© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
CASE REPORT
Secondary organising pneumonia complicating
acute respiratory distress syndrome caused by
severe influenza A: a case report
Alwin WT Yeung, MB, BS, FHKAM (Medicine)1; Judianna SY Yu, MB, BS, MRCP1; Richard WC Wong, FHKCPath, FHKAM (Pathology)2
1 Department of Medicine and Geriatrics, Ruttonjee Hospital, Wan Chai, Hong Kong
2 Department of Clinical Pathology, Pamela Youde Nethersole Eastern Hospital, Chai Wan, Hong Kong
Corresponding author: Dr Alwin WT Yeung (yeungwt@ha.org.hk)
Case report
A 69-year-old man with a history of diabetes mellitus
and benign prostatic hypertrophy was admitted
to our medical unit with a 1-week history of fever,
runny nose, and shortness of breath. Chest X-ray
revealed bilateral diffuse ground glass opacities in
both lung fields. The patient had type 1 respiratory
failure and required non-invasive positive pressure
ventilation to maintain oxygenation. The patient was
given ceftriaxone 1 g every 12 hours, and doxycycline
100 mg and oseltamivir 75 mg twice daily. He was
transferred to the intensive care unit and intubated
due to severe acute respiratory distress syndrome
(ARDS). The patient’s nasopharyngeal swab was
tested by polymerase chain reaction and the result
was positive for influenza A virus H1 RNA. His
clinical course was further complicated by septic
acute kidney injury that necessitated continuous
venovenous haemofiltration. His lungs gradually
improved with supportive measures including prone
ventilation and muscle paralysis for 48 hours. The
fractional oxygenation requirement improved from
1.0 to 0.4 between day 1 and day 8 of admission and
chest X-ray showed improving aeration of both lungs.
Unfortunately, his ventilatory requirement
deteriorated again from day 9 onwards, with chest
X-ray showing new right upper zone and left middle
zone infiltrates (Fig 1). Repeat microbiological
investigation results were negative except for
Candida albicans and Candida species in the
endotracheal culture. Antibiotics were upgraded to
meropenem 500 mg every 8 hours. High-resolution
computed tomography of the thorax on day 14
showed patchy consolidation with air bronchogram
and ground glass opacities in both lungs, more
prominent in the right upper lobe, right lower
lobe, and left lower lobe, and mild bilateral pleural
effusions.
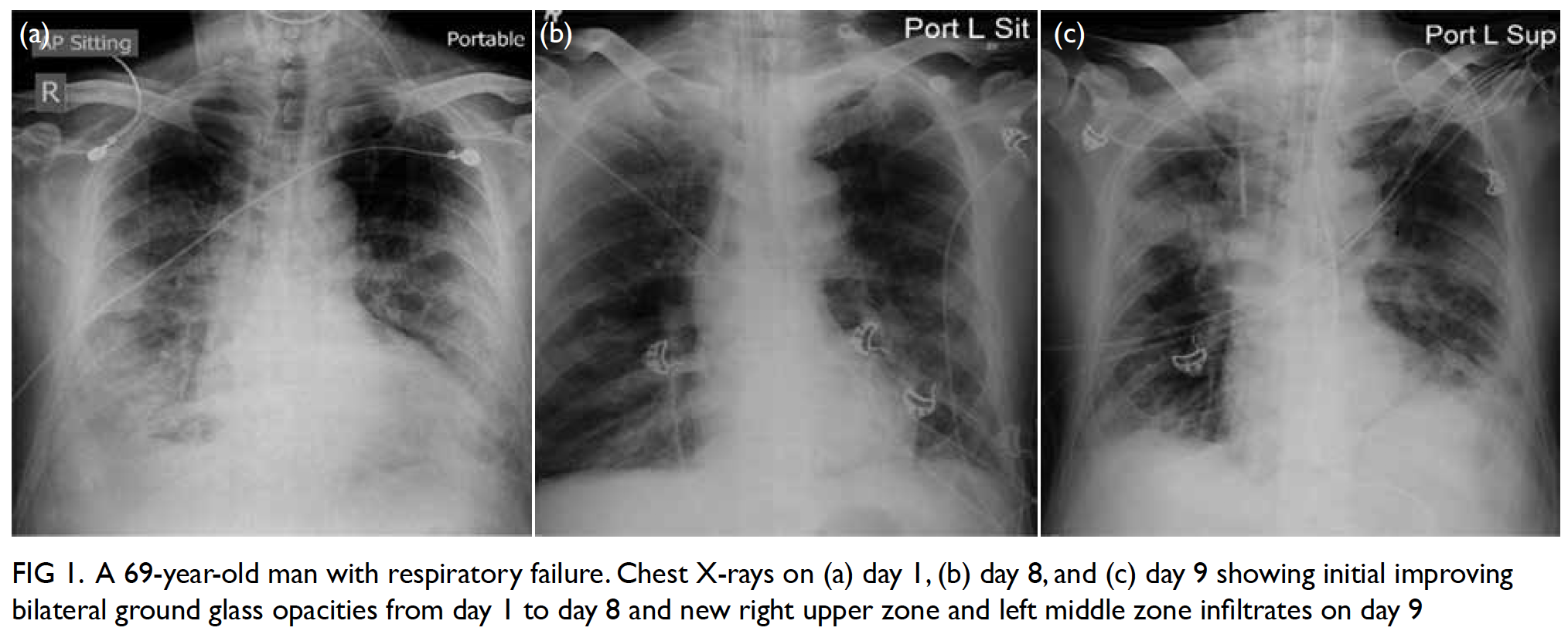
Figure 1. A 69-year-old man with respiratory failure. Chest X-rays on (a) day 1, (b) day 8, and (c) day 9 showing initial improving bilateral ground glass opacities from day 1 to day 8 and new right upper zone and left middle zone infiltrates on day 9
Bronchoscopy with transbronchial biopsy
of the apical segment of the left lower lobe was
performed uneventfully. Histological examination
of the biopsy specimen revealed alveolar lining
partially composed of cuboidal cells with foamy
cytoplasm, a variable degree of nuclear enlargement
and pleomorphism, and prominent nucleoli. The
histology could be suggestive of adenocarcinoma
with appropriate clinical settings. In view of the
unusual clinical course, it was decided to repeat transbronchial biopsies at different sites, namely at
the left lower lobe apical segment again on day 18
and the right upper lobe posterior segment on day
19. Both histological specimens revealed a pattern
compatible with organising pneumonia (OP) [Fig 2].
Intravenous hydrocortisone 100 mg every 8 hours
and subsequently enteral prednisolone 40 mg
daily were prescribed, and surgical tracheostomy
performed in view of the prolonged mechanical
ventilation.
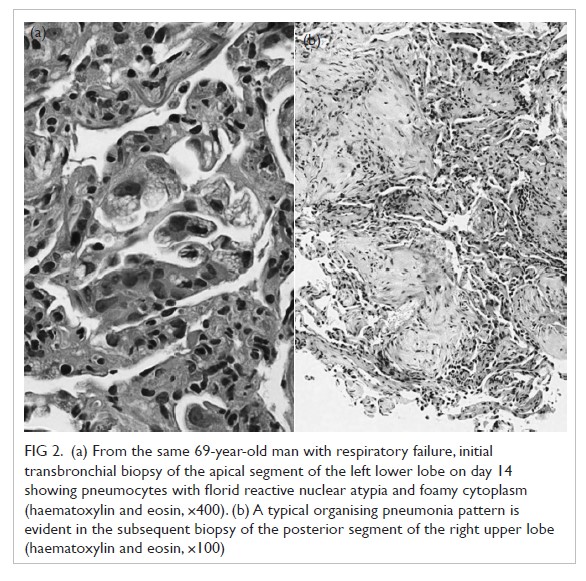
Figure 2. (a) From the same 69-year-old man with respiratory failure, initial transbronchial biopsy of the apical segment of the left lower lobe on day 14 showing pneumocytes with florid reactive nuclear atypia and foamy cytoplasm (haematoxylin and eosin, ×400). (b) A typical organising pneumonia pattern is evident in the subsequent biopsy of the posterior segment of the right upper lobe (haematoxylin and eosin, ×100)
The patient showed dramatic improvement
with steroid treatment. He was weaned off mechanical
ventilatory support and renal replacement therapy
and discharged from the intensive care unit on
day 22. He underwent rehabilitation in a general
ward and was weaned off tracheostomy and
supplementary oxygen. Serial chest X-rays showed
resolution of both lung consolidations with minimal
residual fibrotic scarring.
Discussion
In general, H1 influenza infection causes mild upper
respiratory tract symptoms. A minority of patients
present with ARDS secondary to viral pneumonia
with or without bacterial co-infection. Apart from
neuraminidase inhibitors such as oseltamivir,
management is mostly supportive. This includes
protective lung ventilation and a conservative fluid
management strategy. In moderate to severe ARDS
with partial pressure of oxygen/fraction of inspired
oxygen ratio <150 mm Hg, 48 hours of muscle paralysis, prone ventilation, and extracorporeal membrane oxygenation may be required.
The definition of ARDS includes acute onset
within 1 week, bilateral radiological opacities not
explained by pleural effusion or lung collapse,
respiratory failure not explained by heart failure,
or fluid overload with partial pressure of oxygen/fraction of inspired oxygen ratio <300 mm Hg under
a positive end-expiratory pressure of at least 5 cm
H2O. Typically, patients with ARDS exhibit diffuse
alveolar damage in histological specimens, divided
into an acute exudative phase shortly after the
pulmonary insult, followed by an organising phase,
with or without a final fibrotic phase. However, a
continuum and overlapping features exist, especially
late in the first week or if the patient has encountered
repeat pulmonary insults. The acute exudative phase
is characterised by hyaline membranes that gradually
disappear in the subsequent organising phase. The
organising phase is characterised by interstitial
fibrosis and pronounced type 2 pneumocyte
hyperplasia. Cytological atypia may be quite
pronounced and can be confused with malignancy,
as in our case.1 Subsequently, diffuse alveolar damage
will gradually resolve although some may progress
to a fibrotic phase with continued interstitial fibrosis
and compromises lung function.
Other histological patterns can present in
patients with ARDS, including OP and acute fibrinous
OP. In acute fibrinous OP, the alveolar spaces are
filled with organising fibrin balls instead of hyaline
membranes, whereas in OP, patchy accumulation of
intra-alveolar organising fibroblastic tissue primarily
centred around bronchioles is present.2
Organising pneumonia, acute fibrinous
OP, and diffuse alveolar damage are histological
manifestations arising from a broad range of
pulmonary insults. Temporal and regional
heterogeneity of the pulmonary parenchymal
alterations may result in diverse or mixed patterns
upon lung biopsy sampling. Corticosteroids remain
the first-line therapy in OP. Around two thirds
of patients with OP respond to treatment with
corticosteroids. However, the role of corticosteroids
in diffuse alveolar damage remains controversial.
The steroid response of acute fibrinous OP is
intermediate, between that of diffuse alveolar
damage and OP.3
To the best of our knowledge, few cases of post-influenza OP have been reported in the literature.4 5
Most were influenza A infection and patients
usually presented with refractory respiratory failure,
incomplete recovery, or new radiological infiltrate
after initial improvement. Most cases responded
well to corticosteroid therapy.
The present case demonstrates that OP can
complicate influenza-related ARDS. Physicians
should be aware of this possibility: timely confirmation by histological proof, exclusion of superimposed nosocomial pneumonia, and
initiation of corticosteroid therapy after balancing
the risks and benefits may result in a more favourable
outcome in the disease trajectory.
Author contributions
All authors contributed to the concept of study, acquisition and analysis of data, drafting of the manuscript, and had
critical revision of the manuscript for important intellectual
content. All authors had full access to the data, contributed to
the study, approved the final version for publication, and take
responsibility for its accuracy and integrity.
Conflicts of interest
All authors have disclosed no conflicts of interest.
Funding/support
This case report received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Ethics approval
The patient was treated in accordance with the Declaration of Helsinki. The patient verbally agreed publication of this
anonymous case report.
References
1. Butnor KJ. Avoiding underdiagnosis, overdiagnosis, and misdiagnosis of lung carcinoma. Arch Pathol Lab Med
2008;132:1118-32.
2. Beasley MB. The pathologist's approach to acute lung injury. Arch Pathol Lab Med 2010;134:719-27.
3. Bihari S, Bailey M, Bersten AD. Steroids in ARDS: to be or not to be. Intensive Care Med 2016;42:931-3. Crossref
4. Cornejo R, Llanos O, Fernández C, et al. Organizing pneumonia in patients with severe respiratory failure due
to novel A (H1N1) influenza. BMJ Case Rep 2010; 2010. pii:
bcr0220102708.Crossref
5. Asai N, Yokoi T, Nishiyama N, et al. Secondary organizing pneumonia following viral pneumonia caused by severe
influenza B: a case report and literature reviews. BMC
Infect Dis 2017;17:572. Crossref

