Hong Kong Med J 2020 Jun;26(3):250–1.e1-2 | Epub 29 Apr 2020
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
PICTORIAL MEDICINE
Temporal changes in computed tomography of COVID-19 pneumonia with perilobular fibrosis
FH Ng, MB, ChB, FHKCR; SK Li, MB, ChB, FHKCR; YC Lee, MB, ChB, FHKCR; Johnny KF Ma, MB, BS, FHKCR
Department of Radiology, Princess Margaret Hospital, Hong Kong
Corresponding author: Dr FH Ng (ngphonehim@gmail.com)
As the designated tertiary referral centre for infectious diseases, Princess Margaret Hospital, Hong Kong, received the city’s first influx of patients diagnosed with coronavirus disease 2019 (COVID-19). In January 2020, a 57-year-old man with a history of travel to Wuhan, China, presented to Princess Margaret Hospital with a 4-day history of respiratory symptoms and fever. Laboratory studies showed lymphopoenia 0.7 × 109/L (reference range, 1.1-2.9 109/L) and elevated inflammatory markers. The patient’s C-reactive protein level was 33.2 mg/L (reference range, <5 mg/L) on the day of admission and peaked (123 mg/L) on day 3 after admission. The diagnosis of COVID-19 was made by the detection of severe acute respiratory syndrome coronavirus 2 RNA in a nasopharyngeal aspirate using reverse transcription polymerase chain reaction. High-resolution computed tomography (HRCT) images were acquired on days 2, 14, and 22 after admission. On day 2 after admission, HRCT showed peripheral subpleural ground-glass opacities (GGOs) and consolidation without zonal predominance in the absence of centrilobular nodules, pleural effusions, or lymph node enlargement, compatible with organising pneumonia,1 which correlated with the known radiological pattern of COVID-19 pneumonia.2
Concurrent with improvement of clinical symptoms and normalising inflammatory markers, serial HRCTs showed reduced GGOs (Fig 1). By day 22 after admission, the patient’s C-reactive protein level had normalised (5.3 mg/L). Instead of complete resolution, consolidations became curved or arched consolidation bands, with shaded margins, distributed around the structures surrounding the secondary pulmonary lobules. It was likely the result of perilobular inflammation and took the form of an arcade (Fig 2). This arcade-like sign is one of the typical features of perilobular fibrosis found in secondary organising pneumonia.3
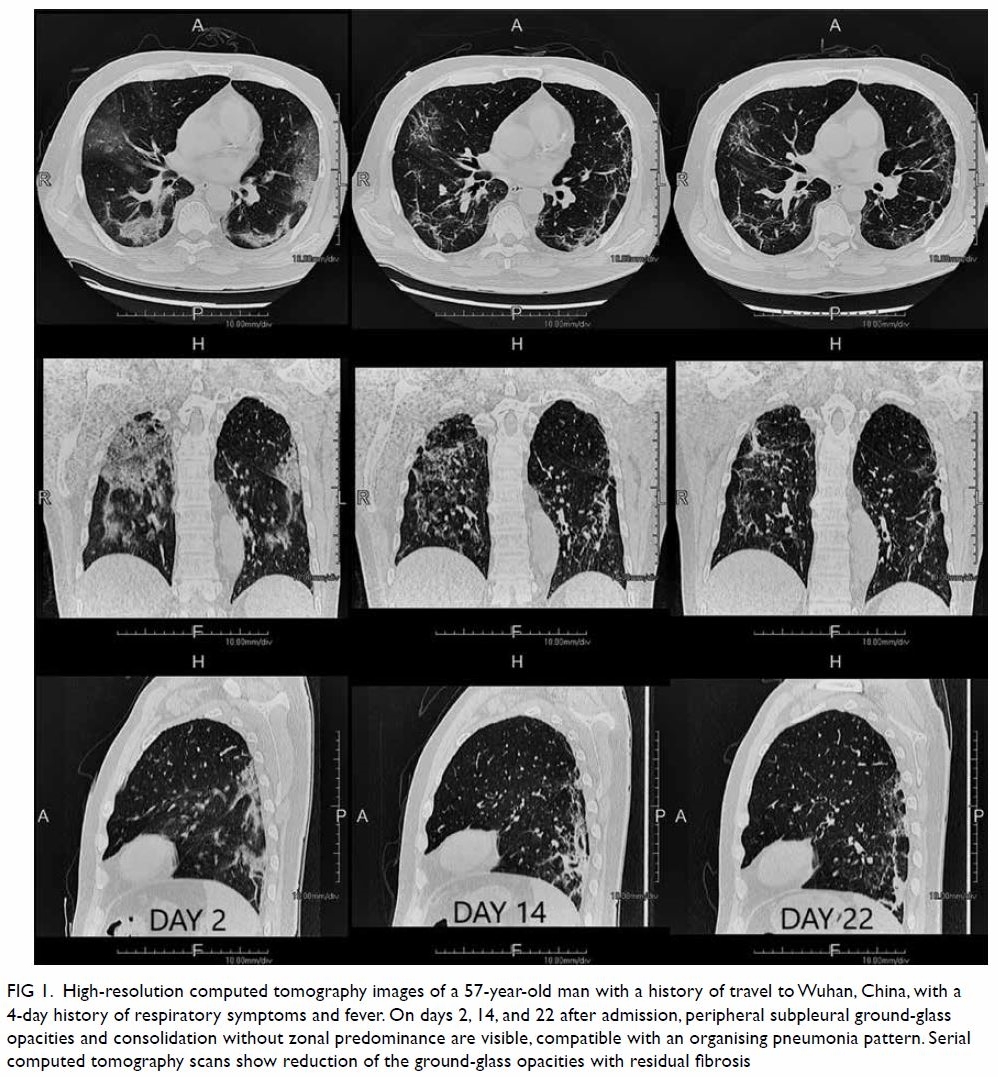
Figure 1. High-resolution computed tomography images of a 57-year-old man with a history of travel to Wuhan, China, with a 4-day history of respiratory symptoms and fever. On days 2, 14, and 22 after admission, peripheral subpleural ground-glass opacities and consolidation without zonal predominance are visible, compatible with an organising pneumonia pattern. Serial computed tomography scans show reduction of the ground-glass opacities with residual fibrosis
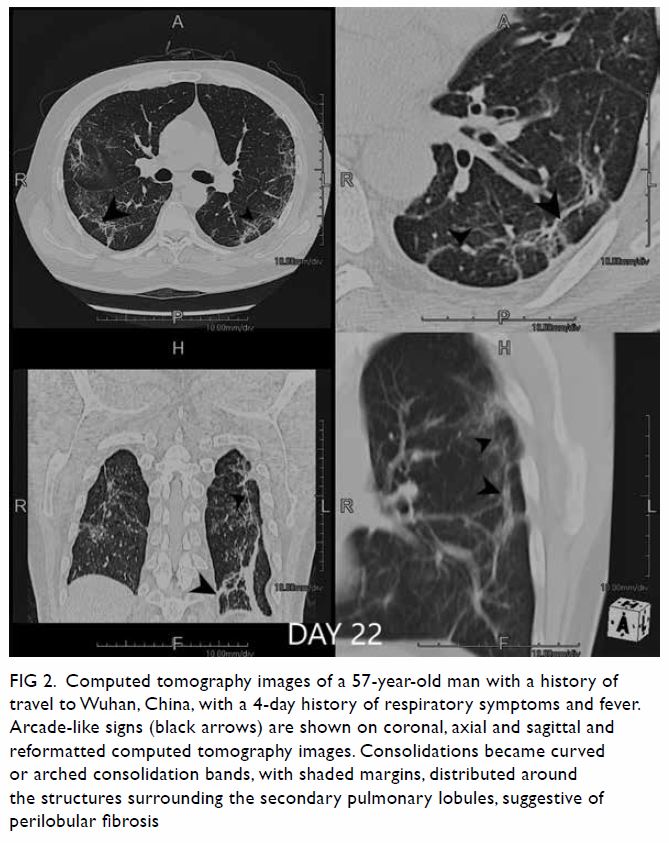
Figure 2. Computed tomography images of a 57-year-old man with a history of travel to Wuhan, China, with a 4-day history of respiratory symptoms and fever. Arcade-like signs (black arrows) are shown on coronal, axial and sagittal and reformatted computed tomography images. Consolidations became curved or arched consolidation bands, with shaded margins, distributed around the structures surrounding the secondary pulmonary lobules, suggestive of perilobular fibrosis
Residual GGOs with irregular lines and interfaces are the second most common pattern in COVID-19 pneumonia, suggesting the presence of secondary organising pneumonia, and hence pulmonary fibrosis.4 The gold standard to confirm pulmonary fibrosis requires lung biopsy or bronchoalveolar lavage, which are invasive. Lung biopsy was not performed in our case.
The present case highlights the computed tomography findings of pulmonary fibrosis, one of the sequelae of COVID-19 pneumonia.
Author contributions
All authors contributed to the concept or design of the study, acquisition of the data, drafting of the manuscript, and critical revision of the manuscript for important intellectual content. All authors had full access to the data, contributed to the study, approved the final version for publication, and take responsibility for its accuracy and integrity.
Conflicts of interest
All authors have disclosed no conflicts of interest.
Acknowledgement
We would like to express our gratitude to the Infectious Disease Team and “dirty team” physicians of Princess Margaret Hospital, Hong Kong, for their professional patient care and invaluable contribution to the understanding of a novel disease.
Funding/support
This pictorial medicine paper received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Ethics approval
This study was approved by the Kowloon West Cluster Research Ethics Committee (Ref 144-20). The patient provided written informed consent for all procedures and treatments.
References
1. Ujita M, Renzoni EA, Veeraraghavan S, Wells AU, Hansell DM. Organizing pneumonia: perilobular pattern at thin-section CT. Radiology 2004;232:757-61. Crossref
2. Chung M, Bernheim A, Mei X, et al. CT imaging features of 2019 novel coronavirus (2019-nCoV). Radiology 2020;295:202-7. Crossref
3. Chiarenza A, Ultimo LE, Falsaperla D, et al. Chest imaging using signs, symbols, and naturalistic images: a practical guide for radiologists and non-radiologists. Insights Imaging 2019;10:114. Crossref
4. Wang Y, Dong C, Hu Y, et al. Temporal changes of CT findings in 90 patients with COVID-19 pneumonia: A longitudinal study. Radiology 2020:200843. Crossref

