Hong Kong Med J 2020 Jun;26(3):176–83 | Epub 1 Jun 2020
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE
How are family doctors serving the Hong Kong
community during the COVID-19 outbreak? A survey of HKCFP members
Esther YT Yu, MB, BS, FHKAM (Family Medicine)1,2; Will LH Leung, FHKAM (Family Medicine), MScHSM (CUHK)1,3; Samuel YS Wong, MD, FHKAM (Family Medicine)1,4; Kiki SN Liu, BSc2; Eric YF Wan, PnD2,5; for the HKCFP Executive and
Research Committee
1 The Hong Kong College of Family Physicians, Hong Kong
2 Department of Family Medicine and Primary Care, The University of Hong Kong, Hong Kong
3 Department of Family Medicine and Primary Health Care, Kowloon West Cluster, Hospital Authority, Hong Kong
4 The Jockey Club School of Public Health and Primary Care, The Chinese University of Hong Kong, Hong Kong
5 Department of Pharmacology and Pharmacy, The University of Hong Kong, Hong Kong
Corresponding author: Prof Samuel YS Wong (yeungshanwong@cuhk.edu.hk)
Abstract
Introduction: This study evaluated the preparedness of family doctors during the early phase of the coronavirus disease 2019 (COVID-19) outbreak in Hong Kong.
Methods: All members of the Hong Kong College
of Family Physicians were invited to participate
in a cross-sectional online survey using a 20-item
questionnaire to collect information on practice
preparedness for the COVID-19 outbreak through
an email followed by a reminder SMS message
between 31 January 2020 and 3 February 2020.
Results: Of 1589 family doctors invited, 491 (31%)
participated in the survey, including 242 (49%) from
private sector. In all, 98% surveyed doctors continued
to provide clinical services during the survey period,
but reduced clinic service demands were observed
in 45% private practices and 24% public clinics.
Almost all wore masks during consultation and
washed hands between or before patient contact.
Significantly more private than public doctors
(80% vs 26%, P<0.001) experienced difficulties in
stocking personal protective equipment (PPE); more
public doctors used guidelines to manage suspected
patients. The main concern of the respondents was
PPE shortage. Respondents appealed for effective
public health interventions including border control,
quarantine measures, designated clinic setup, and public education.
Conclusion: Family doctors from public and private
sectors demonstrated preparedness to serve the
community from the early phase of the COVID-19
outbreak with heightened infection control measures
and use of guidelines. However, there is a need for
support from local health authorities to secure PPE
supply and institute public health interventions.
New knowledge added by this study
- The coronavirus disease 2019 (COVID-19) outbreak in Hong Kong resulted in reduced primary care service demands and abrupt shortage of personal protective equipment (PPE) among primary care clinics.
- The majority of surveyed Hong Kong family doctors consistently adopted facemask wearing and handwashing for infection control at their practice.
- Public health measures including border control, quarantine, and public education were advocated as important interventions to limit the spread of COVID-19.
- Family doctors in Hong Kong from both public and private sectors were willing and prepared to provide firstcontact clinical service to the community during the COVID-19 outbreak.
- Family doctors in Hong Kong needed better support from local health authorities on PPE supply, guided management of patients with COVID-19, greater availability of rapid diagnostic tests, and complementary public health interventions.
- Better coordination between public and private sectors is crucial, to include private family doctors as part of the overall health system strategy and emergency responses, because 70% of primary care consultations take place in the private sector in Hong Kong.
Introduction
Family doctors, serving as the first point of
professional contact for patients, are inevitably first
to identify probable cases of coronavirus disease 2019
(COVID-19) among the many patients presenting
with respiratory symptoms each day.1 Family doctors
in Hong Kong have experience in dealing with the
severe acute respiratory syndrome (SARS) epidemic
in 20032 3 and the H1N1 pandemic in 2009.4 5
However, their preparedness in handling another
outbreak of a novel infectious disease has not been
explored. Furthermore, Hong Kong has a dual-track
healthcare system in which 70% of primary medical
care, especially acute episodic care, is provided in the
private sector where practice settings and resources
vary and differ from those of public clinics.6 7 8 Family
doctors play a crucial role in the community to
offer first contact and coordinated care for patients,
and their preparedness, perceptions, and attitudes
towards COVID-19 are particularly important to
inform future strategies for responding to epidemics. Hence, the Hong Kong College of Family Physicians
(HKCFP) conducted an online survey among its
members to evaluate preparedness and to identify
clinic-related challenges of private and public family
doctors who were providing primary care services
during the early phase of the evolving COVID-19
outbreak in Hong Kong.
Methods
All family doctors who are HKCFP members were
invited to complete an online survey. The structured
questionnaire (online supplementary Appendix 1)
comprised 20 questions. Twelve closed-ended
questions assessed the effects of the COVID-19
outbreak (at the time of the survey, the World
Health Organization had not announced it as a
pandemic) on clinical services and the preparedness
of the responding family doctors, such as changes in
infection control practice. An open-ended question
invited respondents to express their concerns
towards the COVID-19 outbreak and suggest
measures that would facilitate their clinical practice.
The last seven questions collected demographics of
the respondents. The survey questions were modified
from a previous survey for primary care doctors
in Hong Kong and Canada9 10 and pilot-tested by
a panel of experienced academic family doctors
and HKCFP Research and Executive Committee
members. Invitation e-mails and short message
service reminders were sent to target participants
between 31 January 2020 and 3 February 2020.
Descriptive statistics were used to summarise
the characteristics of the respondents. Respondents
were stratified by their practice sector (ie, public
vs private). The differences in the effects of the
COVID-19 outbreak on the clinical practices, clinic
service, and infection control practices between
public and private family doctors were evaluated
by Pearson Chi squared test. Thematic analysis
was performed on the respondents’ free comments
and suggestions. The responses were reviewed
independently by two investigators and consolidated
into themes. Inconsistencies were resolved by
discussion between the two investigators to reach
consensus on a common theme. The consolidated
themes from the respondents’ suggestions and
concerns were further stratified by respondents’
practice sector using descriptive statistics.
All significance tests were two-tailed and those
with a P value of <0.05 were considered statistically
significant. The statistical analysis was executed by
Stata (Version 16.0; StataCorp LLC, College Station
[TX], US).
Since the survey was initially conducted to
examine the needs and preparedness of frontline
family doctors who are members of the HKCFP
during the early phase of COVID-19 outbreak in
Hong Kong, ethics approval was obtained from
the Survey and Behavioural Research Ethics
Committee of The Chinese University of Hong Kong
subsequently for data analysis and presentation.
The Strengthening the Reporting of
Observational Studies in Epidemiology (STROBE)
checklist for cross-sectional studies was used in the
drafting of this article.11
Results
Of 1589 HKCFP members invited to complete
the survey, 491 (31%) provided a complete and
valid response (Table 1). Of the respondents, 393
(80%) had attained higher qualifications in Family
Medicine. Among the respondents, 236 (48%)
worked at public primary care clinics operated by
the Hospital Authority or Department of Health,
and 242 (49%) worked in the private sector, half of
whom were solo practitioners. The ratio of public to
private sector respondents was approximately 1:1.
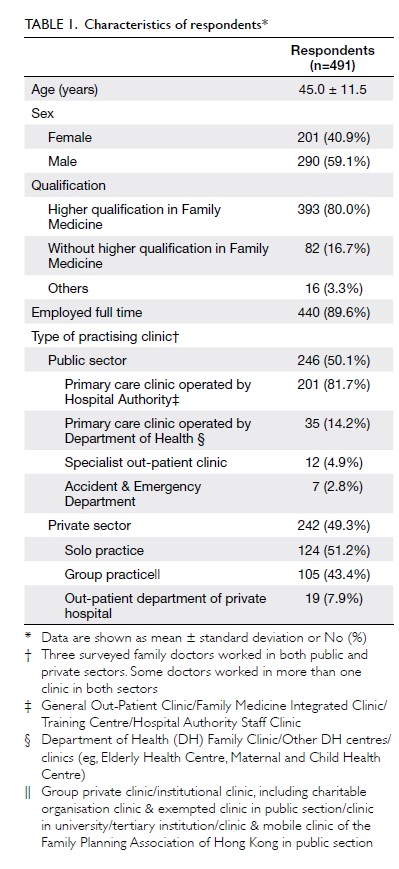
Effects of the COVID-19 outbreak on clinical
practices and regular clinic services
The vast majority of the respondents (n=482, 98%) continued to provide clinic services although most
of their clinic practices (n=428, 87%) had been
affected by the COVID-19 outbreak (Fig 1, online
supplementary Appendix 2). Significantly a higher
proportion of private than public family doctors
reported reduced clinic service demands during
this outbreak (n=111 [45%] vs n=60 [24%], P<0.001).
Half of the surveyed family doctors adjusted non-acute consultation services and/or reduced consultation time. As of 4 February 2020, over 140
patients with suspected severe acute respiratory
syndrome coronavirus 2 (SARS-CoV-2) infection
had been encountered by 70 (14%) surveyed family
doctors; one public family doctor reported
a patient who was subsequently confirmed to have
SARS-CoV-2 infection. Among the surveyed family
doctors, 310 (63%) perceived needs for more training
on how to deal with the COVID-19 outbreak. At time
of the survey, to assist clinical decision making for
diagnosing COVID-19, guidelines from the Centre
for Health Protection or the Hospital Authority
were used by public family doctors more frequently
than by private family doctors (n=143 [58%] vs
n=98 [40%], P<0.001). Conversely, 195 (80%) of
the surveyed private family doctors encountered
problems in stocking personal protective equipment
(PPE).
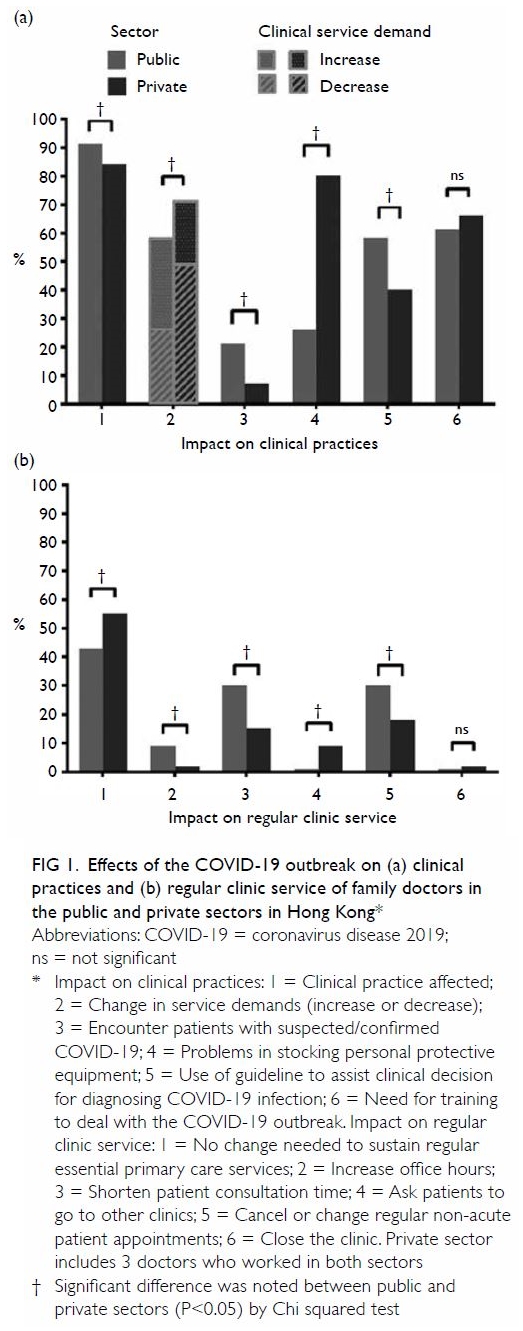
Figure 1. Effects of the COVID-19 outbreak on (a) clinical practices and (b) regular clinic service of family doctors in the public and private sectors in Hong Kong
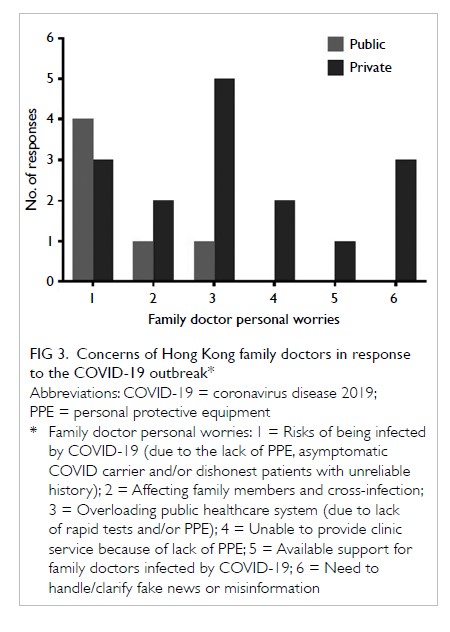
Changes in infection control practices in
response to the COVID-19 outbreak
Nearly all respondents wore masks during
consultations (n=490, 99%) and washed hands
between or before patient encounter (n=486, 99%)
[Fig 2 and Supplementary Appendix 2]. A greater
proportion of public than private family doctors
insisted patients wear masks during consultations
(n=210 [85%] vs n=165 [67%], P<0.001) and routinely
screened patients’ body temperatures (n=211 [86%]
vs n=183 [75%], P=0.002). In contrast, a greater
proportion of private than public family doctors
cleaned work surfaces with antiseptics at least once
a day (n=223 [91%] vs n=200 [81%], P=0.002) and
installed air purifiers (n=71 [29%] vs n=35 [14%],
P<0.001).
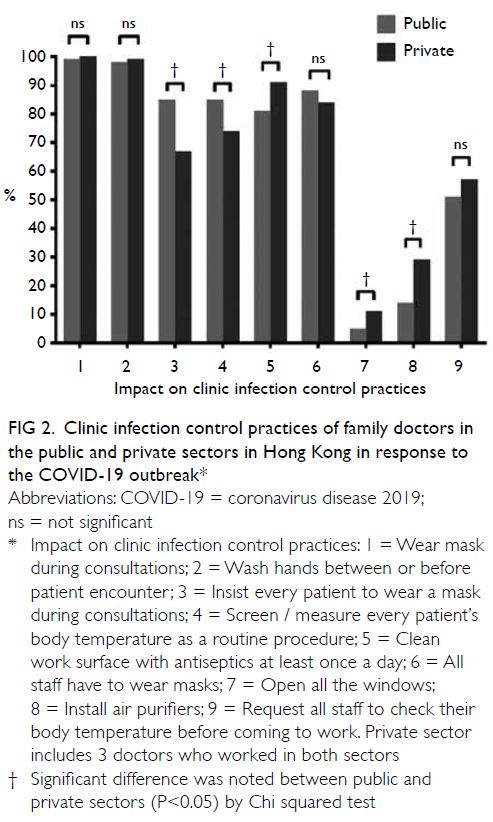
Figure 2. Clinic infection control practices of family doctors in the public and private sectors in Hong Kong in response to the COVID-19 outbreak
Suggested measures to respond to the
COVID-19 outbreak
Of the respondents, 159 (32%) answered the open-ended
question, among which 135 (85%) suggested
measures to be instituted by government and/or
local health authorities to facilitate frontline family
doctors to respond to the COVID-19 outbreak
(Table 2). A significant proportion of respondents
(n=52, 39%) appealed to the government, health
service providers and/or professional bodies for
securing adequate supply of PPE, especially surgical
masks, for frontline healthcare workers as well as the
general public. There was a strong call (n=49, 36%)
for more effective public health policy to contain the
outbreak, such as border control and/or quarantine
measures for returning residents and travellers to
reduce imported cases. Two respondents (1.5%)
had expectations for better coordination between
the public and private sectors with respect to role
delineation and resource allocation, for example,
setting up a Primary Care Authority to maximise efficiency and effectiveness of scattered primary
healthcare delivery locally. Some family doctors (n=9,
7%) advocated for the introduction of designated
clinics and requested availability of rapid diagnostic
tests. A few respondents (n=8, 6%) stressed the
importance of public education on infection control
practice and reporting accurate travel and contact
history during consultation.
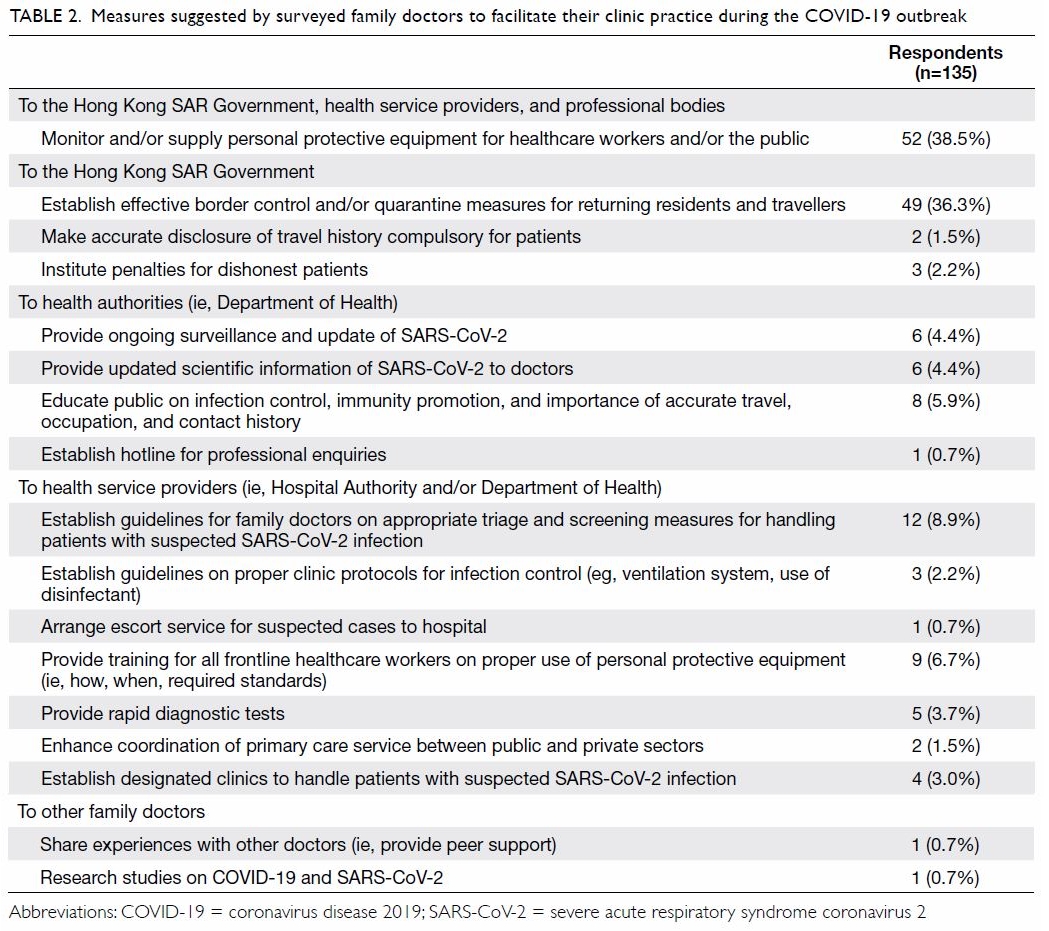
Table 2. Measures suggested by surveyed family doctors to facilitate their clinic practice during the COVID-19 outbreak
Concerns of Hong Kong family doctors in
response to the COVID-19 outbreak
Nineteen respondents (4%) expressed personal
concerns that were consolidated into six themes (Fig 3 and online supplementary Appendix 3). The major
concern was the risk of SARS-CoV-2 infection,
as a result of the lack of PPE, consultation with an
asymptomatic patient with SARS-CoV-2 infection,
or dishonest patients with unreliable history. Owing
to the lack of rapid tests and/or PPE, two private
family doctors (11%) worried that they would be
unable to provide clinic services, resulting in public
healthcare system overload. Three respondents
(16%) raised concerns about the need to handle
and/or clarify “fake news” (ie, misinformation).
Discussion
The vast majority of surveyed family doctors were
committed to discharging their duties in the early
phase of the COVID-19 outbreak despite clinical
uncertainties, psychological distress arising from
infectious risk to self and family, and corresponding
significant effects on clinical services. Only 2% of
the surveyed private family doctors had closed their
clinics, compared with 8% during the SARS epidemic
in 2003.9 These figures were also much lower than
reported absenteeism rates of healthcare workers
during influenza pandemics.12 13 14 In the 2009 H1N1
pandemic in 2009, 59% of local primary care doctors
reported higher demands in clinical services.4 In
contrast, in the present study, 25% of public family
doctors and 45% of private family doctors reported
reductions in clinical service demand. Different from
an influenza outbreak when primary care doctors are
tasked with providing confirmatory diagnostic tests
and antiviral treatment, rapid diagnostic tests were not readily accessible in the primary care setting at
time of our survey, and treatments for COVID-19 were available only in hospital settings. Patients
with highly probable SARS-CoV-2 infection were
sent directly to hospital isolation wards for further
management. Patients suspecting themselves to have
SARS-CoV-2 infection presented in large numbers
to emergency departments instead of primary care
clinics. Local citizens were also strongly encouraged
to practise social distancing, especially avoiding areas
of high contact risk, including clinics.15 Patients with
other non-urgent health needs might opt to delay their
clinic visits. Nevertheless, family doctors encountered
probable SARS-CoV-2 infection, especially patients
with milder, non-specific respiratory symptoms
and with less clear travel and/or contact history.
Thus, family doctors needed to remain vigilant in
identifying suspected cases in the community during
this period, while providing continuing care to other
patients with unrelated medical conditions, mental
health support for patients affected by the outbreak
and educating healthy patients.
Although the mode of transmission of
COVID-19 was not clearly understood in the early phase of outbreak, almost all surveyed family doctors
readily adopted standard droplet and contact
precautions, including wearing facemasks during
consultation and washing hands before and/or
between seeing patients as recommended by the
Centre for Health Protection of Hong Kong.16
Wearing facemask during consultation became
a common practice among family doctors in
Hong Kong since the global outbreak of SARS.4 9 17
Conversely, hand hygiene practices of family doctors
were less consistent and varied between 45% before
the H1N1 influenza epidemic4 to 70% during SARS
in 2003.9 In the present survey, 99% of family
doctors reported washing their hands before patient
encounters during the current outbreak, which has
been proven more effective than facemask wearing
alone in limiting the transmission of respiratory
infections.18 19 The practice of other recommended
infection control measures differed between public
and private family doctors, reflecting practical
challenges in their implementation. A particular
infection control challenge for local small-sized
clinics would be the required isolation of patients
with suspected SARS-CoV-2 infection, where an
extra single isolation room with or without negative
pressure, or even a designated isolation area >1 m
from the rest of the waiting area, was often
unavailable.16 To protect other patients from possible
cross-infection in clinics, respondents adjusted non-nonacute
patient appointments, shortened consultation
times to avoid crowding of patients in the clinic,
or divert patients to other clinics. Despite the
variations, these infection control measures might
be contributory to the zero-infection rate observed
among primary care providers in Hong Kong at the
time of the survey.
Many respondents considered public health
policies and interventions in response to the
COVID-19 outbreak to be important. There has
been an escalation of infection control responses
to the COVID-19 outbreak, especially wearing
of facemasks, in the healthcare20 and community
settings.21 Consequently, an acute shortage of
facemasks was experienced by respondents, similar
to the situation observed in the US.22 Echoing the
viewpoints of Australian general practitioners
towards influenza pandemic management, family
doctors from Hong Kong also considered that
government and health authorities should be
responsible for ensuring steady supply of PPE to
frontline healthcare workers and/or the public.23
A few surveyed family doctors commented that
they would cease to provide clinical service if PPE
became unavailable, owing to the high infection
risk. Moreover, a large proportion of respondents
advocated for border controls and quarantine
measures to limit cross-border transmission.24
Subsequently, border controls and mandatory
quarantine were implemented on people arriving
from mainland China in early February 2020,25 and
extended to travellers from most regions around the
globe in March 2020.26 These measures may have
contributed to the relatively slow rise in the number
of confirmed COVID-19 cases in Hong Kong.
Some private family doctors requested the
introduction of designated fever clinics for the
public, so that high-risk patients presenting with
fever and/or respiratory symptoms could be diverted
to a designated location and managed appropriately.
Such arrangements would be particularly important
for protecting the many small private clinics
which lack the capacity to properly isolate high-risk
patients. Designated clinics were successfully
implemented in Hong Kong during the 2009 H1N1
pandemic5 and in China and the US during the
current COVID-19 outbreak.1 22 Unfortunately,
local citizens opposed these clinics owing to a fear
of COVID-19 transmission in the neighbourhood.
Instead, designated doctors were assigned to attend
high-risk or febrile patients in certain public primary
care clinics. However, the arrangement was not clear
to the public nor frontline private family doctors and
symptomatic patients continued to seek care from
private family doctors. Despite repeated calls for
coordinated care or clear role delineation of family
doctors between public and private sectors at times
of outbreak, this has still not been achieved.5 9
Strengths and limitations of the study
This study had two key strengths. First, our survey
was conducted in the early phase of the COVID-19
outbreak, thus the survey rapidly captured the early
effects of an emerging outbreak on primary care
services and reflected the clinic preparedness and
needs of frontline family doctors in Hong Kong.
Second, our study covered family doctors from both
public and private sectors, allowing for comparison
between the two sectors. Possible service gaps in the
current dual-track primary healthcare system could
be readily identified to inform policy makers.
A major limitation of this study was the low
response rate, attributable to the relatively short
survey period. Although our response rate (31%) was
lower than previous similar surveys among family
doctors in Hong Kong during SARS (75%) and H1N1
pandemic (42%), the crude response rate was higher
(n=491, vs 137 and 126, respectively). However, our
respondents included only approximately 10% of the
doctors listed in the Primary Care Directory.27 Also,
only HKCFP members and fellows were targeted
in this survey. Hence, the sample might not be
representative of all primary care physicians in Hong
Kong. Lastly, as an observational study, reporting
bias existed.
Conclusion
Family doctors from both public and private sectors
in Hong Kong reported willingness and preparedness
to provide primary, continuous, and whole-person
care to the community from the early phase of the
COVID-19 outbreak. Despite limitations in clinic
physical settings and potential for PPE shortages,
most family doctors adopted standard precautions
and effectively protected themselves and the public
from cross-infection. Nevertheless, there is an obvious
need for health authorities to improve role delineation
and coordination between private and public primary
care services and to provide relevant support during
an outbreak, so that family doctors can continue to
play their various roles in the community under the
current dual-track primary healthcare system.
Author contributions
Concept or design: SYS Wong, EYT Yu, WLH Leung.
Acquisition of data: SYS Wong, EYT Yu, WLH Leung.
Analysis or interpretation of data: All authors.
Drafting of the manuscript: All authors.
Critical revision of the manuscript for important intellectual content: All authors.
Acquisition of data: SYS Wong, EYT Yu, WLH Leung.
Analysis or interpretation of data: All authors.
Drafting of the manuscript: All authors.
Critical revision of the manuscript for important intellectual content: All authors.
All authors had full access to the data, contributed to the study, approved the final version for publication, and take
responsibility for its accuracy and integrity.
Conflicts of interest
All authors have disclosed no conflicts of interest.
Acknowledgement
We would like to thank The Hong Kong College of Family
Physicians (HKCFP) Research and Executive Committee
members who have contributed to the design of questionnaire
and review of the draft, including Dr Angus Chan, Dr David
Chao, Dr Catherine Chen, Dr Lap-kin Chiang, Dr Billy Chiu,
Dr Cecilia Fan, Dr Ho-lim Lau, Dr Jun Liang, Dr Shuk-yun
Leung, Dr Lorna Ventura Ng, Professor Martin Wong, and
Dr William Wong; and Miss Erica So, Miss Crystal Yung, and
Miss Angel Fung who provided administrative support for the
study. We would also like to thank all the participating family
doctors who responded promptly to this survey.
Declaration
This research has not been presented in any academic
conference or published previously. Part of the findings from
the survey was disseminated through a local press release on
10 March 2020.
Funding/support
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Funding/support
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Ethics approval
This study was approved by the Survey and Behavioural
Research Ethics Committee of The Chinese University of
Hong Kong (Ref SBRE-19-578).
References
1. Li DK, Zhu S. Contributions and challenges of general
practitioners in China fighting against the novel coronavirus
crisis. Fam Med Community Health 2020;8:e000361. Crossref
2. Zhong NS, Zheng BJ, Li YM, et al. Epidemiology and
cause of severe acute respiratory syndrome (SARS) in
Guangdong, People’s Republic of China, in February, 2003.
Lancet 2003;362:1353-8. Crossref
3. Tsang KW, Ho PL, Ooi GC, et al. A cluster of cases of
severe acute respiratory syndrome in Hong Kong. N Engl J
Med 2003;348:1977-85. Crossref
4. Wong SY, Kung K, Wong MC, et al. Primary care
physicians’ response to pandemic influenza in Hong Kong:
a mixed quantitative and qualitative study. Int J Infect Dis
2012;16:e687-91. Crossref
5. Lee A, Chuh AA. Facing the threat of influenza pandemic—roles of and implications to general practitioners. BMC
Public Health 2010;10:661. Crossref
6. Lee A. Seamless health care for chronic diseases in a dual
health care system: managed care and the role of family
physicians. J Manag Med 1998;12:398-405. Crossref
7. Working Party on Primary Health Care. Health for all, the
way ahead: Report of the Working Party on primary health
care. Hong Kong: Government Printer; 1990.
8. Wun YT, Lee A, Chan KK. Morbidity pattern in private and
public sectors of family medicine/general practice in a dual
health care system. Hong Kong Practitioner 1998;20:3-15. Crossref
9. Wong WC, Lee A, Tsang KK, Wong SY. How did general
practitioners protect themselves, their family, and staff
during the SARS epidemic in Hong Kong? J Epidemiol
Community Health 2004;58:180-5. Crossref
10. Wong SY, Wong W, Jaakkimainen L, Bondy S, Tsang
KK, Lee A. Primary care physicians in Hong Kong and
Canada—how did their practices differ during the SARS epidemic? Fam Pract 2005;22:361-6. Crossref
11. von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC,
Vandenbroucke JP; STROBE Initiative. The Strengthening
the Reporting of Observational Studies in Epidemiology
(STROBE) statement: guidelines for reporting
observational studies. Lancet 2007;370:1453-7. Crossref
12. Balicer RD, Omer SB, Barnett DJ, Everly GS, Jr. Local
public health workers’ perceptions toward responding to
an influenza pandemic. BMC Public Health 2006;6:99. Crossref
13. Ehrenstein BP, Hanses F, Salzberger B. Influenza pandemic
and professional duty: family or patients first? A survey of
hospital employees. BMC Public Health 2006;6:311. Crossref
14. Damery S, Wilson S, Draper H, et al. Will the NHS
continue to function in an influenza pandemic? A survey of
healthcare workers in the West Midlands, UK. BMC Public
Health 2009;9:142. Crossref
15. Fung CS, Yu EY, Guo VY, et al. Development of a Health
Empowerment Programme to improve the health of
working poor families: protocol for a prospective cohort
study in Hong Kong. BMJ Open 2016;6:e010015. Crossref
16. Ashton LM, Hutchesson MJ, Rollo ME, Morgan PJ, Collins
CE. Motivators and barriers to engaging in healthy eating
and physical activity. Am J Mens Health 2017;11:330-
43. Crossref
17. Wong CK, Yip BH, Mercer S, et al. Effect of facemasks on
empathy and relational continuity: a randomised controlled
trial in primary care. BMC Fam Pract 2013;14:200. Crossref
18. Cowling BJ, Chan KH, Fang VJ, et al. Facemasks and hand
hygiene to prevent influenza transmission in households:
a cluster randomized trial. Ann Intern Med 2009;151:437-
46. Crossref
19. Aiello AE, Murray GF, Perez V, et al. Mask use, hand
hygiene, and seasonal influenza-like illness among young
adults: a randomized intervention trial. J Infect Dis
2010;201:491-8. Crossref
20. Cheng VC, Wong SC, Chen JH, et al. Escalating infection
control response to the rapidly evolving epidemiology of
the coronavirus disease 2019 (COVID-19) due to SARS-CoV-2 in Hong Kong. Infect Control Hosp Epidemiol
2020;41:493-8. Crossref
21. Leung CC, Lam TH, Cheng KK. Mass masking in the COVID-19 epidemic: people need guidance. Lancet
2020;395:945. Crossref
22. Kamerow D. Covid-19: Don’t forget the impact on US
family physicians. BMJ 2020;368:m1260.Crossref
23. Shaw KA, Chilcott A, Hansen E, Winzenberg T. The GP’s
response to pandemic influenza: a qualitative study. Fam
Pract 2006;23:267-72. Crossref
24. Jefferson T, Foxlee R, Del Mar C, et al. Physical interventions
to interrupt or reduce the spread of respiratory viruses:
systematic review. BMJ 2008;336:77-80. Crossref
25. Viner R, Macfarlane A. Health promotion. BMJ
2005;330:527-9. Crossref
26. Magnussen CG, Koskinen J, Chen W, et al. Pediatric
metabolic syndrome predicts adulthood metabolic
syndrome, subclinical atherosclerosis, and type 2 diabetes
mellitus but is no better than body mass index alone: the
Bogalusa Heart Study and the Cardiovascular Risk in
Young Finns Study. Circulation 2010;122:1604-11. Crossref
27. Hong Kong SAR Government. Primary Care Directory.
Available from: https://apps.pcdirectory.gov.hk. Accessed
15 Mar 2020.