© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
CASE REPORT
Indocyanine green fluorescence-assisted
laparoscopic hepatectomy for hepatocellular
carcinoma in a pre-adolescent girl: a case report
Patrick HY Chung, MB, BS, FHKAM (Surgery); Kenneth SH Chok, MB, BS, FHKAM (Surgery); Kenneth KY Wong , MB, ChB, FHKAM (Surgery)
Department of Surgery, The University of Hong Kong, Hong Kong
Corresponding author: Dr Kenneth KY Wong (kkywong@hku.hk)
Case report
We present the case of a 9-year-old Chinese girl who presented with an incidental finding of elevated alkaline phosphatase (349 U/L) during a routine medical examination in 2018. Further blood test results were positive for hepatitis B. The patient was prescribed entecavir 0.5 mg daily and underwent regular liver ultrasound scans. After 6 months, a tumour at the right lobe of the liver was identified during routine scanning, and serum alpha-fetoprotein was elevated at 489 ng/mL. Further investigation with contrast computed tomography scan revealed a 3.8-cm × 5.0-cm tumour at segment 5 of the liver with radiological features compatible with hepatocellular carcinoma (HCC, Fig 1a). Liver function tests were normal (total bilirubin: 12 μmol/L, albumin 38 g/L, international normalised ratio:1.1). The patient’s body weight was 28 kg and her height was 128 cm.
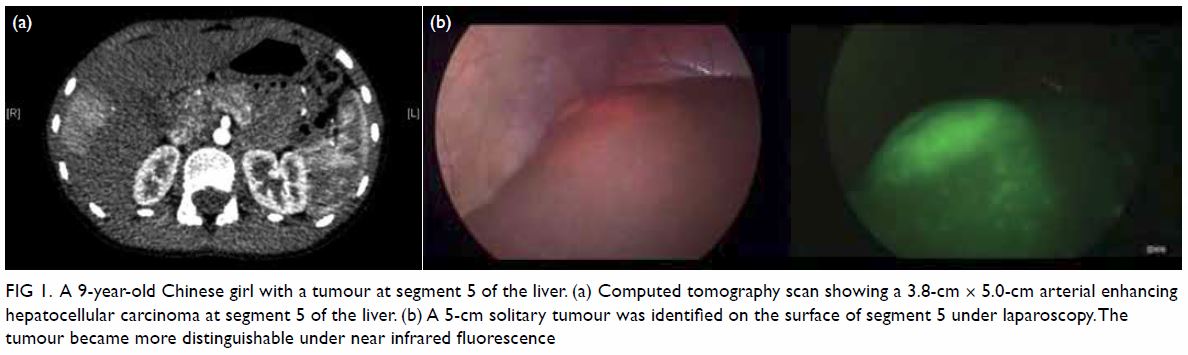
Figure 1. A 9-year-old Chinese girl with a tumour at segment 5 of the liver. (a) Computed tomography scan showing a 3.8-cm × 5.0-cm arterial enhancing hepatocellular carcinoma at segment 5 of the liver. (b) A 5-cm solitary tumour was identified on the surface of segment 5 under laparoscopy.The tumour became more distinguishable under near infrared fluorescence
Laparoscopic segment 5 resection was suggested. Intravenous indocyanine green (ICG) at a dosage of 0.5 mg/kg was administered 24 hours before surgery with no adverse effects. The following day, laparoscopic hepatectomy (LH) was performed under general anaesthesia. The patient was placed in a reverse Trendelenburg position with her right side mildly elevated and three 10-mm and two 5-mm abdominal ports created. Intra-operatively, a 5-cm solitary tumour was identified on the surface of segment 5 and it became more distinguishable under fluorescence (Fig 1b). Near-infrared fluorescence imaging and intra-operative ultrasound scan revealed no further tumours. The liver was not cirrhotic, and the surface was smooth. Guided by the fluorescent signal, a 1-cm resection margin was marked and hepatic transection performed using laparoscopic ultrasonic dissectors. The segmental branches of the hepatic vessels and bile ducts were controlled with non-absorbable polymer clips prior to division. The resected specimen was retrieved via a 5-cm Pfannenstiel incision. The operation was uneventful and lasted for 3 hours. Total blood loss was 30 mL and no blood products were required.
Postoperatively the patient was extubated and she was able to eat and drink on the same day. Wound pain was well controlled by oral paracetamol (15 mg/kg/dose) and she was transferred from the intensive care unit to a general ward the following day. She was able to walk on day 2 after surgery and made an uneventful recovery. She was discharged home on day 6 after surgery with normal liver function. Histological analysis of the resected liver confirmed the presence of a 5-cm moderately differentiated HCC with clear resection margins. The patient returned to school 14 days after surgery. Out-patient review at 3 months revealed healing of her surgical wounds with minimal scarring. The Pfannenstiel scar was not seen. Histological analysis of the resected specimen showed clear liver parenchymal and bile duct resection margins (Fig 2).
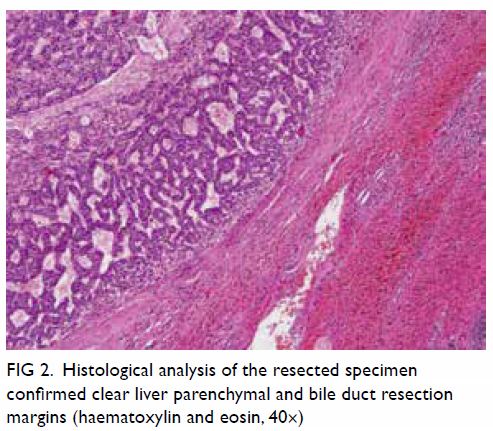
Figure 2. Histological analysis of the resected specimen confirmed clear liver parenchymal and bile duct resection margins (haematoxylin and eosin, 40×)
Discussion
Since the early 2000s, there have been significant advances in paediatric minimally invasive surgery owing to the availability of smaller-sized instruments as well as increasing technical expertise. However, the development of paediatric LH has advanced more slowly, even though it was first performed over 10 years ago in adults with proven benefit, especially in minor liver resection.1 Given the advantages of LH, including a smaller incision, less blood loss, early return of bowel function and rapid recovery, we believe this surgical approach should be extended to children with liver tumour. Our patient recovered quickly from her LH with only paracetamol required for pain control, largely due to the less invasive nature of the surgery. She was also able to resume her usual activities much earlier than usual for patients who underwent open hepatectomy. Although a Pfannenstiel incision was required, the small scars over the visible part of her abdomen would be more cosmetically acceptable to a young adolescent. Intra-operatively, conventional laparoscopic instruments are usually sufficient with no need for specialised equipment. The absence of liver cirrhosis and consequent minimal blood loss also favoured LH in our patient.
Of particular interest in this case was the use of ICG fluorescence for intra-operative tumour navigation. The ICG is a hydrosoluble molecule that has been used for the evaluation of hepatic function prior to liver resection. The clinical application of its fluorescent properties during HCC resection was first reported in 2009.2 Following intravenous injection, ICG is protein-bound and becomes fluorescent under infrared light. In the liver, ICG is taken up by normal hepatocytes and excreted in bile after 4 to 6 hours. However, in tumour cells, the excretion is inhibited and ICG will accumulate. Tumour tissue will thus remain fluorescent and this facilitates real-time identification of a primary tumour as well as any metastatic lesions under infrared light.3 The benefit of ICG fluorescence is more important during laparoscopic surgery since its fluorescent property compensates for the inability of LH to examine the whole liver in its absence. The tumour margin is also more obvious under ICG fluorescence imaging as the tumour appears much brighter. In addition, ICG fluorescence helps to differentiate a non-cancerous lesion detected by intra-operative ultrasound. Regarding the timing of injection, previous studies have suggested that it should be administered at least 48 hours before surgery to decrease the background fluorescence.4 In our case, the injection time was 24 hours before surgery but the fluorescent signal was still intense with good tumour-to-liver contrast. The exact timing for ICG injection remains undetermined. Normal hepatic function that promotes ICG excretion and that was present in our patient may have enabled the shorter time interval between injection and operation which in turn translated into a shorter hospitalisation.
In conclusion, LH is feasible in paediatric patients and should be considered as a surgical approach for children with liver cancer, especially when minor hepatectomy is required. It is associated with a speedier recovery after surgery with minimal scarring, both of which are important for the physical as well as psychosocial well-being of a growing child. Furthermore, ICG fluorescence is safe for use in children and provides an additional method to assist intra-operative tumour identification. The best timing of injection requires further study.
Author contributions
Concept or design: PHY Chung.
Acquisition of data: PHY Chung, KSH Chok.
Analysis or interpretation of data: PHY Chung.
Drafting of the manuscript: PHY Chung, KKY Wong.
Critical revision of the manuscript for important intellectual content: KSH Chok, KKY Wong.
Acquisition of data: PHY Chung, KSH Chok.
Analysis or interpretation of data: PHY Chung.
Drafting of the manuscript: PHY Chung, KKY Wong.
Critical revision of the manuscript for important intellectual content: KSH Chok, KKY Wong.
Conflicts of interest
As an editor of the journal, KKY Wong was not involved in the peer review process. Other authors have disclosed no conflicts of interest.
Acknowledgement
The authors would like to acknowledge Prof John Nicholls from the Department of Pathology, The University of Hong Kong for his valuable contribution in preparing Figure 2.
Funding/support
This case report received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Ethics approval
This study was approved by the hospital ethics committee and was carried out in accordance with the principles outlined in the Declaration of Helsinki. Consent from the patient and her mother were obtained. This report does not contain any information by which they could be identified.
References
1. Mirnezami R, Mirnezami AH, Chandrakumaran K, et al. Short- and long-term outcomes after laparoscopic and open hepatic resection: systematic review and meta-analysis. HPB (Oxford) 2011;13:295-308. Crossref
2. Gotoh K, Yamada T, Ishikawa O, et al. A novel image- guided surgery of hepatocellular carcinoma by indocyanine green fluorescence imaging navigation. J Surg Oncol 2009;100:75-9. Crossref
3. Souzaki R, Kawakubo N, Matsuura T, et al. Navigation surgery using indocyanine green fluorescent imaging for hepatoblastoma patients. Pediatr Surg Int 2019;35:551-7. Crossref
4. Ishizawa T, Fukushima N, Shibahara J, et al. Real-time identification of liver cancers by using indocyanine green fluorescent imaging. Cancer 2009;115:2491-504. Crossref

