Hong Kong Med J 2020 Oct;26(5):382–9 | Epub 8 Oct 2020
Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE
Comparison of carbetocin and oxytocin infusions
in reducing the requirement for additional
uterotonics or procedures in women at increased
risk of postpartum haemorrhage after
Caesarean section
KY Tse, MB, BS, MRCOG; Florrie NY Yu, FHKAM (Obstetrics and Gynaecology); KY Leung, FRCOG
Department of Obstetrics and Gynaecology, Queen Elizabeth Hospital, Hong Kong
Corresponding author: Dr KY Tse (barontse@hotmail.com)
Abstract
Introduction: Postpartum haemorrhage is a major
cause of maternal mortality and morbidity, commonly
due to uterine atony. Prophylactic oxytocin use
during Caesarean section is recommended; patients
with a high risk of postpartum haemorrhage may
require additional uterotonics or procedures.
Carbetocin is a long-acting analogue of oxytocin
which has shown beneficial results, compared with
oxytocin. This study compared the requirement for
additional uterotonics or procedures between at-risk
women who underwent carbetocin infusion and
those who underwent oxytocin infusion.
Methods: This retrospective cohort study included
women at increased risk of postpartum haemorrhage
after Caesarean section for various indications
in a public hospital. Women who received carbetocin
infusion and women who received oxytocin infusion
were compared, stratified by Caesarean section
timing (elective or emergency). The primary outcome
was the requirement for additional uterotonic agents
or procedures. Secondary outcomes included total
blood loss, operating time, rate of postpartum
haemorrhage, need for blood transfusion, and need
for hysterectomy.
Results: Of 1236 women included in the study, 752
received oxytocin first and 484 received carbetocin
first. The two groups had comparable blood loss,
operating time, rate of postpartum haemorrhage,
requirement for additional uterotonics or
procedures, need for blood transfusion, and need
for hysterectomy. There was a reduction in the
requirement for additional uterotonics or procedures,
and in the rate of postpartum haemorrhage for
women with major placenta praevia or with multiple
pregnancies, following receipt of carbetocin first.
Conclusion: Compared with oxytocin, carbetocin
can reduce the requirement for additional uterotonics
or procedures in selected high-risk patient groups.
New knowledge added by this study
- The use of carbetocin reduced the requirement for additional uterotonics or procedures in women with major placenta praevia and in women with multiple pregnancies.
- Infusions of carbetocin and oxytocin had differential effects on the requirement for additional uterotonics or procedures in women who underwent Caesarean section for different indications.
- Women who received carbetocin infusion had similar blood loss, operating time, rate of postpartum haemorrhage, requirement for additional uterotonics or procedures, need for blood transfusion, and need for hysterectomy, compared with women who received oxytocin infusion.
- Carbetocin may be appropriate for women undergoing Caesarean section for major placenta praevia or multiple pregnancies.
- Oxytocin may be appropriate for women undergoing Caesarean section for other indications.
- There is a need to investigate the cost-effectiveness of carbetocin, which will aid clinicians in treatment selection.
Introduction
Postpartum haemorrhage is the major cause of
maternal death and morbidity worldwide,1 commonly
due to uterine atony (approximately 70% of cases).2 This type of haemorrhage is defined as blood loss of at
least 500 mL after vaginal delivery and blood loss of
>1000 mL after Caesarean section.3 Oxytocin (with or
without ergometrine) is the current standard therapy for the prevention of postpartum haemorrhage; it is a
peptide hormone secreted by the posterior pituitary
gland, which stimulates myometrial contraction
in the second and third stages of labour. However,
failure of postpartum haemorrhage prophylaxis with
oxytocin (as demonstrated by the need for a rescue
uterotonic) occurs commonly, necessitating the use
of further oxytocin or other treatments to maintain
haemodynamic stability.4
Carbetocin is a synthetic analogue of oxytocin
which has a longer half-life than oxytocin, thus
reducing the requirement for an infusion after the
initial dose. This difference in structure, compared
with oxytocin, makes carbetocin more stable;
thus, carbetocin can avoid early decomposition by
disulfidase, aminopeptidase, and oxidoreductase
enzymes. Compared with oxytocin, carbetocin
induces a prolonged uterine response, in terms of
both amplitude and frequency of contractions, when
administered postpartum.5
A Cochrane review in 2012 found that
carbetocin reduced the use of additional uterotonics
and uterine massage, when compared with oxytocin.3
In 2018, a meta-analysis involving seven trials
showed that carbetocin was effective in reducing the
use of additional uterotonics, as well as in reducing
postpartum haemorrhage and transfusion, when
used during Caesarean section.6 A recent meta-analysis
involving 30 trials has shown that carbetocin
is effective in reducing the need for additional uterotonic use and postpartum blood transfusion in
women at increased risk of postpartum haemorrhage
after Caesarean delivery.7 Another recent
meta-analysis involving nine trials has shown that
carbetocin is associated with a 53% reduction in the
need for additional uterotonics, when compared with
oxytocin, at the time of elective Caesarean delivery.8
The use of carbetocin has been recommended in
elective Caesarean sections by the Royal College of
Obstetricians and Gynaecologists9 and the Society of
Obstetricians and Gynaecologists of Canada.10
In one meta-analysis,6 heterogeneity was found
in the use of dose of oxytocin, which ranged from 2 IU
to 10 IU of bolus oxytocin to infusions of 20 to 30 IU,
and in the indications for Caesarean section. In a study
of 1568 Chinese women who underwent Caesarean
section for different indications, carbetocin and
oxytocin were found to have differential effects on
postpartum haemorrhage and related changes.6
However, to the best of our knowledge, most studies
have compared the differential therapeutic effects of
carbetocin and oxytocin in the general population or
in low-risk groups. Carbetocin is a relatively more
expensive drug than conventional synthetic oxytocin
(eg, Syntocinon), and there has not been sufficient
evidence from cost-effectiveness studies to support
its use in all patients. The use of carbetocin is therefore
limited to certain high-risk populations in some
institutions, including our hospital. The aim of the
present study was to compare effectiveness between
carbetocin and oxytocin in terms of reducing the
requirement for additional uterotonics in women at
increased risk of postpartum haemorrhage after
Caesarean section.
Methods
This study was conducted at the Department of
Obstetrics and Gynaecology, Queen Elizabeth
Hospital, Hong Kong, from 1 January 2016 to 30
June 2019; during this period, 5994 pregnant women
underwent Caesarean section in our hospital.
Demographic characteristics, obstetric histories,
risk factors, and perinatal outcomes were collected.
The study was approved by the Hospital Authority
Research Ethics Committee (Kowloon Central/Kowloon East) [KC/KE-20-0073/ER-1].
The inclusion criteria were women who
underwent Caesarean section for live birth after
24 weeks of completed gestation during the
aforementioned time period, with high risk of
developing postpartum haemorrhage (including
placenta praevia, presence of uterine fibroids,
multiple pregnancies, polyhydramnios, and
macrosomia), excluding patients with low risk
(n=4758, of whom 96 had low risk but received
oxytocin and carbetocin after identification of
postpartum haemorrhage). Patients who received
both oxytocin and carbetocin were assigned to the group where the first drug (oxytocin or carbetocin)
was used for prevention of postpartum haemorrhage,
then considered to require additional uterotonics
(carbetocin or oxytocin).
In our hospital, the implementation of
carbetocin began in April 2017. Prior to the
implementation of carbetocin, women who
were presumed to have a low risk of postpartum
haemorrhage were administered 10 IU oxytocin
intravenous bolus after delivery of the baby during
Caesarean section; women who were presumed to
have a high risk of postpartum haemorrhage were
administered 40 IU oxytocin intravenous infusion
over the course of 5 hours for a longer protective
effect. Depending on the clinical response,
further infusion of oxytocin might be indicated.
Following the implementation of carbetocin, we
have revised our protocol to administer the drug
100 μg intravenously over 1 minute for a single
dose after delivery of the baby, for women with
a high risk of postpartum haemorrhage (ie, with
the aforementioned risk factors) or for women
who required such treatment in accordance with
the obstetrician’s judgement. Contra-indications
included hypersensitivity to carbetocin, timing
prior to delivery of the baby, vascular disease
(especially coronary artery disease), and hepatic
or renal disease. The use of blood transfusion,
additional uterotonic agents (eg, carboprost 250 μg
intramuscularly or intramyometrially, misoprostol
800 μg rectally, oxytocin infusion after carbetocin,
or carbetocin after oxytocin infusion), obstetric
balloon tamponade, compression suture, uterine
artery embolisation, uterine artery ligation, or
hysterectomy was based on the control of postpartum
haemorrhage and the patient’s vital signs, as well as
the attending obstetrician’s judgement.
In this study, we subdivided the patients
according to risk factors. We then analysed each
patient group separately: patients who underwent
elective Caesarean section (ie, those who underwent
Caesarean section before labour onset) versus
patients who underwent emergency Caesarean
section (ie, those who either underwent intrapartum
Caesarean section, or who underwent Caesarean
section prior to the scheduled elective date for
reasons such as heavy antepartum haemorrhage).
The primary outcome was the requirement
for additional uterotonic agents or haemostatic
procedures (carboprost, misoprostol, oxytocin
infusion after carbetocin, carbetocin after oxytocin
infusion, obstetric balloon tamponade, uterine artery
embolisation, or uterine artery ligation). Secondary
outcomes were estimated blood loss, rate of
postpartum haemorrhage, operating time, the need
for blood transfusion, and the need for hysterectomy.
Blood loss was estimated by measuring the volume
within the suction bottle and the uptake in surgical drapes, pads, and gauzes. Postpartum haemorrhage
was defined as blood loss >1000 mL during or
immediately after the operation.
Statistical analysis was performed using IBM
SPSS Statistics for Windows, version 20.0 (IBM Corp,
Armonk [NY], United States). Continuous variables
were expressed as the mean±standard deviation and
compared by Student’s t test. Qualitative data were
expressed as number (percentage) and compared by
the Chi squared test or Fisher’s exact test. A P value of
<0.05 was considered statistically significant. Linear
regression and multiple logistic regression were used
to control for potential confounding factors when
assessing the associations of carbetocin treatment
with primary outcomes. Potential confounding
factors included age, parity, fetal body weight,
gestation, and order of pregnancy. Unstandardised
regression coefficients, adjusted odds ratios, and
associated 95% confidence intervals were calculated
to estimate relative risk.
Results
Of 5994 pregnant women who underwent Caesarean
sections during the study period, 4758 were excluded
because they were at low risk of postpartum
haemorrhage. Of the remaining 1236 women who
met the criteria for inclusion in the study, 752
received oxytocin first and 484 received carbetocin
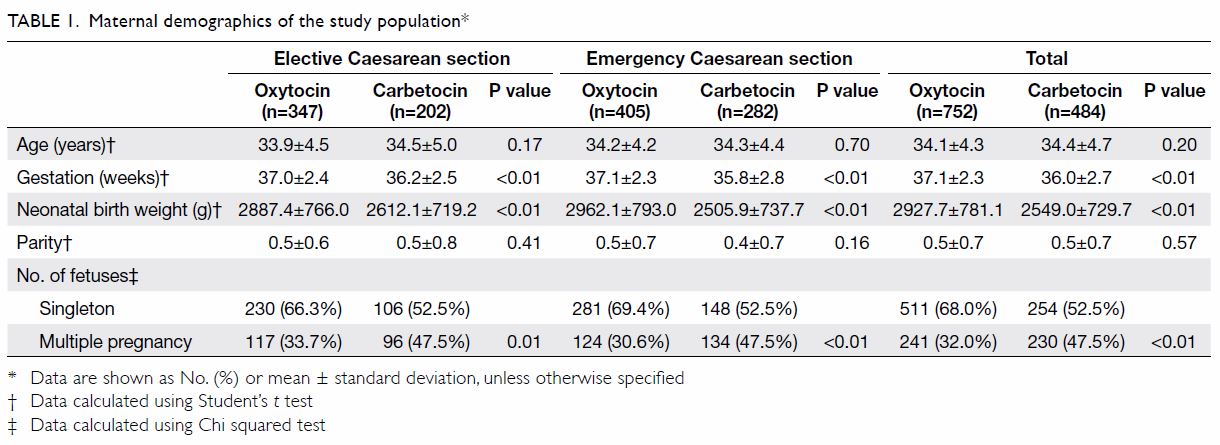
first. Compared with women who received oxytocin
first, women who received carbetocin first had earlier
gestation, lower neonatal birth weight, and a greater
proportion of twins or higher order pregnancy
(Table 1). The two groups had comparable blood loss,
operating time, rate of postpartum haemorrhage,
requirement for additional uterotonics and
procedures, need for blood transfusion, and need for
hysterectomy (Table 2).
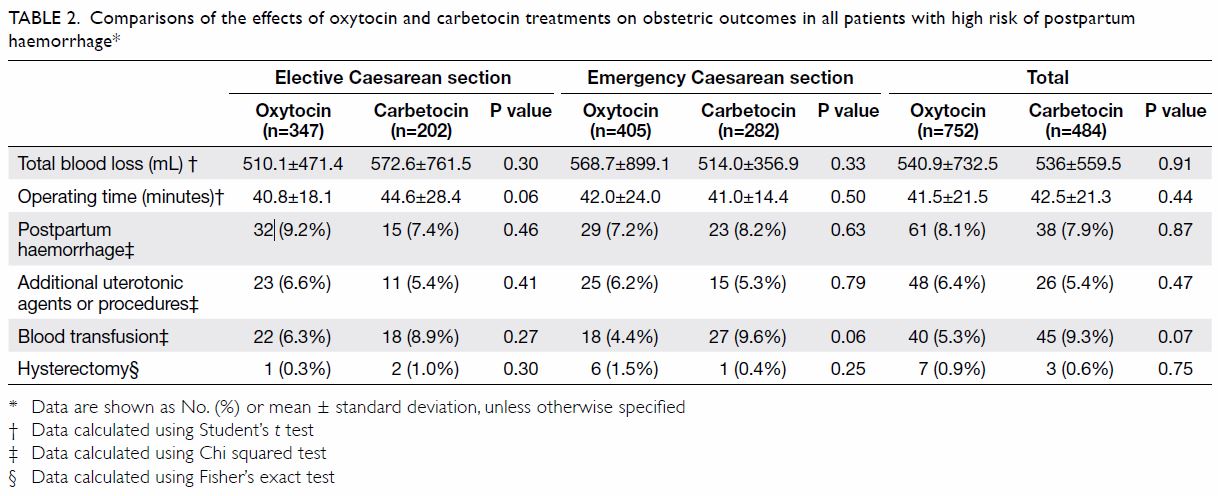
Table 2. Comparisons of the effects of oxytocin and carbetocin treatments on obstetric outcomes in all patients with high risk of postpartum haemorrhage
Significant reductions in the rate of postpartum
haemorrhage and in the requirement for additional
uterotonics or procedures were observed among
women with multiple pregnancies (Table 3a) and
women with major placenta praevia (Table 3b).
Significant reductions in total blood loss were also
observed for women with multiple pregnancies
and women with major placenta praevia in the
emergency Caesarean group. Additionally, the rate
of hysterectomy was significantly reduced in
women with multiple pregnancies in the emergency
Caesarean group.
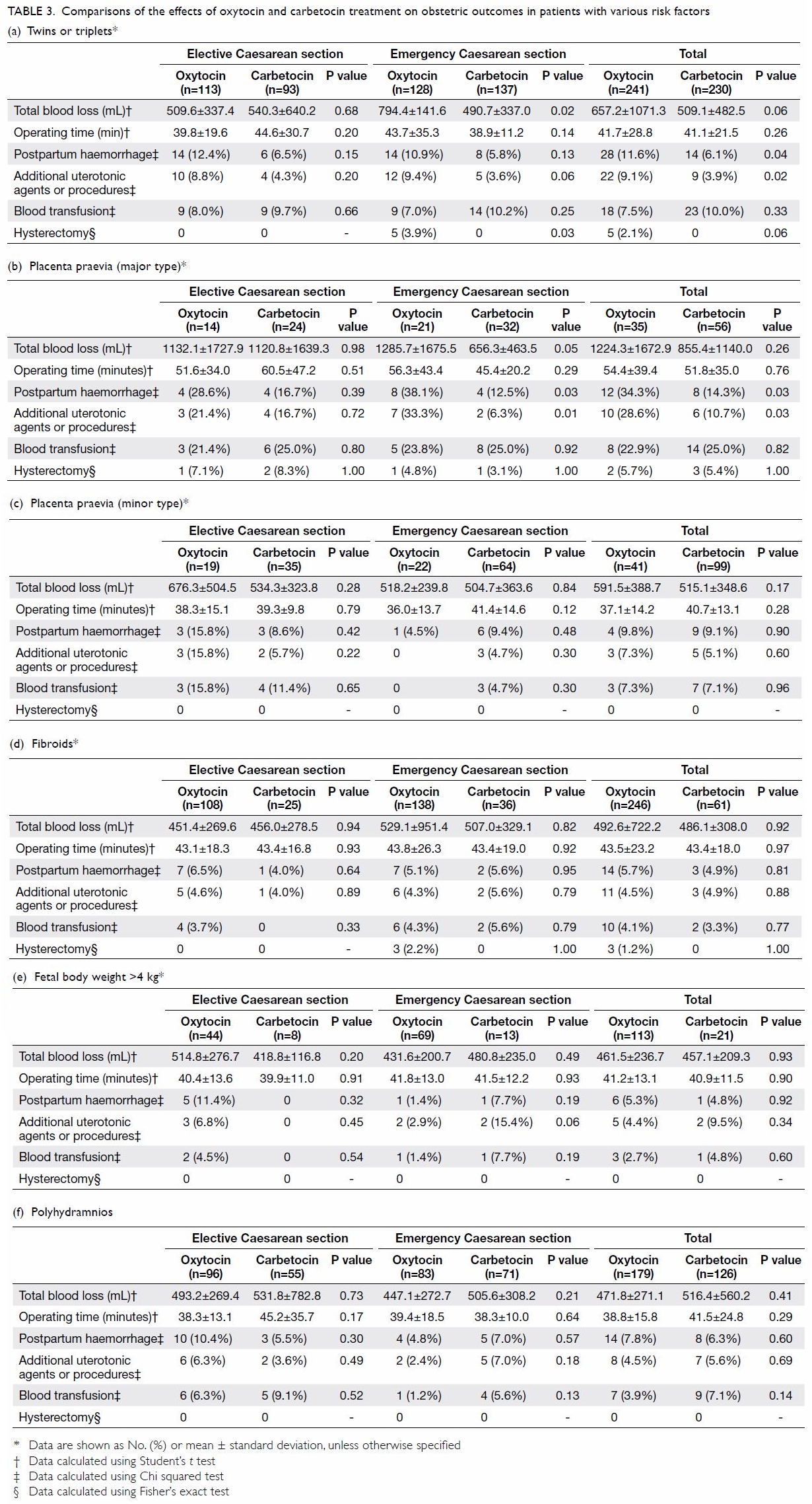
Table 3. Comparisons of the effects of oxytocin and carbetocin treatment on obstetric outcomes in patients with various risk factors
For women with minor placenta praevia
(Table 3c), fibroids (Table 3d), macrosomia
(Table 3e), or polyhydramnios (Table 3f), no
significant differences in total blood loss, operating
time, rate of postpartum haemorrhage, requirement
for additional uterotonics, need for blood
transfusion, or need for hysterectomy were observed
between the two groups.
After adjustments for confounding effects,
linear regression analysis revealed reductions in
the rate of postpartum haemorrhage and in the
requirement for additional uterotonics or procedures
for Caesarean section in women with major placenta
praevia and in women with multiple pregnancies,
but not for other risk factors (Table 4).
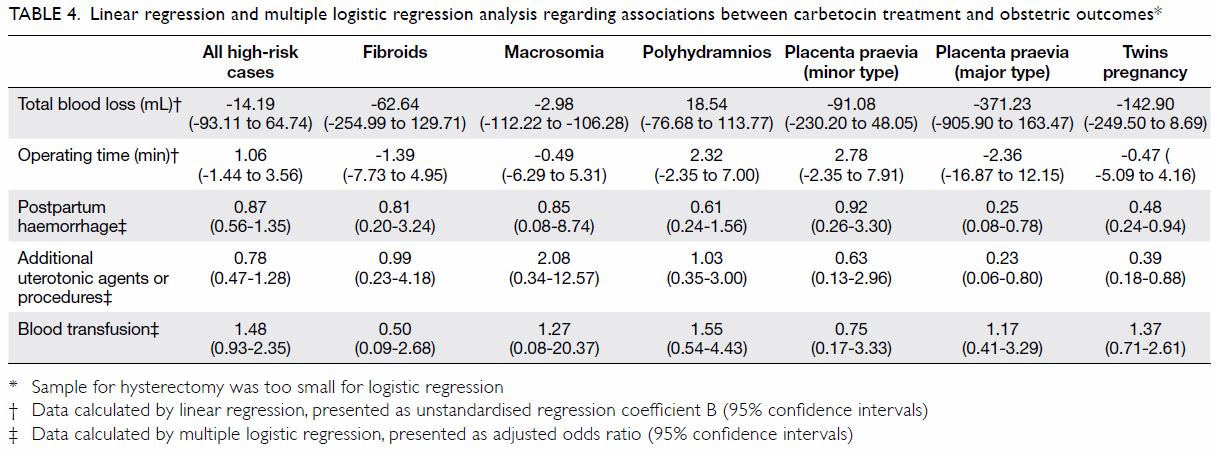
Table 4. Linear regression and multiple logistic regression analysis regarding associations between carbetocin treatment and obstetric outcomes
No serious side-effects were reported after the
use of carbetocin.
Discussion
This study showed that the general cohort of women
with risk factors for postpartum haemorrhage who
received carbetocin treatment exhibited comparable
blood loss, rate of postpartum haemorrhage,
requirement for additional uterotonics or
procedures, need for blood transfusion, and need for
hysterectomy, compared with oxytocin treatment. Our results are inconsistent with the findings of
previous studies,11 12 13 14 in which there were reductions
in blood loss and risk of postpartum haemorrhage
among women in the general population following
receipt of carbetocin alone, compared with oxytocin
alone. We presume that the difference was related
partly to the use of different oxytocin regimens. In
particular, 40 IU oxytocin infusion (greater than the
effective dose of carbetocin, 10 IU oxytocin) was
used in the present study, whereas a smaller dose
of oxytocin infusion of 10 to 20 IU or a bolus of
5 IU was used in previous studies.4 15 16 Furthermore,
the indications for Caesarean section might
have differed between the present study and the
prior studies. Notably, carbetocin and oxytocin
have been shown to exert differential effects on
postpartum haemorrhage and related changes in
patients undergoing Caesarean section for different
indications.6
When we analysed individual risk factors for
postpartum haemorrhage, we found significant
reductions in the use of additional uterotonics
or procedures and in the rate of postpartum
haemorrhage in women with major placenta praevia
and in women with multiple pregnancies. We also
observed a significant reduction in total blood loss
in the emergency Caesarean section group for both
women with major placenta praevia and women with multiple pregnancies. Our results are consistent
with the findings of a previous study in which lower
haemoglobin and haematocrit differences were
found in women who received carbetocin treatment
during Caesarean section due to multiple gestation
or placenta praevia, compared with women who
received oxytocin treatment.15 Carbetocin can
induce strong contraction of an overdistended uterus
associated with twin pregnancies.16 However, a study in 2013 did not show beneficial effects of carbetocin
administration.17 The sample size was small in that
study and its design comprised a retrospective
before-and-after analysis. Additionally, we presume
that the beneficial effect of carbetocin in reduction
of bleeding in women with placenta praevia might
be related to its effectiveness in stimulating the
retroplacental myometrium.18 Carbetocin can
shorten the third stage, prevent and treat retained
placenta at term, and prevent and treat second
trimester abortion.19 However, our results were
inconsistent with the findings of a previous study,
in which the additional effects of carbetocin were
presumed to be trivial because of thinning in the
lower uterine myometrium, thereby reducing the
immunoreactivity of oxytocin receptors relative to
the upper part of the uterus.20
We noted that the significant differences in
outcomes between treatments were mainly due to the
contributions of the emergency Caesarean section
group. Previous studies have largely demonstrated
beneficial effects from carbetocin treatment in
women undergoing elective Caesarean section, but
not in women undergoing intrapartum Caesarean
section.15 21 A possible explanation might be that
emergency Caesarean sections were performed
before the date of scheduled Caesarean section date;
hence, the gestational age and fetal weight were
typically lower at the time of the operation.
The greatest strength of this study was that
it included a relatively large sample size, which
comprised 1236 patients in one hospital with
standard protocols. There were a few limitations in
this study. First, it used single-centre, retrospective
design. Second, complete blood count data were not
routinely collected before delivery during the study
period, so these data could not be compared among
subgroups. Third, the implementation of carbetocin
began in April 2017. Since this implementation, most
patients with the risk factors considered in this study
were administered carbetocin instead of oxytocin
infusion, in accordance with our department
protocol. This led to a comparison between different
time frames, during which there were changes in
medical personnel and training. Finally, judgement
regarding the use of additional uterotonic agents
and transfusion may have differed among attending
physicians.
In clinical practice, the use of carbetocin
has been acknowledged in guidelines from the
Society of Obstetricians and Gynaecologists of
Canada10 and the Royal College of Obstetricians
and Gynaecologists.9 We recommend the use of
carbetocin during Caesarean section for women with
multiple pregnancies and major placenta praevia,
based on the beneficial effects demonstrated in the
present study and in prior studies.15 In women with
other risk factors for postpartum haemorrhage, we recommend the use of oxytocin infusion, instead of
carbetocin.15 Larger studies or prospective trials are
needed to investigate the effectiveness of carbetocin
during Caesarean section for different indications
and in women with risk factors for postpartum
haemorrhage; such studies are also needed to
establish the cost-effectiveness of this relatively new
drug.
In conclusion, we found that carbetocin
and oxytocin infusion had differential effects on
the requirement for additional uterotonics or
procedures in women who underwent Caesarean
section for different indications. In particular,
compared with oxytocin infusion, carbetocin was
associated with a reduction in the requirement for
additional uterotonics or procedures for women
with multiple pregnancies and women with major
placenta praevia.
Author contributions
Concept or design: All authors.
Acquisition of data: KY Tse, FNY Yu.
Analysis or interpretation of data: KY Tse, FNY Yu.
Drafting of the manuscript: KY Tse, KY Leung.
Critical revision of the manuscript for important intellectual content: KY Tse, KY Leung.
Acquisition of data: KY Tse, FNY Yu.
Analysis or interpretation of data: KY Tse, FNY Yu.
Drafting of the manuscript: KY Tse, KY Leung.
Critical revision of the manuscript for important intellectual content: KY Tse, KY Leung.
All authors had full access to the data, contributed to the study, approved the final version for publication, and take
responsibility for its accuracy and integrity.
Conflicts of interest
As an editor of the journal, KY Leung was not involved in the peer review process. Other authors have no conflicts of
interests to disclose.
Funding/support
This study did not receive any specific grant from funding agency in the public or commercial sectors.
Ethics approval
This study was approved by the Hospital Authority Kowloon Central/Kowloon East Research Ethics Committee (Ref KC/KE-20-0073/ER-1).
References
1. Say L, Chou D, Gemmill A, et al. Global causes of maternal
death: a WHO systematic analysis. Lancet Glob Health
2014;2:e323-33. Crossref
2. Anderson JM, Etches D. Prevention and management of
postpartum haemorrhage. Am Fam Physician 2007;75:875-
82.
3. Su LL, Chong YS, Samuel M. Carbetocin for preventing
postpartum haemorrhage. Cochrane Database Syst Rev
2012;(4):CD005457. Crossref
4. Fahmy NG, Yousef HM, Zaki HV. Comparative study
between effect of carbetocin and oxytocin on isofluraneinduced
uterine hypotonia in twin pregnancy patients
undergoing cesarean section. Egypt J Anaesth 2016;32:117-
21. Crossref
5. Hunter DJ, Schulz P, Wassenaar W. Effect of carbetocin,
a long-acting oxytocin analog on the postpartum uterus.
Clin Pharmacol Ther 1992;52:60-7. Crossref
6. Voon HY, Suharjono HN, Shafie AA, Bujang MA.
Carbetocin versus oxytocin for the prevention of
postpartum hemorrhage: a meta-analysis of randomized
controlled trials in cesarean deliveries. Taiwan J Obstet
Gynecol 2018;57:332-9. Crossref
7. Kalafat E, Gokce A, O’Brien P, et al. Efficacy of carbetocin
in the prevention of postpartum hemorrhage: a systematic
review and Bayesian meta-analysis of randomized trials. J
Matern Fetal Neonatal Med 2019 Sep 19. Epub ahead of
print. Crossref
8. Onwochei DN, Van Ross J, Singh PM, Salter A, Monks DT.
Carbetocin reduces the need for additional uterotonics
in elective Caesarean delivery: a systematic review, meta-analysis
and trial sequential analysis of randomised
controlled trials. Int J Obstet Anesth 2019;40:14-23. Crossref
9. Mavrides E, Allard S, Chandraharan E, et al. Prevention
and management of postpartum haemorrhage. Green-top
Guideline No. 52. BJOG 2016;124:e106-49. Crossref
10. Leduc D, Senikas V, Lalonde AB. No. 235–Active
management of the third stage of labour: prevention and
treatment of postpartum hemorrhage. J Obstet Gynaecol
Can 2018;40:e841-55. Crossref
11. El Behery MM, El Sayed GA, El Hameed AA, Soliman BS,
Abdelsalm WA, Bahaa A. Carbetocin versus oxytocin for
prevention of postpartum hemorrhage in obese nulliparous
women undergoing emergency cesarean delivery. J Matern
Fetal Neonatal Med 2016;29:1257-60. Crossref
12. Chen CY, Su YN, Lin TH, et al. Carbetocin in prevention of
postpartum hemorrhage: experience in a tertiary medical
center of Taiwan. Taiwan J Obstet Gynecol 2016;55:804-9. Crossref
13. Mohamed Maged A, Ragab AS, Elnassery N, Ai Mostafa W,
Dahab S, Kotb A. Carbetocin versus syntometrine for prevention of postpartum hemorrhage after cesarean
section. J Matern Fetal Neonatal Med 2017;30:962-6. Crossref
14. Borruto F, Treisser A, Comparetto C. Utilization of
carbetocin for prevention of postpartum hemorrhage after
cesarean section: a randomized clinical trial. Arch Gynecol
Obstet 2009;280:707-12. Crossref
15. Chen YT, Chen SF, Hsieh TT, Lo LM, Hung TH. A
comparison of the efficacy of carbetocin and oxytocin
on hemorrhage-related changes in women with cesarean
deliveries for different indications. Taiwan J Obstet
Gynecol 2018;57:677-82. Crossref
16. Seow KM, Chen KH, Wang PH, Lin YH, Kwang JL.
Carbetocin versus oxytocin for prevention of postpartum
hemorrhage in infertile women with twin pregnancy
undergoing elective cesarean delivery. Taiwan J Obstet
Gynecol 2017;56:273-5. Crossref
17. Demetz J, Clougueur E, D’Haveloose A, Staelen P, Ducloy AS,
Subtil D. Systematic use of carbetocin during cesarean
delivery of multiple pregnancies: a before-and-after study.
Arch Gynecol Obstet 2013;287:875-80. Crossref
18. Abbas AM. Different routes and forms of uterotonics for
treatment of retained placenta: methodological issues. J
Matern Fetal Neonatal Med 2017;30:2179-84. Crossref
19. Elfayomy AK. Carbetocin versus intra-umbilical oxytocin
in the management of retained placenta: a randomized
clinical study. J Obstet Gynaecol Res 2015;41:1207-13. Crossref
20. Kato S, Tanabe A, Kanki K, et al. Local injection of
vasopressin reduces the blood loss during cesarean section
in placenta previa. J Obstet Gynaecol Res 2014;40:1249-56. Crossref
21. Elbohoty AE, Mohammed WE, Sweed M, Bahaa Eldin AM,
Nabhan A, Abd-El-Maeboud KH. Randomized controlled
trial comparing carbetocin, misoprostol, and oxytocin
for the prevention of postpartum hemorrhage following
an elective cesarean delivery. Int J Gynaecol Obstet
2016;34:324-8. Crossref