Hong Kong Med J 2020 Apr;26(2):120–6 | Epub 14 Apr 2020
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE
Brain death in children: a retrospective review of
patients at a paediatric intensive care unit
KL Hon, MB, BS, MD1,2; TT Tse3; CC Au, MB, BS, MRCPCH2; WS Lin3; TC Leung3; TC Chow3; CK Li, MB, BS, MD1,2; HM Cheung, MB, BS, MRCPCH1; SY Qian, MD4; Alexander KC Leung, MB, BS, MRCPC5
1 Department of Paediatrics, The Chinese University of Hong Kong, Prince of Wales Hospital, Shatin, Hong Kong
2 Department of Paediatrics and Adolescent Medicine, The Hong Kong
Children’s Hospital, Kowloon Bay, Hong Kong
3 Faculty of Medicine, The Chinese University of Hong Kong, Shatin, Hong
Kong
4 Pediatric Intensive Care Unit, Beijing Children’s Hospital, Capital Medical
University, National Center for Children, Beijing, China
5 Department of Paediatrics, The University of Calgary and The Alberta
Children’s Hospital, Calgary, Alberta, Canada
Corresponding author: Dr KL Hon (ehon@hotmail.com)
Abstract
Purpose: Among patients in paediatric intensive
care units (PICUs), death is sometimes inevitable
despite advances in treatment. Some PICU patients
may have irreversible cessation of all brain function,
which is considered as brain death (BD). This study
investigated demographic and clinical differences
between PICU patients with BD and those with
cardiopulmonary death.
Methods: All children who died in the PICU
at a university-affiliated trauma centre between
October 2002 and October 2018 were included in
this retrospective study. Demographics and clinical
characteristics were compared between patients
with BD and patients with cardiopulmonary death.
Results: Of the 2784 patients admitted to the
PICU during the study period, 127 died (4.6%).
Of these 127 deaths, 22 (17.3%) were BD and 105
were cardiopulmonary death. Length of PICU stay
was shorter for patients with cardiopulmonary
death than for patients with BD (2 vs 8.5 days,
P=0.0042). The most common mechanisms of injury
in patients with BD were hypoxic-ischaemic injury
(40.9%), central nervous system infection (18.2%),
and traumatic brain injury (13.6%). The combined
proportion of accident and trauma-related injury
was greater in patients with BD than in patients with
cardiopulmonary death (27.3% vs 3.8%, P<0.001).
Organ donation was approved by the families of four of the 22 patients with BD (18.2%) and was performed
successfully in three of these four patients.
Conclusions: These findings emphasise the
importance of injury prevention in childhood, as
well as the need for education of the public regarding
acceptance of BD and support for organ donation.
New knowledge added by this study
- This 16-year retrospective study compared demographic and clinical differences between patients with brain death and patients with cardiopulmonary death in a Hong Kong paediatric intensive care unit.
- Among 127 deaths, approximately one in five were brain death. Length of paediatric intensive care unit stay was shorter for patients with cardiopulmonary death than for patients with brain death.
- The most common mechanisms of injury in patients with brain death were hypoxic-ischaemic injury, central nervous system infection, and traumatic brain injury. The combined proportion of accident and trauma-related injury was greater in patients with brain death than in patients with cardiopulmonary death.
- Organ donation was approved by the families of four of the 22 patients with brain death (18.2%) and was performed successfully in three of these four patients.
- Family acceptance of the diagnosis of brain death may influence the length of paediatric intensive care unit stay. Without family acceptance of the diagnosis, physicians may be compelled to continue treatment for a patient with brain death.
- Education of the general public and early dialogue between the family and the attending physician are necessary to resolve common misconceptions regarding the biological and legal statuses of patients with brain death.
- Acceptance of the diagnosis of brain death may be associated with acceptance of organ donation and withdrawal of ventilator support, which may improve organ donation rates in Hong Kong.
Introduction
Despite advances in paediatric critical care
medicine, death remains inevitable in some
instances, due to various aetiologies.1 2 In paediatric
critical care medicine settings, patients who
would have otherwise died may be kept ‘alive’ by
advanced cardiovascular and ventilatory support.
Some patients on cardiopulmonary support may
experience irreversible cessation of all brain
function, which is regarded as brain death (BD).3 4 5 6
Because BD or cardiopulmonary death is equivalent
to death, there is no obligation for the physician to
provide further futile treatment.1 2 3 4 7 Nevertheless,
miraculous survivals have been reported in lay media
involving patients who were previously declared
BD or dead, which has created a mis-informed
understanding of BD.8 In this retrospective study,
all patients who underwent BD assessment over a
16-year period were evaluated to determine whether
survival occurred following BD assessment; the
demographics of patients diagnosed with BD were
compared with those of all other patients diagnosed
with cardiopulmonary death at a paediatric intensive
care unit (PICU). The null hypothesis was that there
would be no demographic or clinical differences
between patients diagnosed with BD and those
diagnosed with cardiopulmonary death.
Methods
Study population
All children admitted to the PICU of a university-affiliated
teaching hospital and trauma centre (Prince
of Wales Hospital) between October 2002 and
October 2018 were included in the study. The Prince
of Wales Hospital provides tertiary PICU service for
children, from birth to age 16 years, in the Eastern
New Territories of Hong Kong. The institutional
ethics committee approved this review and waived
the requirement for patient consent.
Data collection
The demographics and clinical characteristics of
deceased children were collected from the principal
author’s database (KLH), in which every PICU
admission was registered; data were also collected
retrospectively from the Clinical Management
System of the hospital. All deaths were reviewed,
including those of patients with clinical evidence
of BD who underwent BD assessment. Brain death
was defined as irreversible loss of all functions of
the brain, including the brainstem. The presence of
coma, absence of brainstem reflexes, and positive
apnoea test were essential findings for diagnosis of
BD. The diagnosis of BD was mainly clinical and
was made in accordance with the hospital’s standard
protocol for paediatric patients.4 9 Patients were
classified either as BD or cardiopulmonary death.
Statistical analysis
The demographics and clinical characteristics of
these two groups of patients were summarised as
median (interquartile range [IQR]) or as number
(percentage), and were compared using the Chi
squared test, Fisher’s exact test, or Mann-Whitney U
test, as appropriate. Patient characteristics included
age, sex, length of PICU stay (time from PICU
admission to withdrawal of ventilator support), and
diagnoses associated with PICU admissions. The
GraphPad Prism 6 software (GraphPad Software,
La Jolla [CA], US) and SPSS (Windows version
19.0; IBM Corp, Armonk [NY], US) were used for
statistical analysis. All comparisons were two-tailed,
and P values <0.05 were considered statistically
significant.
Results
Patient characteristics
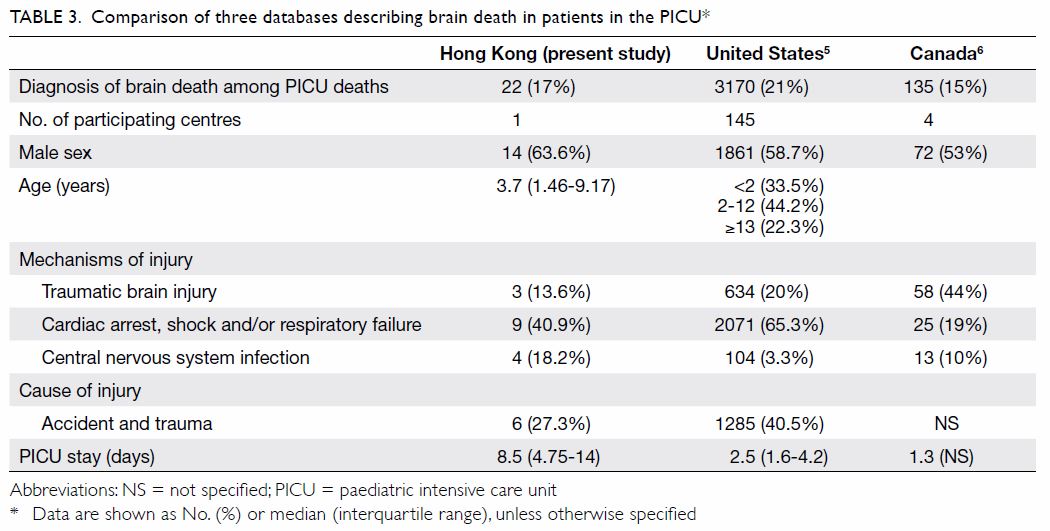
Of the 2784 children admitted to the PICU, 127
(4.6%) died in the PICU (Table 1). All but seven
children were of Chinese ethnicity. There were 73
boys (57.5%) and 54 girls (42.5%); the median age was
3.2 years (IQR: 0.94-7.34 years). Most patients had
not previously been admitted to the PICU (n=103,
81%), and most patients were aged >1 year (74.8%).
Of the 127 patients who died, BD assessments were
performed for 22 (17.3%) patients who had clinical
evidence of BD; all 22 patients were diagnosed
with BD. The remaining 105 (82.7%) patients were
diagnosed with cardiopulmonary death.
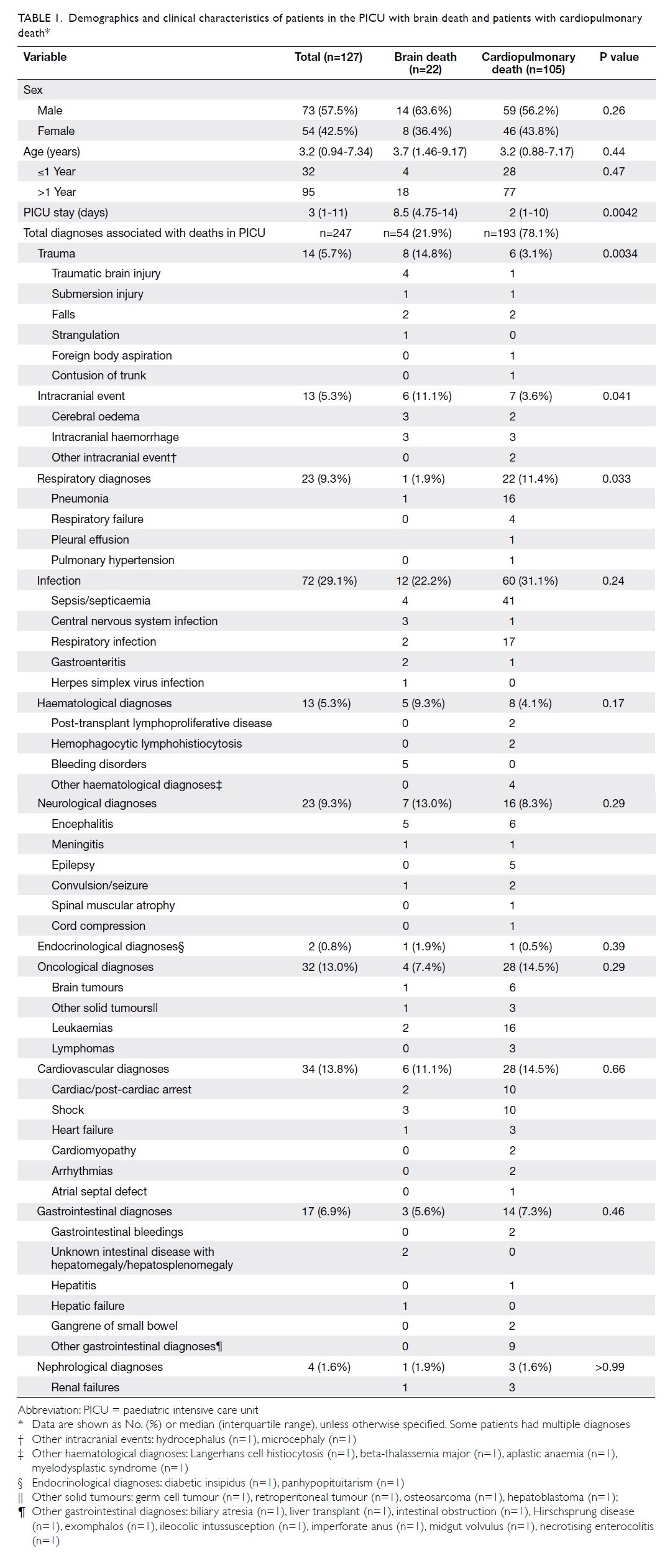
Table 1. emographics and clinical characteristics of patients in the PICU with brain death and patients with cardiopulmonary death
Factors associated with brain death and
cardiopulmonary death in patients in
paediatric intensive care unit
Comparison of the two groups showed that
length of PICU stay was significantly longer for
patients with BD (8.5 days; IQR: 4.75-14 days)
than for patients with cardiopulmonary death
(2 days; IQR: 1-10 days; P=0.004). The two groups
shared similar demographics. The most common
diagnoses associated with death in the PICU were
infections (29.1% of patients), oncological diagnoses
(13.0%), and cardiovascular diagnoses (13.8%)
[Table 1]. Comparison of the two groups showed
that trauma (P=0.003) and intracranial events (P=0.041) were more common in patients with BD, whereas respiratory diagnoses (P=0.033) were more
common in patients with cardiopulmonary death.
With respect to the cause of injury, the combined
proportion of accident and trauma-related injury
was greater in patients with BD than in patients with
cardiopulmonary death (27.3% vs 3.8%, P<0.001).
Among patients with BD, the most common
mechanisms of brain injury were hypoxic-ischaemic
injury (eg, cardiac arrest, shock, and/or respiratory
failure), central nervous system infection, and
traumatic brain injury (Table 2). Organ donation was
approved by the families of four of the 22 patients
with BD (18.2%) and was performed successfully in
three of these four patients.
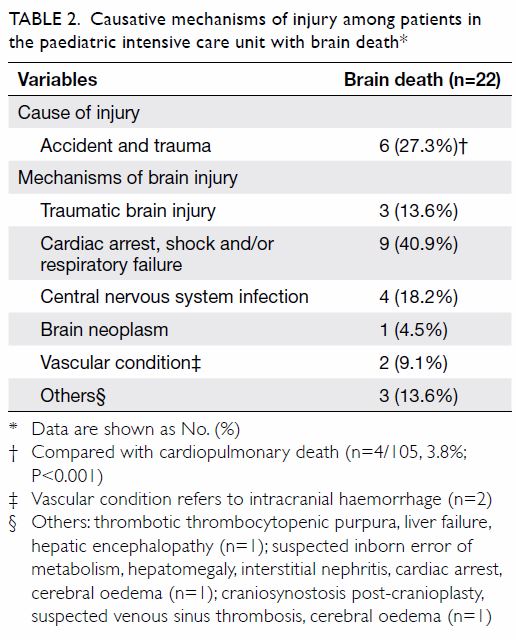
Table 2. Causative mechanisms of injury among patients in the paediatric intensive care unit with brain death
Brain death in patients aged <2 years
Our local guideline for BD determination does
not include patients aged <2 years. Nevertheless,
we found no difference in the proportion of
patients aged <2 years between the BD (n=7) and
cardiopulmonary death groups (n=42) [31.8% and
40%, P=0.47]. There was a non-significant trend
towards greater use of ancillary tests (eg, radionuclide
cerebral perfusion scan or electroencephalography)
for BD determination in patients aged <2 years,
compared with patients aged >2 years (85.7% and 53.3%, P=0.19). The United Kingdom guidelines
recommend that ancillary tests are not required in
infants from gestational age of 37 weeks to 2 months
after birth.10 None of the patients were within this
age range in our study.
Family acceptance of the diagnosis of brain
death
Family acceptance of the diagnosis of BD may
have influenced the length of PICU stay in our
study. Among patients with documented family
acceptance of the diagnosis of BD, the time interval
from BD to withdrawal of ventilator support was
0.5 days (range, 0-1.5 days; n=10). This interval was
prolonged among patients with documented family
resistance of the diagnosis of BD (median, 8 days;
range, 5-16 days; n=5, P=0.005); three of the five
patients’ families eventually accepted withdrawal
of ventilator support, whereas the remaining two
patients remained on ventilator support and lapsed
into cardiac arrest after 16 days and 66 days.
Discussion
Brain death demographics and survival
Over this 16-year period, BD assessment was only
performed in 22 (17.3%) patients who had clinical
signs of BD; all 22 patients were confirmed to have
BD. Notably, patients with BD had longer length of
PICU stay and a greater combined proportion of
accident and trauma-related injury, while patients
with cardiopulmonary death had a greater frequency
of respiratory diagnoses. In the present study, the
percentage of patients with BD in the PICU was
comparable to the numbers of patients with BD in
two large reports (one from the US and the other
from Canada; Table 3).5 6 Accident and trauma-related injury led to one in four diagnoses of BD in
our study, whereas the proportions of accident and
trauma-related injury, as well as traumatic brain
injury, were higher in the US and Canada.
Brain death and evaluation
Guidelines for BD assessment vary in terms of the
numbers of examinations, numbers and types of
physicians, time intervals between examinations,
and use of ancillary tests.11 12 In general, if BD is
suspected, two physicians (neither of whom would
be involved in organ harvesting from the patient)
should perform two sets of brainstem examinations,
at least 6 hours apart to ensure sufficient observation
time. A single apnoea test should also be performed.
If the results of these tests are positive, the patient
can then be declared legally and clinically BD.1 2 3 4
Before these examinations, conditions that may
confound the clinical diagnosis of BD should be
excluded.1 2 3 4 11 12 Absence of the pupillary reflex to
direct and consensual light, as well as the absence
of corneal, cough, and gag reflexes, support the
clinical diagnosis of BD. The calorie test can aid in
determining the integrity of the oculovestibular
reflex. A positive result consists of the absence of eye
deviation when ice water is irrigated into an external
auditory canal. The apnoea test is performed after
the second examination of brainstem reflexes; only
a single apnoea test is needed. Before the apnoea
test is performed, the physician must confirm that
the patient is not hypothermic, is euvolemic, and
has normal arterial pressure of carbon dioxide
and pressure of oxygen levels. The patient should
then be connected to a pulse oximeter and the
ventilator should be disconnected. Concurrently,
100% O2 is delivered into the trachea at 6 L/min. A
patient with BD may exhibit systolic blood pressure
<90 mm Hg, significant oxygen desaturation, or
cardiac arrhythmia. If respiratory movements are
absent and the arterial pressure of carbon dioxide
is ≥60 mm Hg, the apnoea test result is considered
positive. If the patient is very unstable and an apnoea
test might not be tolerated, or if the results of the
apnoea test are inconclusive, physicians may opt
for other neuro-diagnostic options (eg, four-vessel
cerebral angiography, radionuclide cerebral perfusion
scan, and/or electroencephalography). A lack of
blood perfusion to the brain and lack of electrical
activity would support a diagnosis of BD.
Implications for management of patients with
brain death in the paediatric intensive care
unit
The length of PICU stay was longer for patients
with BD than for patients with cardiopulmonary
death; this differed from the trends observed in the
US and Canada (Table 3).5 6 As noted in the Results,
family acceptance of the diagnosis of BD may have influenced the length of PICU stay in our study.
Unfortunately, not all stakeholders understand or
accept the implications of a diagnosis of BD. In our
experience, the reasons for the family’s resistance
might be two-fold. First, it might be emotionally
difficult to accept the death of a loved one, when the
child is apparently ‘breathing’ and appears physically
‘well’ when ventilatory support is provided. Second,
the family might have confused persistent vegetative
state with BD3 4; notably, patients with persistent
vegetative state have intact brainstem function, while
patients with BD have an irreversible loss of brainstem
function. In such instances of confusion, families may
wish to wait for the patient’s ‘miraculous revival’.1 13 14 15 16 While the acknowledgement of BD as biological
death may be counterintuitive to the public, there
is a need to emphasise and accept that BD is legal
death.17 Thus, public education is necessary to resolve
common misconceptions regarding the biological
and legal statuses of patients with BD.18 Notably,
among university students in Hong Kong, improved
knowledge has been shown to promote acceptance
of the withdrawal of ventilator support following
BD.19 From a physician’s perspective, withdrawal of
ventilator support for patients with BD should not be
regarded as withdrawal of life support; in addition,
continued use of ventilator support that allows a
patient to lapse into cardiac arrest is not a suitable
option. Prolonged and unnecessary treatment in the
PICU prevents other critically ill patients from using
the PICU service; it also constitutes ineffective use
of scarce medical resources. Abuse of PICU beds is
undesirable because medical resources in the public
sector are extremely competitive and limited.20
Further studies regarding physician counselling skills
and family acceptance of the diagnosis of BD may
improve resource utilisation.
Medical professionals should closely monitor
aetiologies that can lead to BD and consider
discussions with affected patients’ families at an early
stage of medical treatment. These early discussions
would allow more time for families to comprehend
the implications of a BD assessment and potential
positive test results. In a previous study, we found
that prolonged length of PICU stay was associated
with a Do-Not-Attempt-Resuscitation order, which
was placed in nearly half of our PICU deaths; this
finding implied that patients’ families often need
considerable time to accept the end-of-life decision
when futility of medical treatment becomes evident.1
Family acceptance of the diagnosis of BD is critical
for successful management of such situations. If
family acceptance is not achieved, physicians may
become involved in a conflict with the family, which
results in an ethical dilemma regarding the need
to continue treatment for a patient with BD. For
example, one patient in the present study remained
in the PICU for 66 days due to this difficult situation. Communication to identify common values and
establish options based on objective criteria may
resolve potential disputes and allow physicians and
families to reach agreements before, during, and after
BD assessment.21
Implications for organ donation
A practical aspect of BD assessment involves its
implications for the organ donation process. Four
of 22 patients’ families opted for organ donation;
notably, all four families also accepted the diagnosis
of BD. Successful donations of liver or kidneys
were made from three patients. Acceptance of the
diagnosis of BD may be associated with acceptance
of organ donation and withdrawal of ventilator
support.19 Support for organ donation, which was
initiated by the organ transplant coordinator, had
avoided potential instances of conflict. Acceptance of
the diagnosis of BD could be a factor, in combination
with other cultural and religious beliefs, for the lower
organ donation rate than that observed in Western
countries.12
Conclusions
In this study, one in five PICU deaths were BD. Acute
hypoxic-ischaemic injury was the most common
mechanism of brain injury; moreover, accident and
trauma-related injuries were the cause of injury in
one quarter of patients with BD. Diagnosis of BD
was associated with significantly longer PICU stay.
Notably, the organ donation rate was suboptimal.
These findings emphasise the importance of injury
prevention in childhood, as well as the need for
education of the public regarding acceptance of BD
and support for organ donation.
Author contributions
Concept or design: KL Hon.
Acquisition of data: KL Hon, CC Au, TT Tse, WS Lin, TC Leung, TC Chow.
Analysis or interpretation of data: KL Hon, CC Au, TT Tse, WS Lin, TC Leung, TC Chow, AKC Leung.
Drafting of manuscript: KL Hon, CC Au, TT Tse, WS Lin, TC Leung, TC Chow.
Critical revision of the manuscript for important intellectual content: KL Hon, CC Au, CK Li, HM Cheung, SY Qian, AKC Leung.
Acquisition of data: KL Hon, CC Au, TT Tse, WS Lin, TC Leung, TC Chow.
Analysis or interpretation of data: KL Hon, CC Au, TT Tse, WS Lin, TC Leung, TC Chow, AKC Leung.
Drafting of manuscript: KL Hon, CC Au, TT Tse, WS Lin, TC Leung, TC Chow.
Critical revision of the manuscript for important intellectual content: KL Hon, CC Au, CK Li, HM Cheung, SY Qian, AKC Leung.
All authors have full access to the data, contribute to the
study, approve the final version for publication, and take
responsibility for its accuracy and integrity.
Conflicts of interest
As an editor of the journal, KL Hon was not involved in the
peer review process. Other authors have no conflicts of
interest to disclose.
Funding/support
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Ethics approval
The Joint Chinese University of Hong Kong–New Territories
East Cluster Clinical Research Ethics Committee approved
this review (CREC Ref. No. 2016.116).
References
1. Hon KL, Poon TC, Wong W, et al. Prolonged non-survival
in PICU: does a do-not-attempt-resuscitation order matter.
BMC Anesthesiol 2013;13:43. Crossref
2. Hon KL, Luk MP, Fung WM, et al. Mortality, length of stay,
bloodstream and respiratory viral infections in a pediatric
intensive care unit. J Crit Care 2017;38:57-61. Crossref
3. Goila AK, Pawar M. The diagnosis of brain death. Indian J
Crit Care Med 2009;13:7-11. Crossref
4. Sarbey B. Definitions of death: brain death and what
matters in a person. J Law Biosci 2016;3:743-52. Crossref
5. Kirschen MP, Francoeur C, Murphy M, et al. Epidemiology
of brain death in pediatric intensive care units in the United
States. JAMA Pediatr 2019;173:469-76. Crossref
6. Joffe AR, Shemie SD, Farrell C, Hutchison J, McCarthy-Tamblyn L. Brain death in Canadian PICUs: demographics,
timing, and irreversibility. Pediatr Crit Care Med 2013;14:1-9. Crossref
7. Citerio G, Murphy PG. Brain death: the European
perspective. Semin Neurol 2015;35:139-44. Crossref
8. Daoust A, Racine E. Depictions of “brain death” in the
media: medical and ethical implications. J Med Ethics
2014;40:253-9. Crossref
9. Verheijde JL, Rady MY, Potts M. Neuroscience and brain
death controversies: the elephant in the room. J Relig
Health 2018;57:1745-63. Crossref
10. Marikar D. The diagnosis of death by neurological criteria
in infants less than 2 months old: RCPCH guideline 2015.
Arch Dis Child Educ Pract Ed 2016;101:186. Crossref
11. Greer DM, Varelas PN, Haque S, Wijdicks EF. Variability
of brain death determination guidelines in leading US
neurologic institutions. Neurology 2008;70:284-9. Crossref
12. Chua HC, Kwek TK, Morihara H, Gao D. Brain death: the
Asian perspective. Semin Neurol 2015;35:152-61. Crossref
13. Al-Shammri S, Nelson RF, Madavan R, Subramaniam TA,
Swaminathan TR. Survival of cardiac function after brain
death in patients in Kuwait. Eur Neurol 2003;49:90-3. Crossref
14. Burkle CM, Sharp RR, Wijdicks EF. Why brain death is
considered death and why there should be no confusion.
Neurology 2014;83:1464-9. Crossref
15. Shewmon DA. Chronic “brain death” meta-analysis and
conceptual consequences. Neurology 1998;51:1538-45. Crossref
16. López-Navidad A. Chronic “brain death”: meta-analysis
and conceptual consequences. Neurology 1999;53:1369-70. Crossref
17. Truog RD, Miller FG. Changing the conversation about
brain death. Am J Bioeth 2014;14:9-14. Crossref
18. Shah SK, Kasper K, Miller FG. A narrative review of the
empirical evidence on public attitudes on brain death and
vital organ transplantation: the need for better data to
inform policy. J Med Ethics 2015;41:291-6. Crossref
19. Leung KK, Fung CO, Au CC, Chan DM, Leung GK.
Knowledge and attitudes toward brain stem death among
university undergraduates. Transplant Proc 2009;41:1469-72. Crossref
20. Truog RD. Brain death-too flawed to endure, too ingrained
to abandon. J Law Med Ethics 2007;35:273-81. Crossref
21. Burns JP, Truog RD. Futility: a concept in evolution. Chest
2007;132:1987-93. Crossref