolisation when percutaneous
mechanical thrombectomy (PMT) is planned.2
The caval filter can be removed within 2 weeks if
there are no further thrombi but must remain in
situ if there are large clots in the apex of the caval
filter. Ideally, in our patient with acute iliofemoral
vein thrombosis, the hysterectomy should be
performed safely with the inferior vena cava filter
in place to prevent life-threatening PE during
surgery. Thrombectomy and iliac vein stenting may
be performed after hysterectomy. Percutaneous
mechanical thrombectomy provides greatest benefit in patients with acute extensive proximal (above knee) DVT, and is best performed within 14 days of
onset of symptoms.3
Compared with catheter-directed
thrombolysis, the potential benefits of mechanical
thrombectomy include shorter procedural time,
lower thrombolytic dosage, lower associated
systemic effects, and higher thrombus clearance.4
The success rate for PMT has been reported to be
93.4%,4 with a venous patency rate of 75% to 100%
after mean follow-up of 12.3 months.5 The potential
complications of PMT include injury or perforation
of the vein, PE caused by thrombus during
thrombectomy, and thrombolytic agent-related
haemorrhage. Nonetheless to date, there has been
no report of the application of PMT in the treatment
of DVT secondary to uterine fibroid. A retrospective
study showed that PMT is an acceptable initial
therapy in venous thrombosis patients with May-Thurner syndrome.6 In our patient, PMT was proven
effective and safe in the treatment of acute proximal
DVT caused by uterine fibroid.
Current guidelines make no recommendation
about the duration of anticoagulation following
iliofemoral vein stenting. Nonetheless it has been
reported that in selected patients with acute
iliofemoral deep vein thrombosis and patent
venous stent, particularly younger and otherwise
healthy patients with May-Thurner syndrome,
anticoagulation therapy can be safely discontinued
3 to 12 months after endovascular treatment.7 Our
patient received anticoagulation for 1 year after
surgery.
To the best of our knowledge, this is the first
case in the world’s literature to report a dedicated
staged venous procedure to treat a left iliofemoral
DVT in the presence of a large uterine fibroid.
Application of a staged process that combined
urgent caval filter insertion, PMT to remove the
DVT thrombus load as soon as possible, and
then hysterectomy to remove the external venous
compression, and finally completion venogram with
angioplasty or stenting of any residual stenosis was
an effective and safe treatment for acute iliac DVT
with large uterine fibroid. This multidisciplinary
dedicated staged therapeutic strategy resulted in a
successful long-term outcome.
Author contributions
Concept or design: H Zhang, HL Li, YC Chan.
Acquisition of data: H Zhang and DZ Cui.
Analysis or interpretation of data: H Zhang, HL Li, SW Cheng.
Drafting of the manuscript: H Zhang, HL Li, YC Chan.
Critical revision of the manuscript for important intellectual content: All authors.
Acquisition of data: H Zhang and DZ Cui.
Analysis or interpretation of data: H Zhang, HL Li, SW Cheng.
Drafting of the manuscript: H Zhang, HL Li, YC Chan.
Critical revision of the manuscript for important intellectual content: All authors.
All authors had full access to the data, contributed to the
study, approved the final version for publication, and take
responsibility for its accuracy and integrity.
Conflicts of interest
The authors have no conflicts of interest to disclose.
Funding/support
This case report received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Ethics approval
The patient was treated in accordance with the Declaration of Helsinki. The patient provided written informed consent for
all treatment and procedures and for publication of this paper.
References
1. Gupta S, Manyonda IT. Acute complications of fibroids. Best Pract Res Clin Obstet Gynaecol 2009;23:609-17.Crossref
2. Avgerinos ED, Hager ES, Jeyabalan G, Marone L,
Makaroun MS, Chaer RA. Inferior vena cava filter
placement during thrombolysis for acute iliofemoral deep
venous thrombosis. J Vasc Surg Venous Lymphat Disord
2014;2:274-81. Crossref
3. Kearon C, Kahn SR, Agnelli G, Goldhaber S, Raskob GE,
Comerota AJ. Antithrombotic therapy for venous
thromboembolic disease: American College of Chest
Physicians Evidence-Based Clinical Practice Guidelines
(8th edition). Chest 2008;133(6 Suppl):454S-545S. Crossref
4. Wang W, Sun R, Chen Y, Liu C. Meta-analysis and systematic
review of percutaneous mechanical thrombectomy for
lower extremity deep vein thrombosis. J Vasc Surg Venous
Lymphat Disord 2018;6:788-800. Crossref
5. Wong PC, Chan YC, Law Y, Cheng SW. Percutaneous
mechanical thrombectomy in the treatment of acute
iliofemoral deep vein thrombosis: a systematic review.
Hong Kong Med J 2019;25:48-57. Crossref
6. Kim IS, Jo WM, Chung HH, Lee SH. Comparison of clinical
outcomes of pharmaco-mechanical thrombectomy in iliac
vein thrombosis with and without May-Thurner syndrome.
Int Angiol 2018;37:12-8.
7. Sebastian T, Engelberger RP, Spirk D, et al. Cessation of
anticoagulation therapy following endovascular thrombus
removal and stent placement for acute iliofemoral deep
vein thrombosis. Vasa 2019;48:331-9. Crossref