Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
EDITORIAL
Prevention of postpartum haemorrhage
WC Leung, MD, FHKAM (Obstetrics and Gynaecology)
Department of Obstetrics and Gynaecology, Kwong Wah Hospital, Hong Kong
Corresponding author: Dr WC Leung (leungwc@ha.org.hk)
Postpartum haemorrhage (PPH) is an important
cause of maternal morbidity and mortality.
Prevention is always better than treatment. In this
issue of Hong Kong Medical Journal, Tse et al1 have
compared the use of carbetocin with oxytocin
infusion in reducing the need for additional
uterotonics or procedures in women at increased
risk for PPH undergoing Caesarean deliveries in
a single Hospital Authority (HA) obstetric unit.
Carbetocin was better than oxytocin infusion in
reducing the requirement of additional uterotonics
or procedures in pregnant women undergoing
Caesarean sections with multiple pregnancies or
major placenta praevia. The findings echo the first of
the three recommendations from the territory-wide
HA survey on massive PPH conducted in 2013.2 3
With the objectives of studying the
characteristics of patients with massive primary PPH
(defined as ≥1500 mL within the first 24 hours after
delivery, which is the clinical indicator for obstetric
performance in HA hospitals) and exploring areas for
improvement in terms of prevention and treatment,
a prospective study2 3 was conducted during the
year 2013 in all the eight HA obstetric units using
a pre-designed code sheet to record the details of
all patients with massive primary PPH, including
causes, risk factors, mode of delivery, interventions
(uterotonic agents, second-line therapies and
emergency hysterectomy), use of blood products,
and maternal outcome.
Massive primary PPH occurred in 0.76%
(n=277) of all deliveries (n=36 510) in HA obstetric
units in 2013. The incidence was comparable to those
reported in international literature. The majority
occurred after Caesarean sections (84.1%). Uterine
atony (37.5%), placenta praevia/accreta (49.9%),
and uterine wound bleeding/tear during Caesarean
section (24.2%) were the three most common causes.
The median total blood loss was 2000 mL (range,
1500-20 000 mL). Coagulopathy occurred in 16.2%
(n=45). A quarter (n=76, 27.4%) required intensive
care or high dependent unit admission. There was no
maternal mortality.
Second-line therapies (balloon tamponade,
compression sutures and uterine artery/internal
iliac artery embolisation or surgical ligation) were
used in 40.1% (n=111). Emergency hysterectomy
was required in 8.7% (n=24). A total of 1052 units of
packed cells, 670 units of platelets, 568 units of fresh frozen plasma, and 200 units of cryoprecipitate were
transfused.
The study identified three areas for
improvement: (1) to increase the choice of uterotonic
agents (carbetocin has been incorporated into HA
Drug Formulary since January 2017, mainly for
prevention of PPH in women at risk such as twin
pregnancy, large fibroids, polyhydramnios, fetal
macrosomia, and placenta praevia. In 2017, a total of
875 ampoules have been used in HA obstetric units,
rising to 2500 ampoules in 2018, and 2865 ampoules
in 2019); (2) to step up the use (and early use) of
second-line therapies, and to watch out for failures
from second-line therapy; (3) to reduce the incidence
of placenta praevia/accreta through education and
to improve its management at multiple care levels.
Carbetocin is a long-acting synthetic analogue
of oxytocin indicated for prevention of uterine
atony after Caesarean section. It is administered as
a slow intravenous injection over 1 minute, with a
rapid onset of uterine contraction within 2 minutes
and lasting for several hours. It is also a heat-stable
compound which does not require refrigeration.
Latest Cochrane reviews showed that carbetocin
may have some additional benefits compared with
oxytocin and appears to be without an increase in
adverse effects.4 The Carbetocin HAeMorrhage
PreventION (CHAMPION) trial5 showed that
carbetocin was non-inferior to oxytocin for the
prevention of PPH after vaginal delivery as well.
The main disadvantage of using carbetocin
in preventing PPH is its cost, making it much less
cost-effective when compared with other uterotonic
drugs.6 For local reference, carbetocin (single dose
of 100 μg) costs HK$200, as compared with oxytocin
(40 IU infusion, HK$32), syntometrine (single
dose, HK$27), and misoprostol (800 μg, HK$7).
As a result, when carbetocin was introduced into
HA Drug Formulary in 2017, we have limited its
use to those women with high-risk factors for PPH
after Caesarean sections such as twin pregnancy,
large fibroids, polyhydramnios, fetal macrosomia,
and placenta praevia. For example, in 2018, only
2500/35 016 or 7.1% of all deliveries in HA had
carbetocin for PPH prophylaxis when compared
with around 90% of deliveries in private hospitals
in Hong Kong. There is capacity to increase the use
of carbetocin in HA by including more women with
risk factors for PPH such as prolonged induction of labour (eg, oxytocin ≥12 hours), high parity (eg,
≥para 3), history of PPH, and others. These risk
factors have not been included in Tse et al’s study.1
Carbetocin should not only be considered for
Caesarean sections, but also for vaginal deliveries
with same risk factors for PPH. Furthermore, the
role of using carbetocin as treatment for PPH could
be explored.
In addition to single-centre studies on the
efficacy of a single drug or procedure on the
prevention and treatment of PPH, further studies are
required on the overall impact of the introduction
of uterotonic drugs such as carbetocin; non-uterotonic
drugs such as tranexamic acid; increasing
use of second-line procedures7 such as balloon
tamponade, compression sutures and uterine artery
embolisation; and new patient blood management
such as intravenous iron therapy, particularly in the
current era of inadequate blood donation, being
further aggravated by coronavirus disease 2019
(COVID-19).
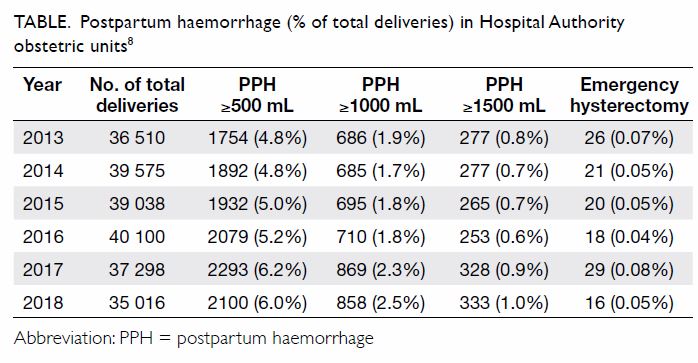
Interestingly, with all the new modalities of
prevention and treatment of PPH, the overall figures
of primary PPH ≥500 mL (traditional definition),
≥1000 mL or ≥1500 mL (defined as massive PPH),
including emergency hysterectomies for massive
PPH, have not been improved in HA from 2013
to 2018 (Table).8 This phenomenon is different
from what had been observed in a single obstetric
unit over a different time period from 2006 to
2011.9 Fortunately, maternal mortality is still rare.
Further studies are definitely indicated to look into
the territory-wide HA data (using the Obstetrics
Clinical Information System) to see whether the new
modalities are not as effective as they are expected
to be or our pregnant population is indeed becoming
more and more high risk for PPH.
Author contributions
The author contributed to the manuscript, approved the
final version for publication, and takes responsibility for its
accuracy and integrity.
Conflicts of interest
The author has disclosed no conflicts of interest.
References
1. Tse KY, Yu FN, Leung KY. Comparison of carbetocin and oxytocin infusions in reducing the requirement
for additional uterotonics or procedures in women at
increased risk for postpartum haemorrhage following
Caesarean section. Hong Kong Med J 2020;26:382-9. Crossref
2. Lau KW, Chan LL, Lo TK, Lau WL, Leung WC; Hospital
Authority COC Obstetrics and Gynaecology Quality
Assurance Subcommittee. Territory-wide massive primary
postpartum haemorrhage (PPH >1,500ml) survey in
Hospital Authority obstetric units with recommendations
and the way forward. Hospital Authority Convention 2017.
Master Class 7.1. Available from: http://www3.ha.org.hk/haconvention/hac2017/ebook/HAC2017_abstract%20day%201.pdf. Accessed 29 Sep 2020.
3. Leung WC. An overview on massive postpartum
haemorrhage in Hong Kong. The Hong Kong Medical
Diary 2019;24(7):2-3.
4. Gallos ID, Papadopoulou A, Man R, et al. Uterotonic agents
for preventing postpartum haemorrhage: a network meta-analysis.
Cochrane Database Syst Rev 2018;(12):CD011689. Crossref
5. Widmer M, Piaggio G, Nguyen TM, et al. Heat-stable
carbetocin versus oxytocin to prevent hemorrhage after
vaginal birth. N Engl J Med 2018;379:743-52. Crossref
6. Pickering K, Gallos ID, Williams H, et al. Uterotonic drugs
for the prevention of postpartum haemorrhage: a cost-effectiveness
analysis. Pharmacoecon Open 2019;3:163-76. Crossref
7. Kellie FJ, Wandabwa JN, Mousa HA, Weeks AD.
Mechanical and surgical interventions for treating primary
postpartum haemorrhage. Cochrane Database Syst Rev
2020;(7):CD013663. Crossref
8. Hospital Authority Annual Obstetric Reports 2013 to 2018.
Available from: https://www.ekg.org.hk/html/gateway/neweKG/newsp/h1-obs-gyn.jsp (internal access via eKG).
9. Chan LL, Lo TK, Lau WL, et al. Use of second-line
therapies for management of massive primary postpartum
hemorrhage. Int J Gynaecol Obstet 2013;122:238-43. Crossref