Hong
Kong Med J 2020 Aug;26(4):350.e1–2
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
PICTORIAL MEDICINE
A common but often neglected source of emboli
SY Au, MB, BS, FHKAM (Medicine); KM Fong, MB, ChB, MRCP (UK); Jack KC Shek, MB, BS, FHKAM (Anaesthesiology); SK Yung, MB, BS, FHKAM (Medicine); George WY Ng, MB, BS, FHKAM (Medicine)
Intensive Care Unit, Queen Elizabeth Hospital, Hong Kong
Corresponding author: Dr SY Au (h0145237@gmail.com)
Case
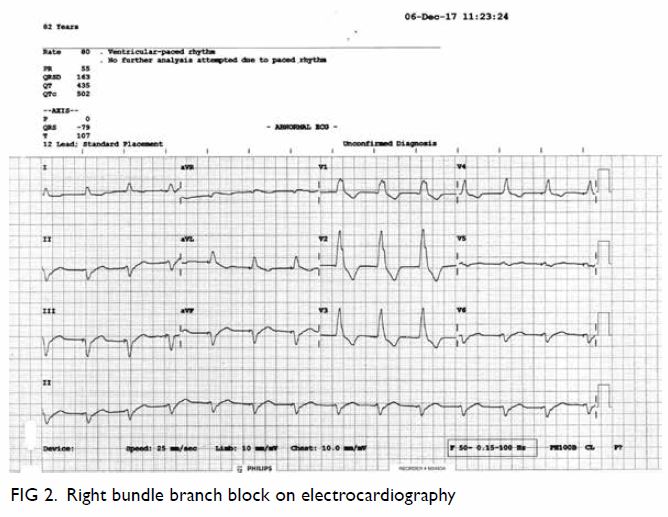
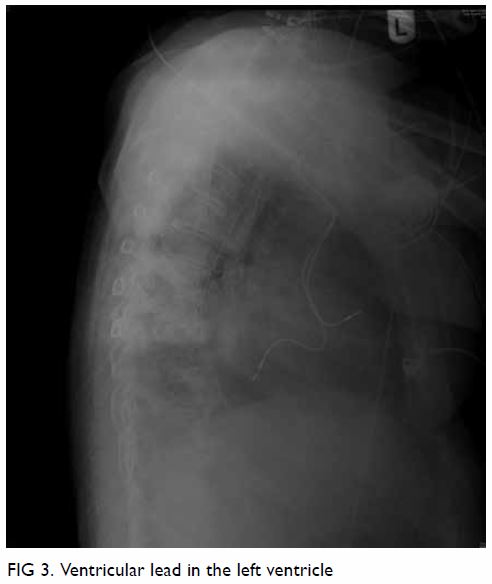
An 82-year-old woman was admitted to the intensive care unit with acute abdomen. She was initially admitted for chest infection but complained of sudden-onset abdominal pain and abdominal distension. She was confused with decreased consciousness. She had a medical history of sick sinus syndrome with dual-chamber pacing performed 4 years previously. She was being treated for hypertension but was prescribed neither aspirin nor anticoagulation. Initial investigations revealed an increased white cell count, coagulopathy, and deranged liver and renal function, with severe mixed respiratory and lactic acidosis. She was commenced on a high-dose dopamine infusion and was intubated prior to transfer to the intensive care unit. Further imaging investigations were performed. Abdominal plain radiograph showed dilated bowel and subsequent computed tomography of the abdomen confirmed diffuse bowel ischaemia (Fig 1). There was no abdominal aortic aneurysm. Computed tomography was also performed in view of her confusion and showed left middle cerebral artery infarction. Electrocardiography performed to identify cardiac causes of systemic embolisation revealed a paced rhythm of 80 beats per minute and right bundle branch block pattern (Fig 2). A lateral chest radiograph subsequently confirmed that the ventricular lead was in the left ventricle as it was pointing posteriorly (Fig 3). Transthoracic echocardiography showed no intracardiac clots but confirmed that the pacing lead was positioned in the left heart through the atrial septum. Transoesophageal echocardiography confirmed that the lead entered the left heart through a patent foramen ovale. The ischaemic bowel was too extensive and not amenable to surgery and the patient finally succumbed.
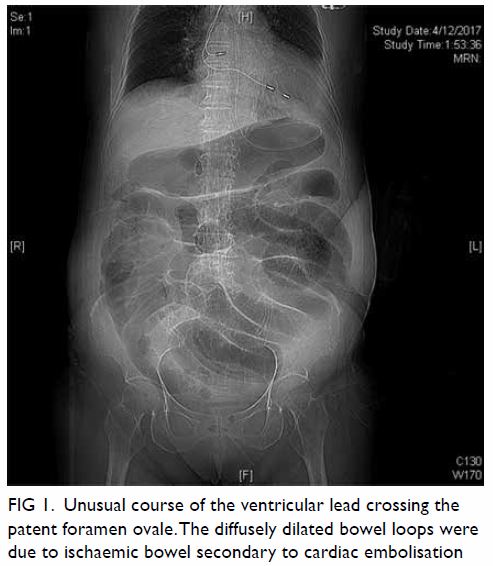
Figure 1. Unusual course of the ventricular lead crossing the patent foramen ovale.The diffusely dilated bowel loops were due to ischaemic bowel secondary to cardiac embolisation
Confirmation of placement of a pacing lead by a posterior-anterior chest radiograph can be difficult. A left bundle branch paced rhythm on echocardiography and a lateral radiograph that shows an anteriorly pointing ventricular lead help confirm placement of a pacing lead in the right ventricle. A pacing lead in the left ventricle and the absence of anticoagulation places a patient at risk of clot formation that may lead to systemic embolisation. In our patient, an intracardiac clot was not well demonstrated on either computed tomography or echocardiography, and 4 years had passed between pacemaker insertion and this systemic embolic episode. Only a probable, not a definite causal relationship could be established. We postulate that her chest infection may have impacted her clotting profile and resulted in this systemic embolic event.
Author contributions
Concept or design: All authors.
Acquisition of data: All authors.
Analysis or interpretation of data: SY Au.
Drafting of the manuscript: SY Au.
Critical revision of the manuscript for important intellectual content: All authors.
Acquisition of data: All authors.
Analysis or interpretation of data: SY Au.
Drafting of the manuscript: SY Au.
Critical revision of the manuscript for important intellectual content: All authors.
All authors had full access to the data, contributed to the study, approved the final version for publication and take responsibility for its accuracy and integrity.
Conflicts of interest
All authors have no conflicts of interest to disclose.
Funding/support
This pictorial medicine received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Ethics approval
The study was conducted in accordance with the Declaration of Helsinki. Consent for publication was obtained from the patient’sfamily.