Hong
Kong Med J 2020 Aug;26(4):348–9.e1–2
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
PICTORIAL MEDICINE
Vision loss due to ophthalmic artery occlusion
secondary to spontaneous internal carotid
artery dissection
Sunny CL Au, MB, ChB, AFCOphthHK1; Simon TC Ko, MB, BS, FHKAM (Ophthalmology)2
1 Department of Ophthalmology, Hong Kong East Cluster Ophthalmic
Service, Tung Wah Eastern Hospital, Hong Kong
2 Department of Ophthalmology, Tung Wah Eastern Hospital, Hong Kong
Corresponding author: Dr Sunny CL Au (kilihcua@gmail.com)
Case
A 47-year-old male smoker with hypertension,
diabetes mellitus, and hyperlipidaemia complained
of right eye vision loss on waking. His best-corrected
visual acuity was reduced to light perception only. Physical examination revealed anisocoria
without ptosis and no extraocular movement
deficit. The right eye pupil was larger than the
left, and the difference was more obvious under
a light environment. Direct and consensual pupil
reflexes were both present but there was a marked
right relative afferent pupillary defect. Slit lamp
examination revealed normal anterior segments
of the eyes, but a right pale optic disc without rim
thinning, and a typical cherry-red spot over the right
fovea surrounded by generalised whitened retina.
Vessels were not tortuous and no emboli were
seen nor retinal haemorrhage over different layers
(Figs 1 and 2). Left eye posterior segment was normal.
The patient also reported right-sided headache and
left-sided numbness. Thorough physical examination
revealed no other cranial nerve deficit or systemic
focal neurological deficit. Temporal pulse was easily
palpable and non-tender, and no carotid bruit was
heard. The patient worked on a construction site
and denied any trauma. He commenced hyperbaric
oxygen therapy but no improvement was observed.
Blood tests and brain imaging were all normal, but
carotid Doppler showed significant obstruction
>90% of the internal carotid artery, accounting
for the absence of bruit. Computed tomography
angiography confirmed dissection of a long segment
of the right internal carotid artery (Figs 3 and 4), not
amendable to stenting or bypass surgery. A diagnosis
of ophthalmic artery occlusion was made and
explained the ineffectiveness of hyperbaric oxygen
therapy due to choroidal ischaemia. Symptomatic
internal carotid artery dissection is a rare but major
cause of young-onset stroke, itself uncommon.1 Neck
trauma is a major aetiology, and there is a slight male
predominance with mean age of onset in the 40s.2
Apart from the neurological signs and symptoms of
stroke, the ophthalmological presentation of internal
carotid artery dissection is more similar to that of
painful Horner’s syndrome due to compression of
the adjacent third-order sympathetic chain fibres;
followed by cranial nerve palsy, caused by direct
local compression or compromise of feeder vessels.3
Ophthalmic artery occlusion is rare. Computed
tomography angiography has 80% sensitivity for
diagnosis and patients need to be closely monitored
for massive stroke that may occur weeks to months
after first presentation.4 Hyperbaric oxygen therapy
is indicated for central retinal artery occlusion, but not ophthalmic artery occlusion. It aims to reperfuse
the ischaemic retina with oxygen by diffusion from
the choroidal circulation, bypassing the obstructed
retinal vasculature. The choroidal arteries are
supplied by the posterior ciliary arteries that branch
from the ophthalmic artery. If the ophthalmic artery
is occluded, hyperbaric oxygen therapy has no means
to tackle the compromised posterior ciliary vessels.5
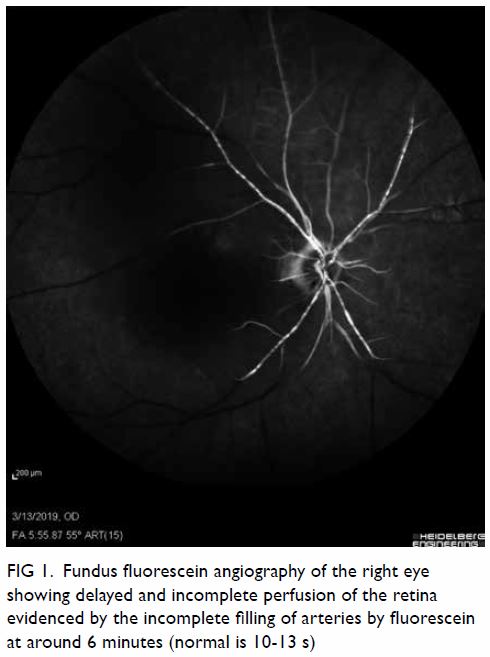
Figure 1. Fundus fluorescein angiography of the right eye showing delayed and incomplete perfusion of the retina evidenced by the incomplete filling of arteries by fluorescein at around 6 minutes (normal is 10-13 s)
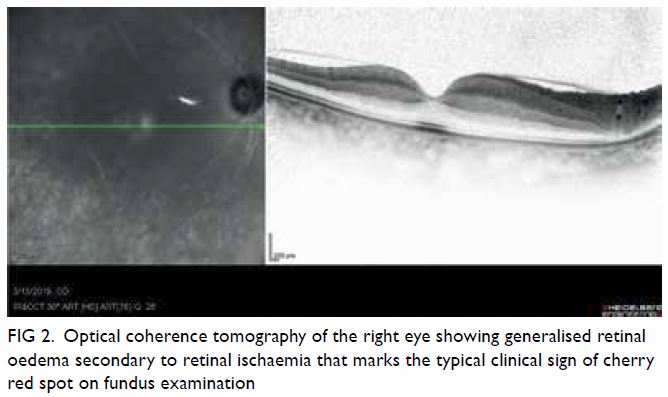
Figure 2. Optical coherence tomography of the right eye showing generalised retinal oedema secondary to retinal ischaemia that marks the typical clinical sign of cherry red spot on fundus examination

Figure 3. Three-dimensional computed tomography angiography showing the presence of left, but the absence of right internal carotid artery (indicated by white arrow) perfusion by contrast
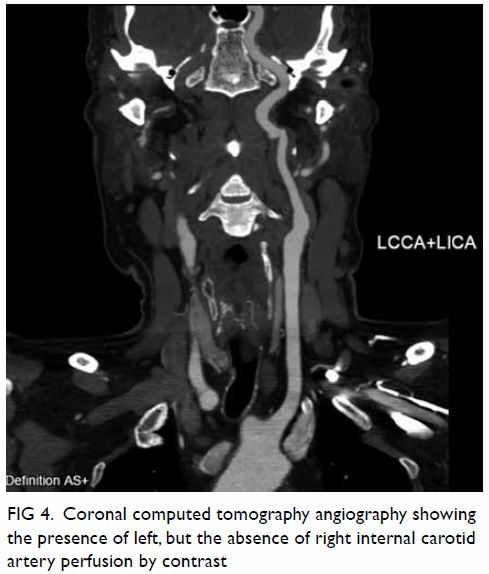
Figure 4. Coronal computed tomography angiography showing the presence of left, but the absence of right internal carotid artery perfusion by contrast
In conclusion, vision loss due to internal carotid
artery dissection is uncommon. Multidisciplinary
care is essential.
Author contributions
Concept or design: SCL Au.
Acquisition of data: SCL Au.
Analysis or interpretation of data: SCL Au.
Drafting of the manuscript: SCL Au.
Critical revision of the manuscript for important intellectual content: All authors.
Acquisition of data: SCL Au.
Analysis or interpretation of data: SCL Au.
Drafting of the manuscript: SCL Au.
Critical revision of the manuscript for important intellectual content: All authors.
All authors had full access to the data, contributed to the
study, approved the final version for publication, and take
responsibility for its accuracy and integrity.
Conflicts of interest
All authors have disclosed no conflicts of interest.
Funding/support
This pictorial medicine received no specific grant from any
funding agency in the public, commercial, or not-for-profit
sectors.
Ethics approval
This study was conducted in accordance with the principles
outlined in the Declaration of Helsinki. Relevant patient
consent was obtained for the purpose of this case study.
References
1. Thanvi B, Munshi SK, Dawson SL, Robinson TG. Carotid
and vertebral artery dissection syndromes. Postgrad Med
J 2005;81:383-8. Crossref
2. Blum CA, Yaghi S. Cervical artery dissection: a review
of the epidemiology, pathophysiology, treatment, and
outcome. Arch Neurosci 2015;2:e26670. Crossref
3. Kasravi N, Leung A, Silver I, Burneo JG. Dissection of
the internal carotid artery causing Horner syndrome and
palsy of cranial nerve XII. CMAJ 2010;182:E373-7. Crossref
4. Borgman CJ. Horner syndrome secondary to internal
carotid artery dissection after a short-distance endurance
run: a case study and review. J Optom 2012;5:209-16. Crossref
5. Kim SH, Cha YS, Lee Y, Kim H, Yoon IN. Successful
treatment of central retinal artery occlusion using
hyperbaric oxygen therapy. Clin Exp Emerg Med
2018;5:278-81. Crossref

