Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
MEDICAL PRACTICE
Hong Kong College of Physicians Position
Statement and Recommendations on the
2017 American College of Cardiology/American Heart Association and 2018 European
Society of Cardiology/European Society of
Hypertension Guidelines for the Management of
Arterial Hypertension
KK Chan, FHKCP, FHKAM (Medicine)1; CC Szeto,FHKCP, FHKAM (Medicine)2; Christopher CM Lum, FHKCP, FHKAM (Medicine)3; PW Ng, FHKCP, FHKAM (Medicine)4; Alice PS Kong, MD, FHKCP, FHKAM (Medicine)2; KP Lau, FHKCP, FHKAM (Medicine)5; Jenny YY Leung, FHKCP, FHKAM (Medicine)6; SL Lui, MD (HK), FHKAM (Medicine)7; KL Mo, FHKCP, FHKAM (Medicine)1; Francis CK Mok, FHKCP, FHKAM (Medicine)8; Vincent CT Mok, FHKCP, FHKAM (Medicine)2; Bryan PY Yan, FHKCP, FHKAM (Medicine)2; Philip KT Li, FHKCP, FHKAM (Medicine)2
1 Department of Medicine, Pamela Youde Nethersole Eastern Hospital, Hong Kong
2 Department of Medicine and Therapeutics, The Chinese University of Hong Kong, Prince of Wales Hospital, Hong Kong
3 Department of Medicine and Geriatrics, Shatin Hospital, Hong Kong
4 Private Practice, Hong Kong
5 Department of Medicine, North District Hospital, Hong Kong
6 Department of Medicine, Ruttonjee Hospital, Hong Kong
7 Department of Medicine, Tung Wah Hospital, Hong Kong
8 Department of Medicine and Geriatrics, Tuen Mun Hospital, Hong Kong
Corresponding authors: Dr KK Chan, Prof Philip KT Li (chankk5@ha.org.hk; philipli@cuhk.edu.hk)
Abstract
The American College of Cardiology/American
Heart Association released guidelines for the
prevention, detection, evaluation, and management
of high blood pressure (BP) in adults in 2017. In
2018, the European Society of Cardiology (ESC)/European Society of Hypertension (ESH) published
new guidelines for the management of arterial
hypertension. Despite the many similarities between
these two guidelines, there are also major differences
in the guidelines in terms of diagnosis and treatment
of hypertension. A working group of the Hong
Kong College of Physicians (HKCP) convened
and conducted a focused discussion on important
issues of public interest, including classification of
BP, BP measurement, thresholds for initiation of
antihypertensive medications, BP treatment targets,
and treatment strategies. The HKCP concurs with
the 2018 ESC/ESH guideline on BP classification,
which defines hypertension as office systolic BP
≥140 mm Hg and/or diastolic BP ≥90 mm Hg. The
HKCP also acknowledges the growing evidence of
home BP monitoring and ambulatory BP monitoring
in the diagnosis and monitoring of hypertension and
endorses the wider use of both methods. The HKCP
also supports the direction of a risk-based approach
for initiation of antihypertensive medications and
the specification of a treatment target range for
both systolic and diastolic BP with consideration of
different age-groups and specific disease subgroups.
Non-pharmacological interventions are crucial, both at the societal and individual patient levels.
The recent guideline publications provide good
opportunities to increase public awareness of
hypertension and encourage lifestyle modifications
among the local population.
Introduction
In 2017, the American College of Cardiology (ACC)/American Heart Association (AHA) released a
guideline for the prevention, detection, evaluation,
and management of high blood pressure (BP) in
adults.1 This guideline was a collaborative effort by
11 organisations that updated the JNC7 (Seventh Report of the Joint National Committee on Prevention,
Detection, Evaluation and Treatment of High Blood
Pressure) in 2003.2 In 2018, the European Society of
Cardiology (ESC)/European Society of Hypertension
(ESH) published a new guideline for the management
of arterial hypertension.3 Both the European and
American guidelines provide comprehensive information for the clinical and public-health
practice communities on high BP management.
There are many similarities between these two
sets of guidelines: both emphasise the importance
of accurate BP measurement and encourage
out-of-office BP measurement for confirmation of
hypertension diagnosis. Both sets of guidelines also
recommend cardiovascular disease risk estimation
for risk stratification and a core strategy of
non-pharmacological lifestyle interventions and
drug treatment, including combination drug therapy.
Despite the many similarities between these two
guidelines, the guidelines also have major differences
in terms of diagnosis and treatment of hypertension.
Hypertension is prevalent in Hong Kong. In
a population health survey in 2014/15 conducted
by Department of Health,4 the prevalence of
hypertension (systolic BP [SBP] ≥140 mm Hg and/or
diastolic BP [DBP] ≥90 mm Hg) was 27.7% among
persons aged 15 to 84 years, with 47.5% of them
having been undiagnosed before the survey. The
prevalence of hypertension increased steadily with
age, from 4.5% among those aged 15 to 24 years to
64.8% among those aged 65 to 84 years.
A working group of the Hong Kong College
of Physicians (HKCP) convened and conducted a
focused discussion on important issues of public
interest pertaining to these two guidelines. This
document formulates the HKCP’s views on the
following issues: (1) classification of BP; (2) BP
measurement; (3) thresholds for initiation of
antihypertensive medications; (4) BP treatment
targets; and (5) treatment strategies.
Classification of blood pressure
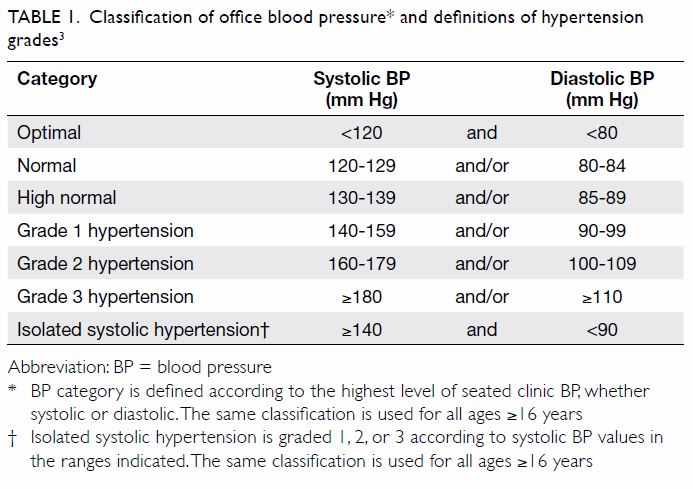
The 2018 ESC/ESH guideline defines hypertension
as office SBP ≥140 mm Hg and/or DBP ≥90 mm Hg
(Table 13). This definition remains unchanged from
the previous 2013 ESC/ESH guideline.5 However,
the 2017 ACC/AHA guideline contains a new BP
classification that proposes a lower threshold to
define hypertension (SBP ≥130 mm Hg and/or DBP
≥80 mm Hg). The same guideline defines normal
BP as <120/80 mm Hg and elevated BP as 120 to
129 mm Hg SBP and <80 mm Hg DBP.
The Systolic Blood Pressure Intervention
Trial is an important trial that significantly
influenced the recommendations of the 2017
ACC/AHA guidelines.6 The method used for office
BP measurement in the Systolic Blood Pressure
Intervention Trial was unattended automatic
measurement, in which automated multiple BP
readings in a doctor’s office are obtained with the
patient seated alone and unobserved. This method
has not been used in any previous randomised
controlled trials that provide an evidentiary basis
for the treatment of hypertension. The relationship
between conventional office BP measurement and unattended office BP measurement remains unclear,
but available evidence suggests that conventional
office SBP readings may be at least 5 to 15 mm Hg
higher.3
The 2017 ACC/AHA guideline’s definition
of hypertension is controversial. According to that
new definition, about 46% of adults in the US have
hypertension, as compared with about 32% under
the previous definition.1 This corresponds to an increase in the number of eligible patients requiring
treatment by more than 7 million in the US and more
than 55 million in China.7 The potential implications
for management of patients with hypertension are immense, both for individual patients as well society
and healthcare economics. The American College
of Physicians and the American Academy of Family
Physicians do not agree with this new definition of
hypertension.8
Other international guidelines, such as those
of the World Health Organization and International
Society of Hypertension,9 the Chinese Joint
Committee for Guideline Revision,10 the Japanese
Society of Hypertension,11 and Hypertension
Canada12 define hypertension as SBP ≥140 mm Hg
and/or DBP ≥90 mm Hg.
The HKCP concurs with the 2018 ESC/ESH
guideline on BP classification, which reflects the
BP-related cardiovascular risks and benefits of BP
reduction in clinical trials.
Blood pressure measurement
Both the European and American guidelines
strongly emphasise accurate BP measurement and
recording and consideration of readings in various
settings as needed. A description detailing the
steps of accurate BP measurement is provided (ie,
having the patient sit quietly for 5 minutes before
measurement, supporting the limb used to measure
BP, ensuring that the BP cuff is at heart level, and
using the correct cuff size). Out-of-office BP
measurements are recommended in patients with
suspected white coat hypertension, for confirmation
of the diagnosis of hypertension, and for titration of
BP-lowering medication, in conjunction with
telehealth counselling or clinical interventions.
Out-of-office BP measurement refers to home
BP monitoring and ambulatory BP monitoring.
These two methods use different BP thresholds
to define high BP than office-based methods do.
The 2018 ESC/ESH statement’s best estimates for
corresponding clinic BP, home BP monitoring, and
ambulatory BP monitoring can be considered as a
guide (Table 2).
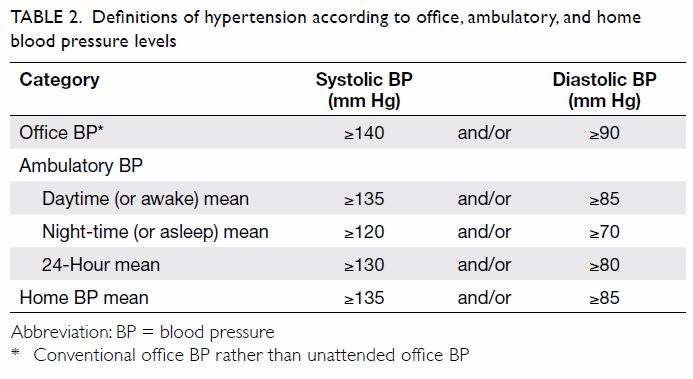
Table 2. Definitions of hypertension according to office, ambulatory, and home blood pressure levels
Although most randomised controlled trials have used clinic BP as the reference, the
HKCP acknowledges the growing body of evidence
surrounding the use of home and ambulatory BP
monitoring in the diagnosis and monitoring of
hypertension and endorses the wider use of both
methods.
Thresholds for initiation of
antihypertensive medications
Both the European and American guidelines adopt
a risk-based approach to treatment. Screening
for and management of other cardiovascular
disease risk factors common in hypertensive
patients is recommended. The European guideline
uses the Systematic COronary Risk Evaluation
system to estimate the 10-year risk of a first
fatal atherosclerotic event in relation to age, sex,
smoking habits, total cholesterol level, and SBP. It
is based on large, representative European cohort
datasets with correction factors for different
first-generation immigrants to Europe. Very high
risk, high risk, and moderate risk correspond to
calculated 10-year Systematic COronary Risk
Evaluation risk values of ≥10%, 5% to <10%, and
≥1% to <5%, respectively. Hypertensive patients
with documented cardiovascular disease, diabetes
mellitus, chronic kidney disease (stage 3-5), and very
high levels of individual risk factors (including grade
3 hypertension) are automatically considered to be
at high or very high risk.
The American guideline recommends using
the ACC/AHA Pooled Cohort Equations to estimate
the 10-year risk of atherosclerotic cardiovascular
disease and to guide treatment in mild hypertension.
However, the ACC/AHA Pooled Cohort Equations
are validated only in the US adults aged 45 to
79 years in the absence of concurrent statin therapy.
The results cannot be generalised to other age and
ethnic groups, and there are no correction factors to
refine the risk calculations for Asian populations.
According to the 2018 ESC/ESH guideline,
patients with grade 2 and 3 hypertension should
be treated with BP-lowering drug treatment and
lifestyle interventions. In patents with grade 1
hypertension (BP 140-159/90-99 mm Hg) at high
risk of cardiovascular disease or with hypertension-mediated
organ damage, drug treatment should
also be initiated simultaneously with lifestyle
interventions. In low- to moderate-risk patients
with grade 1 hypertension, BP-lowering drug
treatment should be initiated after 3 to 6 months if
BP is not controlled by lifestyle interventions alone.
Drug treatment in adults with high normal BP
(130-139/85-89 mm Hg) should only be considered
in very high-risk situations with the presence
of established cardiovascular disease, especially
coronary artery disease (Fig3). In fit, older patients
with hypertension (aged ≥80 years), BP-lowering drug treatment and lifestyle interventions are
recommended when SBP ≥160 mm Hg and/or DBP
≥90 mm Hg.
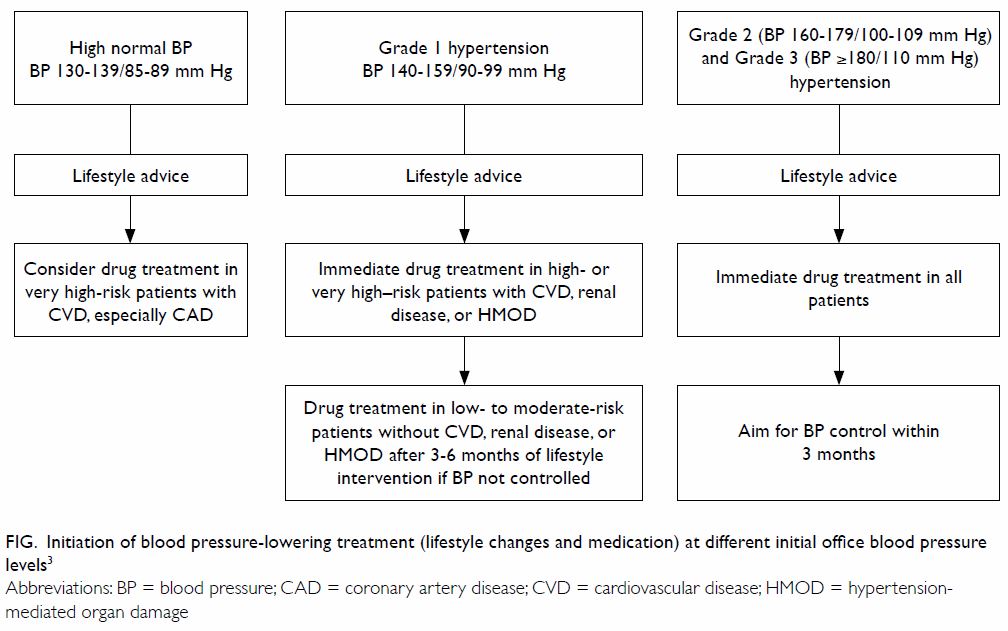
Figure. Initiation of blood pressure-lowering treatment (lifestyle changes and medication) at different initial office blood pressure levels3
The HKCP supports the direction of a riskbased
approach to treatment decision making and
echoes the 2018 ESC/ESH approach. The HKCP
recommends that patients seek physicians’ advice
and that individualised treatment be provided after
a complete assessment of the patient’s clinical profile,
risk factors, and preferences.
Blood pressure treatment targets
The American guideline recommends lowering BP to
<130/80 mm Hg for adults, except in older patients
(aged ≥65 years, noninstitutionalised, ambulatory,
community-living adults), in whom the target is SBP
<130 mm Hg. This one-size-fits-all BP goal raises
much concern, especially for the elderly population.13
In contrast, the American College of Physicians
and the American Academy of Family Physicians
recommend pharmacological treatment to a target
of SBP <150 mm Hg in adults aged ≥60 years
who have persistently elevated SBP (≥150 mm Hg)
and to a target of SBP <140 mm Hg in selected
patients with high cardiovascular risk.8
The European guideline establishes target
ranges. The first objective is to lower BP to
<140/90 mm Hg in all patients, and provided that
treatment is well tolerated, treated BP values should
be targeted to ≤130/80 mm Hg in most patients.
In patients aged <65 years who are receiving BP-lowering drugs, it is recommended that SBP be
lowered to 120 to 129 mm Hg in most patients. If
the BP value reaches 120/70 mm Hg, a step-down
of drug treatment should be considered, with close
BP monitoring during follow-up. In older patients
(aged ≥65 years) and in patients with chronic kidney
disease, the SBP target should be less aggressive:
130 to 139 mm Hg. A DBP target range of 70 to
79 mm Hg is considered for all hypertensive patients,
independent of risk level and co-morbidities.
The HKCP concurs with the 2018 ESC/ESH
guideline in specifying target ranges for both SBP and
DBP, with consideration of different age-groups and
specific disease subgroups.
Treatment strategies
The European and American guidelines have much
in common in terms of treatment strategies.14 Both
recommend a similar array of non-pharmacological
lifestyle interventions and drug treatments as the
core strategy for BP reduction.
Non-pharmacological interventions are crucial
in the prevention and management of high BP, either
on their own or in combination with pharmacological
therapy. These include weight reduction, heart-healthy
diet, sodium reduction, physical exercise,
smoking cessation, and moderation in alcohol intake.
The core drug treatment is based on four major
classes: angiotensin-converting enzyme inhibitors,
angiotensin receptor blockers, calcium channel
blockers, and thiazide/thiazide-like diuretics. Beta blockers are used when there is a specific indication
(eg, heart failure, angina, post myocardial infarction,
or heart rate control). Both guidelines recommend
the initiation of treatment in most patients with a
single-pill combination containing two drugs to
improve adherence and BP control. It is reasonable
to use monotherapy in frail older patients and those
at low risk with mild hypertension.
The HKCP assigns major importance to
non-pharmacological interventions, both at the
societal and individual patient levels. The HKCP
sees the recent guideline publications as good
opportunities to increase public awareness about
hypertension and to encourage lifestyle modifications
among the local population.
The HKCP agrees with the 2018 ESC/ESH
guideline’s drug treatment algorithm and the
initiation of a two-drug combination in most patients.
Monotherapy is recommended in frail older patients
and those at low risk with mild hypertension.
Specific considerations for
geriatric patients
Older patients are characterised by clinical
heterogeneity. A multi-dimensional assessment
is required to assess the biological age of each
individual patient, as well as the risks and benefits of
tight BP control. For patients aged 65 to 79 years with
few co-morbidities who are biologically young, the
target SBP should be 130 to 139 mm Hg, provided
that a medication burden is acceptable. For patients
aged ≥80 years, or patients aged 65 to 79 years with
multiple co-morbidities who are biologically old
(ie, frail), the optimal BP targets are not yet defined
and have to be individualised. A treatment goal of
SBP of 130 to <150 mm Hg can be considered, as
suggested by other professional societies.10 15 Careful
monitoring for any adverse effects or tolerability
problems associated with BP-lowering treatment
is required in frail and dependent older adults.
Monotherapy rather than a single-pill combination
is the preferable initial pharmacotherapy according
to the 2018 ESC/ESH guideline.
Specific considerations for renal
patients
Patients with chronic kidney disease should be
considered as having high cardiovascular risk.
Adequate hypertension control is important for
reducing the rate of renal function deterioration as
well as cardiovascular protection. The BP targets
should be tailored according to age, tolerability,
and the level of proteinuria.16 For diabetic and
non-diabetic patients with albumin excretion rates
of <30 mg per 24 hours (or equivalent), the suggested
BP target is ≤140/90 mm Hg. For diabetic and
non-diabetic patients with urinary albumin excretion ≥30 mg per 24 hours (or equivalent), the suggested
BP target is ≤130/80 mm Hg. The available evidence
is inconclusive but does not prove that a BP target
of <130/80 mm Hg improves clinical outcomes
more than a target of <140/90 mm Hg in adults with
chronic kidney disease.16
Specific considerations for
diabetic patients
Diabetes in combination with hypertension
magnifies the risk of diabetes-related complications.
Control of BP reduces the risk of microvascular
(retinopathy and nephropathy) and macrovascular
(especially stroke) complications. A BP goal of below
130/80 mm Hg is appropriate for individuals with
diabetes, particularly those with established kidney,
eye, or cerebrovascular damage, provided that the
medication burden is acceptable.17
The authors represent the Hong Kong College of Physicians in
the following capacity:
President: Philip KT Li
Cardiology Board: KK Chan, Bryan PY Yan
Nephrology Board: SL Lui, CC Szeto
Geriatric Medicine Board: Christopher CM Lum, Francis CK Mok
Neurology Board: PW Ng, Vincent CT Mok
Endocrinology, Diabetes and Metabolism Board: KP Lau, Jenny YY Leung
Advanced Internal Medicine Board: Alice PS Kong, KL Mo
President: Philip KT Li
Cardiology Board: KK Chan, Bryan PY Yan
Nephrology Board: SL Lui, CC Szeto
Geriatric Medicine Board: Christopher CM Lum, Francis CK Mok
Neurology Board: PW Ng, Vincent CT Mok
Endocrinology, Diabetes and Metabolism Board: KP Lau, Jenny YY Leung
Advanced Internal Medicine Board: Alice PS Kong, KL Mo
Author contributions
All authors contributed to the concept of the manuscript,
acquisition of data, analysis and interpretation of data, drafting
of the article and critical revision for important intellectual
content. All authors had full access to the data, contributed to
the study, approved the final version for publication, and take
responsibility for its accuracy and integrity.
Conflicts of interest
As an editor of the journal, BPY Yan was not involved in the
peer review process. Other authors have disclosed no conflicts
of interest.
Funding/support
This medical practice paper received no specific grant from any funding agency in the public, commercial, or not-forprofit
sectors.
References
1. Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/
AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection,
Evaluation, and Management of High Blood Pressure in
Adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical
Practice Guidelines. J Am Coll Cardiol 2018;71:e127-248. Crossref
2. Chobanian AV, Bakris GL, Black HR, et al. Seventh report
of the Joint National Committee on prevention, detection, evaluation, and treatment of high blood pressure.
Hypertension 2003;42:1206-52. Crossref
3. Williams B, Mancia G, Spiering W, et al. 2018 ESC/ESH
guidelines for the management of arterial hypertension.
Eur Heart J 2018;39:3021-104. Crossref
4. Centre for Health Protection, Department of Health, Hong
Kong SAR Government. Report of Population Health
Survey 2014/15. Available from: https://www.chp.gov.hk/en/static/51256.html. Accessed 14 Jan 2020.
5. Mancia G, Fagard R, Narkiewicz K, et al. 2013 ESH/ESC
guidelines for the management of arterial hypertension: the
Task Force for the Management of Arterial Hypertension
of the European Society of Hypertension (ESH) and of
the European Society of Cardiology (ESC). Eur Heart J
2013;34:2159-219. Crossref
6. SPRINT Research Group, Wright JT Jr, Williamson JD, et al.
A randomized trial of intensive versus standard blood-pressure
control. N Eng J Med 2015;373:2103-16. Crossref
7. Khera R, Lu Y, Lu J, et al. Impact of 2017 ACC/AHA
guidelines on prevalence of hypertension and eligibility
for antihypertensive treatment in United States and
China: nationally representative cross sectional study. BMJ
2018;362:k2357. Crossref
8. Wilt TJ, Kansagara D, Qaseem A, Clinical Guidelines
Committee of the American College of Physicians.
Hypertension limbo: balancing benefits, harms and patient
preferences before we lower the bar on blood pressure.
Ann Intern Med 2018;168:369-70. Crossref
9. Whitworth JA, World Health Organization, International
Society of Hypertension Writing Group. 2003 World
Health Organization (WHO)/International Society
of Hypertension (ISH) statement on management of
hypertension. J Hypertens 2003;21:1983-92. Crossref
10. Joint Committee for Guideline Revision. 2018 Chinese guidelines for prevention and treatment of hypertension—a
report of the Revision Committee of Chinese Guidelines
for Prevention and Treatment of Hypertension. J Geriatr
Cardiol 2019;16:182-245.
11. Umemura S, Arima H, Arima S, et al. The Japanese
Society of Hypertension guidelines for the management
of hypertension (JSH 2019). Hypertens Res 2019;42:1235-
481. Crossref
12. Nerenberg KA, Zarnke KB, Leung AA, et al. Hypertension
Canada’s 2018 guidelines for diagnosis, risk assessment,
prevention and treatment of hypertension in adults and
children. Can J Cardiol 2018;34:506-25. Crossref
13. Bakris G, Sorrentino M. Redefining hypertension—assessing the new blood-pressure guidelines. N Eng J Med
2018;378:497-9. Crossref
14. Whelton PK, Williams B. The 2018 European Society
of Cardiology/European Society of Hypertension and
2017 American College of Cardiology/American Heart
Association blood pressure guidelines: more similar than
different. JAMA 2018;320:1749-50. Crossref
15. Benetos A, Bulpitt CJ, Petrovic M, et al. An expert opinion
from the European Society of Hypertension–European
Union Geriatric Medicine Society Working Group on
management of hypertension in very old, frail subjects.
Hypertension 2016;67:820-5. Crossref
16. Tang SC, Wong AK, Mak SK. Clinical practice guidelines
for the provision of renal service in Hong Kong: general
nephrology. Nephrology (Carlton) 2019;24 Suppl 1:9-26. Crossref
17. Garber AJ, Handelsman Y, Grunberger G, et al. Consensus
statement by the American Association of Clinical
Endocrinologists and American College of Endocrinology
on the comprehensive type 2 diabetes management
algorithm—2020 executive summary. Endocr Pract
2020;26:107-29. Crossref