Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
CASE REPORT
Extended middle pancreatectomy for a large
pancreatic cystic neoplasm: a case report
Albert KK Chui, FRACS, MD1; Juanita N Chui, BSC (Adv), MD2; Gregory E Antonio, FHKAM (Radiology), MD3; KC Lam, MB, BS, FHKAM (Surgery)4
1 Private Practice
2 School of Medicine, University of Sydney, Sydney, Australia
3 Department of Radiology, St Teresa’s Hospital, Hong Kong
4 Private Practice
Corresponding author: Dr Albert KK Chui (akkchui@netvigator.com)
Case report
In December 2016, a 47-year-old Chinese woman
was referred to our clinic for treatment of a large
cystic pancreatic lesion. She presented with a
12-month history of intermittent epigastric pain
associated with eating and weight loss of 5 kg.
The patient had a history of uterine fibroids and
underwent myomectomy 10 years previously. She
was also under observation for a benign thyroid
nodule. She had no family history of malignancy,
denied consumption of alcohol, was a non-smoker,
and lived as a housewife.
A contrast-enhanced computed tomography
scan of the abdomen revealed a cystic neoplasm 8 cm
in diameter involving the head, neck, and body of the
pancreas, with proximal dilatation of the pancreatic
duct (Fig 1). Based on the patient’s symptoms
and the size of the lesion, surgical resection was
recommended. Preoperative laboratory test results, including full blood count, liver and renal function
tests, blood glucose level, amylase, carcinoembryonic
antigen, and cancer antigen 19.9, were within normal
limits.
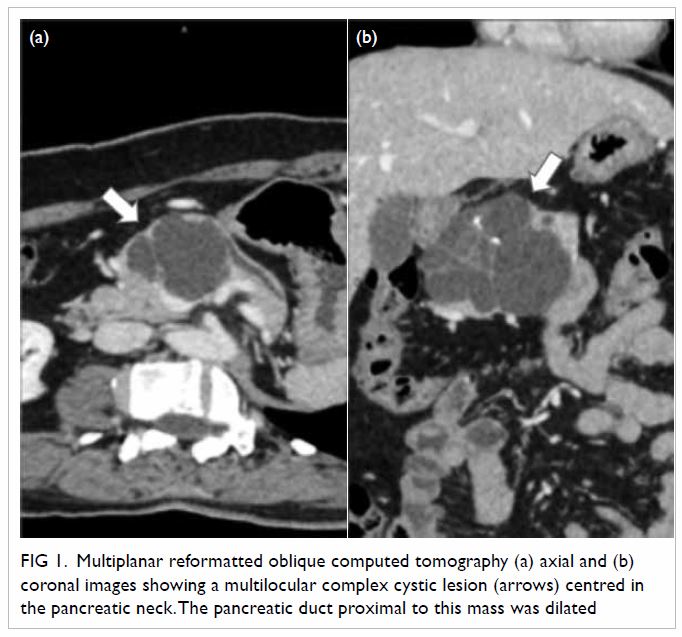
Figure 1. Multiplanar reformatted oblique computed tomography (a) axial and (b) coronal images showing a multilocular complex cystic lesion (arrows) centred in the pancreatic neck. The pancreatic duct proximal to this mass was dilated
During surgery, a multiloculated cystic lesion
was identified (Fig 2). The cystic content was serous.
No nearby enlarged lymph nodes or tissue invasion
suggestive of frank malignancy were evident. The
pancreatic tail was healthy. An extended middle
pancreatectomy (EMP) was performed. The patient
recovered without complication and was discharged
from hospital 13 days after surgery. Histological
examination of the resected tissue confirmed a
benign serous cystadenoma.
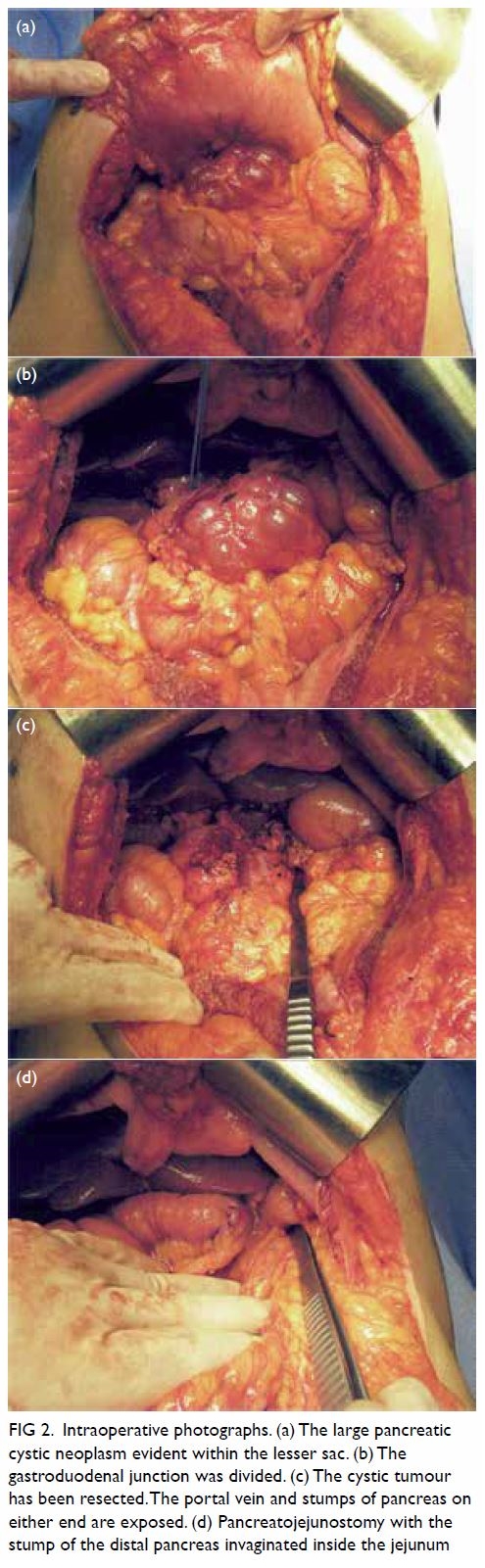
Figure 2. Intraoperative photographs. (a) The large pancreatic cystic neoplasm evident within the lesser sac. (b) The gastroduodenal junction was divided. (c) The cystic tumour has been resected. The portal vein and stumps of pancreas on either end are exposed. (d) Pancreatojejunostomy with the stump of the distal pancreas invaginated inside the jejunum
Surgical procedure
A bilateral subcostal incision was made. The lesser
sac was entered to expose the anterior aspect
of the pancreas after division of the gastrocolic
ligament (Fig 2a). The gastroduodenal junction was
purposefully divided to gain better exposure of the
large cystic lesion and to facilitate further pancreatic
dissection (Fig 2b). The posterior peritoneum along
the inferior and superior margins of the pancreas
was dissected. The superior mesenteric vein was
identified under the neck of the pancreas. The splenic
vein was carefully divided away from the gland and
all the small branches of the pancreas draining into
the splenic vein were ligated. The gallbladder was
removed to facilitate identification and mobilisation
of the common bile duct, the hepatic artery, and
the portal vein from above. The involved portion of
the pancreas was mobilised on both cephalic and
caudal sides. The cystic tumour was resected in its
entirety with a margin by scalpel and cautery. Most
of the head (estimated 80%-90%), neck, and body of
the pancreas were removed (Fig 2c). The remaining
pancreatic head stump was carefully over-sewn with
3-O Prolene sutures (Ethicon; Cornelia [GA], United
States) to avoid pancreatic leak. The pancreatic
duct opening was identified and separately sutured.
The stump was further re-enforced with fibrin
sealant, Tisseel glue (Baxter Healthcare, Deerfield [IL], United States). The distal side stump was
anastomosed into a Roux loop of jejunum using an
end-to-end technique with invagination (Fig 2d).
A short segment of catheter was inserted into the
pancreatic duct. The gastric pylorus was then joined
up to the proximal jejunum as a gastrojejunostomy
and a jejunojejunostomy was fashioned to prevent
bile reflux. The proximal jejunum was reconnected
to the jejunal Roux loop distally. Two drainage tubes
were placed close to the closed cephalic stump and
the pancreaticojejunostomy anastomosis before
proceeding with abdominal wound closure.
Discussion
For benign or low-grade malignant lesions
of the pancreatic neck and body, traditional
approaches for surgical resection include a
pancreaticoduodenectomy (PD) or an extended
distal pancreatectomy. Enucleation is suitable
only for small and superficial lesions that do not have
any connection with the pancreatic duct. In 1957,
Guillemin and Bessot first reported the technique of
middle pancreatectomy (MP) for chronic pancreatitis
and pancreatic transection injury.1 In 1982, Dagradi
and Serio proposed the use of MP for resection of
benign tumours or tumours with low malignant
potential situated in the pancreatic neck and body.2
The technique has since gained acceptance.
In this case, the large cystadenoma involved
a significant portion of the head of the pancreas
in addition to the neck and the body. Traditional
approaches for resection of such a lesion would
involve either subtotal pancreatectomy or PD. The
MP technique described in the literature has not
included resection of the head of the pancreas.
However, in this case, most of the pancreatic head
in addition to the neck and the body of pancreas
had to be resected. Therefore, the procedure is being
formally named for the first time, EMP.
Extended middle pancreatectomy permits
resection of a lesion that extends into the head of
the pancreas while conferring similar advantages of
an MP over traditional approaches. Compared with
other surgical options (subtotal pancreatectomy
and PD), this confers the advantage of parenchymal
preservation and consequent preservation of
pancreatic exocrine and endocrine functions.3
Pancreaticoduodenectomy has been associated with
increased postoperative morbidity and mortality.
Similarly, the inability to preserve the spleen in
subtotal pancreatectomy has been associated with
complications of thrombosis and susceptibility to
infection. Finally, MP has been associated with a
higher incidence of pancreatic fistula, compared
with PD and extended distal pancreatectomy
procedures.4 5 This has been attributed to the need
to manage two pancreatic remnants by anastomosis
or closure. However, as much less pancreatic head tissue is left behind in EMP, the risk of pancreatic
leak from the proximal stump should theoretically
be lower than that observed in MP.
We report, to the best of our knowledge, the
first clinical case of EMP in the management of a large
cystic neoplasm. This case demonstrated excellent
postoperative outcomes and suggests that EMP may
be considered a viable preferred surgical option in
selected cases. However, the technical difficulties
of this procedure should not be underestimated.
The long-term functional outcomes have yet to be
substantiated by further clinical experience.
Author contributions
All authors contributed to the concept or design of the
study, acquisition of the data, analysis or interpretation of
the data, drafting of the manuscript, and critical revision of
the manuscript for important content. All authors had full
access to the data, contributed to the study, approved the final
version for publication, and take responsibility for its accuracy
and integrity.
Conflicts of interest
As an Editor of the Journal, AKK Chui was not involved in
the peer review process. The other authors have disclosed no
conflicts of interest.
Funding/support
This case report received no specific grant from any funding
agency in the public, commercial, or not-for-profit sectors.
Ethics approval
The patient was treated in accordance with the tenets of the
Declaration of Helsinki. Patient consent was obtained.
References
1. Guillemin P, Bessot M. Chronic calcifying pancreatitis in
renal tuberculosis: pancreatojejunostomy using an original
technic [in French]. Mem Acad Chir (Paris) 1957;83:869-71.
2. Dagradi A, Serio G. Pancreatectomia intermedia. In:
Enciclopedia Medica Italiana. Pancreas, vol XI. Florence:
USES Ed Scientifiche; 1984: 850-1.
3. Tan Z, Chen P, Dong Z, Zhou B, Guo WD. Clinical efficacy
of middle pancreatectomy contrasts distal pancreatectomy:
a single-institution experience and review of literature.
ANZ J Surg 2019;89:E184-9. Crossref
4. Shibata S, Sato T, Andoh H, et al. Outcomes and indications
of segmental pancreatectomy. Comparison with distal
pancreatectomy. Dig Surg 2004;21:48-53. Crossref
5. Du ZY, Chen S, Han BS, Shen BY, Liu YB, Peng CH. Middle
segmental pancreatectomy: a safe and organ-preserving
option foe benign and low-grade malignant lesions. World
J Gastroenterol 2013;19:1458-65. Crossref

