Hong Kong Med J 2020 Apr;26(2):102–10 | Epub 2 Apr 2020
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE
External validation of a simple scoring system to
predict pregnancy viability in women presenting
to an early pregnancy assessment clinic
Osanna YK Wan, FHKAM (Obstetrics and Gynaecology), FHKCOG; Symphorosa SC Chan, MD, FRCOG; Jacqueline PW Chung, FHKAM (Obstetrics and Gynaecology), FHKCOG; Janice WK Kwok, BSc; Terence TH Lao, MD, FRCOG; DS Sahota, BEng, PhD
Department of Obstetrics and Gynaecology, The Chinese University of Hong Kong, Shatin, Hong Kong
Corresponding author: Dr Osanna YK Wan (osannawan@cuhk.edu.hk)
Abstract
Introduction: A scoring system combining clinical
history and simple ultrasound parameters was
developed to predict early pregnancy viability
beyond the first trimester. The scoring system
has not yet been externally validated. This study
aimed to externally validate this scoring system to
predict ongoing pregnancy viability beyond the first
trimester.
Methods: This prospective observational cohort
study enrolled women with singleton intrauterine
pregnancies before 12 weeks of gestation. Women
underwent examination and ultrasound scan to
assess gestational sac size, yolk sac size, and fetal
pulsation status. A pregnancy-specific viability
score was derived in accordance with the Bottomley
score. Pregnancy outcomes at 13 to 16 weeks were
documented. Receiver-operating characteristic
curve analysis was used to assess the discriminatory
performance of the scoring system.
Results: In total, 1508 women were enrolled; 1271
were eligible for analysis. After adjustment for
covariates, miscarriage (13%) was significantly
associated with age ≥35 years (odds ratio [OR]=1.99,
95% confidence interval [CI]: 1.19-3.34), higher
bleeding score (OR=2.34, 95% CI: 1.25-4.38), gestational age (OR=1.17, 95% CI: 1.13-1.22), absence
of yolk sac (OR=4.73, 95% CI: 2.11-10.62), absence
of fetal heart pulsation (OR=3.57, 95% CI: 1.87-6.84), mean yolk sac size (OR=1.25, 95% CI: 1.06-1.47), and fetal size (OR=0.82, 95% CI: 0.77-0.88).
The area under the receiver operating characteristic
curve was 0.91 (95% CI: 0.89-0.93). Viability score
of ≥1 corresponded to a >90% probability of viable
pregnancy.
Conclusions: The scoring system was easy to use.
A score of ≥1 could be used to counsel women who
have a high likelihood of viable pregnancy beyond
the first trimester.
New knowledge added by this study
- External validation of the Bottomley score was achieved and a cut-off viability score was established. Women with a viability score of ≥1 had a >90% probability that their pregnancy would be carried to beyond the first trimester.
- Miscarriage was significantly associated with age ≥35 years, higher bleeding score, gestational age, absence of yolk sac, absence of fetal heart pulsation, mean yolk sac size, and fetal size.
- A pregnancy with a large subchorionic haematoma (ratio of mean subchorionic haematoma diameter to gestational sac diameter >0.5) was almost two-fold more likely to miscarry, compared with other pregnancies.
- This scoring system allows gynaecologists to use simple clinical history and standard ultrasound measurements to predict pregnancy viability beyond the first trimester
- This score could potentially enhance treatment of women who present with early pregnancy complications, including reassurance of viability among those with high scores and psychological preparation for miscarriage among those with low scores.
Introduction
Miscarriage is the most common early pregnancy
complication, which constitutes a large burden
for patients and the overall healthcare system.
Approximately one in four women experiences early pregnancy loss during her lifetime; such losses
have significant negative psychological and social
impacts on affected women.1 2 3 4 Miscarriage has
been ranked the second most common diagnosis
for admissions in the past 10 years in Hong Kong.5 In-patient hospital admissions for miscarriage were
considerably reduced following establishment of out-patient
early pregnancy assessment clinics (EPACs)
in various hospitals. Women visit EPACs to seek
reassurance that their pregnancy remains viable,
which may be difficult because gestational sac size
and embryonic growth are not uniform6; moreover,
estimates of gestational age are misleading in women
with irregular menstrual periods.7 8 A score that
signifies the likelihood of a viable pregnancy may
be helpful for clinicians working in EPACs.9 10 This
score would enable clinicians to target appropriate
early psychological or clinical support, thereby
minimising psychological morbidity, especially for
patients with finite resources.
Probability models to predict pregnancy
viability have been reported; these combine clinical
history, sonographic assessment of gestational
sac and heart pulsation, and biochemical
measurements.3 9 11 12 13 However, some models cannot
be utilised in initial counselling, because they require
calculators or biochemical measurements which
may not yet be available.9 12 13 In a recent systematic
review regarding prediction of miscarriage in
women with viable intrauterine pregnancy, it was
found that many combinations of markers have been
tested with varying diagnostic accuracy; however, no
meta-analysis could be performed on combination
models.14 Furthermore, the meta-analysis did not
involve assessment of the proportions of women with intrauterine pregnancy of uncertain viability,
and no scoring system or cut-off value could be
derived for counselling.
The Bottomley score11 is a scoring system
independent of biochemical measurements,
which utilises clinical and ultrasound parameters,
including maternal age, severity of bleeding, and
ultrasound features (eg, mean sizes of gestational
sac and yolk sac, as well as presence of fetal heart
pulsation). It has been validated in comparison
with more complicated probability-based models
in women with intrauterine pregnancy of uncertain
viability; however, the validation study was limited
by small sample size and the exclusion of one third
of the eligible women due to missing variables and
absence of data regarding pregnancy outcomes.12
The scoring system was also limited by the absence of
data regarding body mass index (BMI) and smoking
status, which might affect the likelihood of viable
pregnancy.11 Furthermore, ethnicity influences
miscarriage risk—black women are reportedly more
likely to miscarry than white women,15 whereas rates
among South and East Asian women are reportedly
similar to those of white women after adjustment
for confounders.16 The objective of the present study
was to assess and validate the Bottomley score for
prediction pregnancy viability until 16 weeks of
gestation in a cohort of Chinese pregnant women
who presented to our hospital with threatened
miscarriage or abdominal pain before 12 weeks of
gestation.
Methods
Study design
This non-interventional prospective observational
study was performed at the Prince of Wales Hospital,
Hong Kong, between July 2013 and June 2015.
An out-patient EPAC is available in this hospital
to receive referrals of first trimester pregnant
women with vaginal bleeding, abdominal pain,
or both, and suspected threatened miscarriage,
threatened miscarriage with uncertain viability,
and/or abdominal pain complicating intrauterine
pregnancy; referrals were made by general
practitioners or accident and emergency medical
officers. All gynaecologists at the EPAC had ≥3
years of experience in ultrasound scans, as well as in
diagnosis and treatment of miscarriage.
Patients and clinical assessment
For this study, Chinese women aged ≥18 years with a
singleton intrauterine pregnancy, referred before 12
weeks of gestation based on last menstrual period,
were invited to participate. Participants provided
demographic data for both standard clinical treatment
and determination of the pregnancy viability score.
Women were excluded if they underwent pregnancy termination, had an ectopic or multiple pregnancy,
had pregnancy at an unknown location, or were
diagnosed with miscarriage at the time of initial
presentation. Women with intrauterine pregnancy
of uncertain viability underwent a second ultrasound
examination after 7 to 14 days to determine fetal
viability, in accordance with published guidelines.17 18 19
Detailed information regarding obstetrics
history and history of the current pregnancy were
obtained, including abdominal pain (graded by
pain score) and vaginal bleeding (assessed using a
pictorial blood loss chart with number of pads used;
no bleeding was regarded as a score of 0, while clots
or flooding was regarded as a score of 4). Information
regarding smoking status (smoker or non-smoker),
alcohol intake, and BMI were collected. Smokers
included women who continued to smoke, as well
as those who had discontinued smoking ≤2 weeks
before presentation to our hospital.20 Alcohol
users included women who consumed >2 units per
day, once or twice per week, in the month before
and during their pregnancy.21 Body mass index
was classified in accordance with international
classification as underweight, normal, overweight,
or obese.22
Ultrasound assessment
All women underwent a structured ultrasound
assessment. All transvaginal ultrasound scans were
performed using a GE Voluson 730 ultrasound
machine (GE Healthcare, Zipf, Austria) to ascertain
the location and viability of the pregnancy. Mean
gestational sac diameter, mean yolk sac diameter,
size of fetal pole, and presence of fetal heart
pulsation were documented. The Royal College of
Obstetricians and Gynaecologists guidelines17 18 and
National Institute for Health and Care Excellence
guidelines19 were used for diagnosis of miscarriage,
intrauterine pregnancy of uncertain viability, viable
pregnancy, ectopic pregnancy, or pregnancy of
unknown location. In women with a history of
vaginal bleeding, a hypoechoic or anechoic crescent-shaped
area on ultrasound images was regarded as a
subchorionic haematoma; its three-dimensional size
was classified as small, medium, or large when its
size ratio (relative to gestational sac size) was <0.2,
0.2-0.5, or >0.5, respectively.
Clinical score and patient treatment
Each pregnancy was assigned a Bottomley score based
on clinical history and ultrasound parameters.11 All
clinicians were blinded to the score and all women
in this study were treated in accordance with our
established standard clinical protocols. Pregnancies
were categorised as viable or miscarriage at the repeat
ultrasound scan conducted between 13 and 16 weeks
of gestation, according to the presence or absence of fetal heart pulsation. Women with miscarriage were
treated in accordance with current guidelines.17 19
Watchful waiting, or medical or surgical evacuation
of the uterus, were offered according to each
patient’s clinical condition. For medical evacuation,
misoprostol 800 μg vaginally was used as first-line
treatment, with follow-up assessment to check for
complete evacuation. Patient treatment was not
affected by participation in the study.
Ethics approval
Ethics approval was obtained from the Joint
Chinese University of Hong Kong–New Territories
East Cluster Clinical Research Ethics Committee
(Ref CREC-2013.348). Written informed consent
was obtained from all participants.
Sample size calculations
Bottomley and colleagues11 reported that the areas
under the receiver operating characteristic (ROC)
curves of their score were 0.90 and 0.72 using a
combination of history and ultrasound parameters
and history alone, respectively. To determine
whether the Bottomley score in our local population
exceeded the discriminatory power of the history-alone
model and achieved discriminatory power
similar to that of the combined model, sample size
analysis, using MedCalc Statistical Software version
18.5 (MedCalc Software bv, Ostend, Belgium),
showed that a minimum sample size of 750 was
required for a type 1 error of 1% and power of 90%,
with the assumption that miscarriage occurred in
one of every 10 pregnancies. The planned sample
size was increased to 1500 to allow for the worst-case
scenario of 50% non-participation rate and 50%
loss to follow-up rate.
Statistical analysis
Women were divided into viable or miscarriage groups
according to pregnancy outcome. Comparisons of
socio-demographic and pregnancy characteristics
between the two outcome groups were performed
using the Chi squared test or Fisher’s exact test,
where appropriate, for categorical variables; the
Mann-Whitney U test with post hoc Bonferroni
correction was used for comparisons of continuous
variables. Adjusted odds ratios (ORs) and 95%
confidence intervals (CIs) of significant predictors
of miscarriage were determined by multivariate
logistic regression analysis. Receiver operating
characteristic curves were constructed to determine
the discriminatory performance of the Bottomley
score, as well as to determine the Bottomley score
which predicted 90% viable pregnancies at the
repeat ultrasound scan. Probit regression, with
Bottomley score as the only independent predictor,
was performed to estimate the probability of an ongoing viable pregnancy beyond the first trimester.
Bottomley scores were truncated to a minimum value
of -12 and a maximum value of 18, prior to Probit
regression and ROC analyses. Patients lost to follow-up
were excluded from the study. All analyses were
performed using SPSS Statistics, version 20.0 (IBM
Corp., Armonk [NY], United States) and MedCalc.
P<0.05 was considered statistically significant.
Results
Patient characteristics and ultrasound
measurements
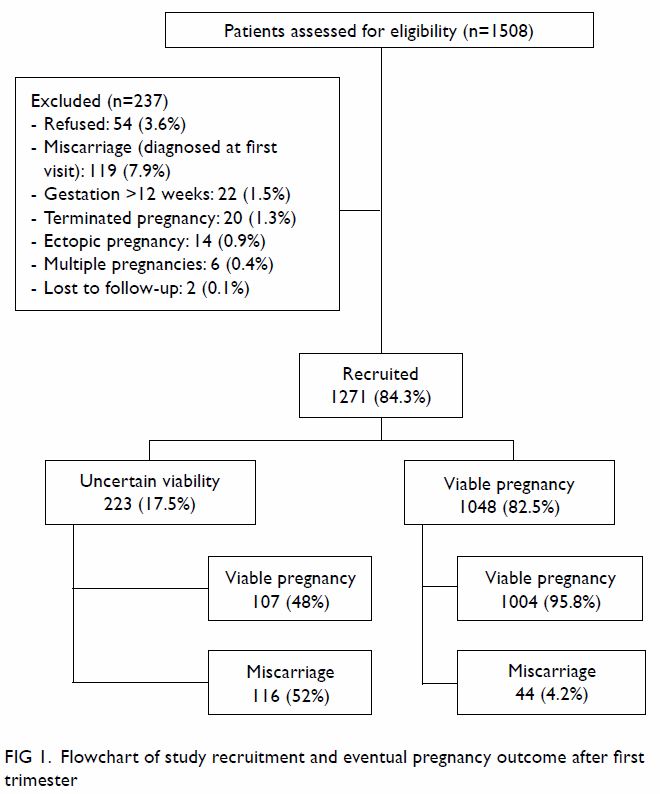
Of the 1508 women invited to participate, 54 (3.6%)
declined and two (0.1%) were lost to follow-up at 13
to 16 weeks of gestation (Fig 1). Table 1 summarises
the socio-demographic characteristics, clinical signs
and symptoms, and ultrasound measurements in the
two outcome groups. The Bottomley score ranged
from -41 to 24; 36 women (2.8%) had a score of
≤-12, and 64 (5.0%) had a score ≥18, while the score
ranged from -12 to +1 in women with a pregnancy of
uncertain viability at first assessment.
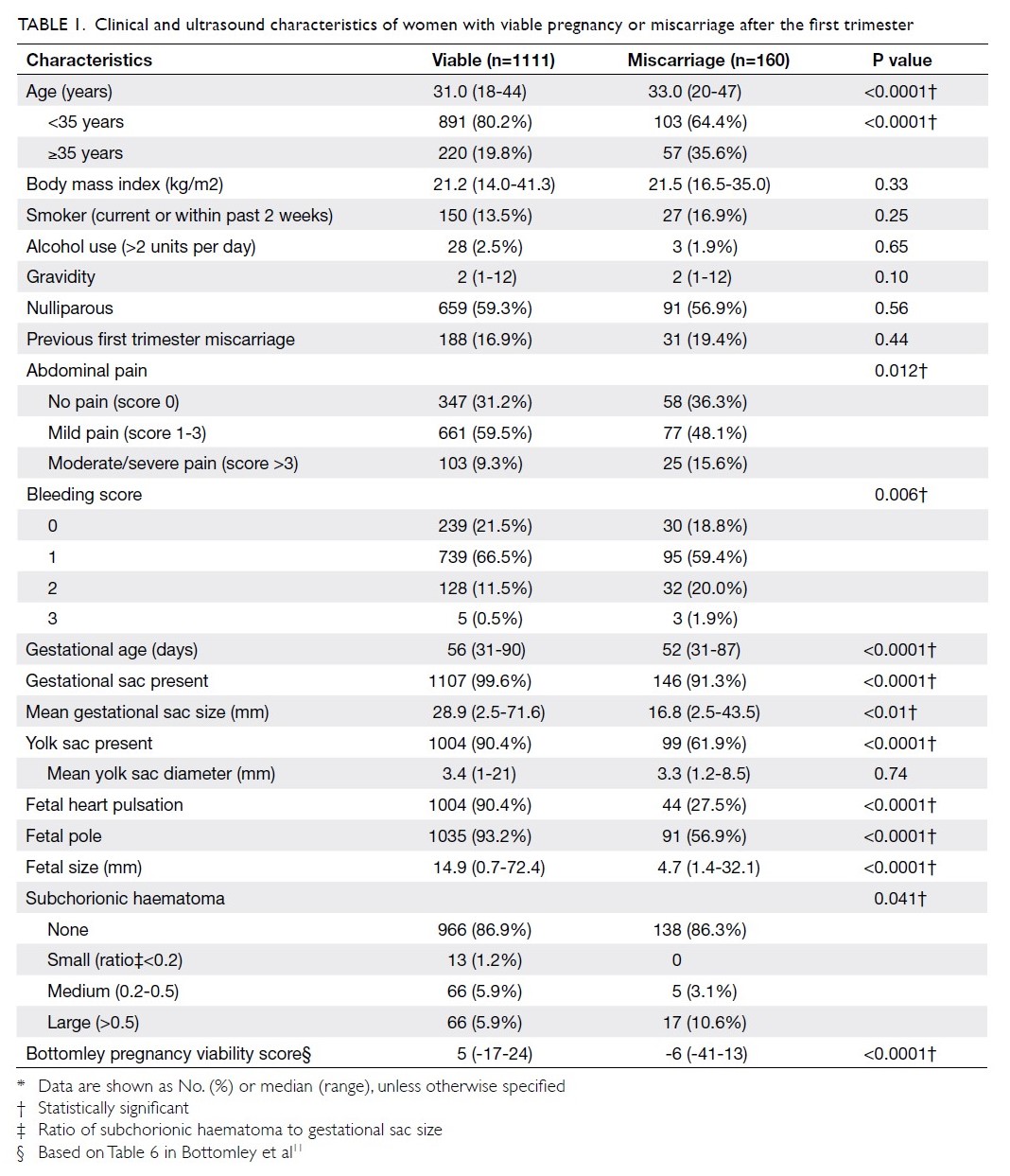
Table 1. Clinical and ultrasound characteristics of women with viable pregnancy or miscarriage after the first trimester
Risk of miscarriage
Unadjusted and adjusted ORs for risk of miscarriage
after adjusting for covariates are summarised in
Table 2. Subchorionic haematoma was noted in 167
pregnancies (13.1%), including 138 (82.6%) with
bleeding. Haematoma size relative to gestational sac
size was significantly associated with miscarriage
(χ2=70.5, P<0.05) [Tables 1 and 2]. A pregnancy
with a large haematoma was nearly two-fold more
likely to miscarry, compared with other pregnancies
(17/160 [10.6%] vs 66/1111 [5.9%]).
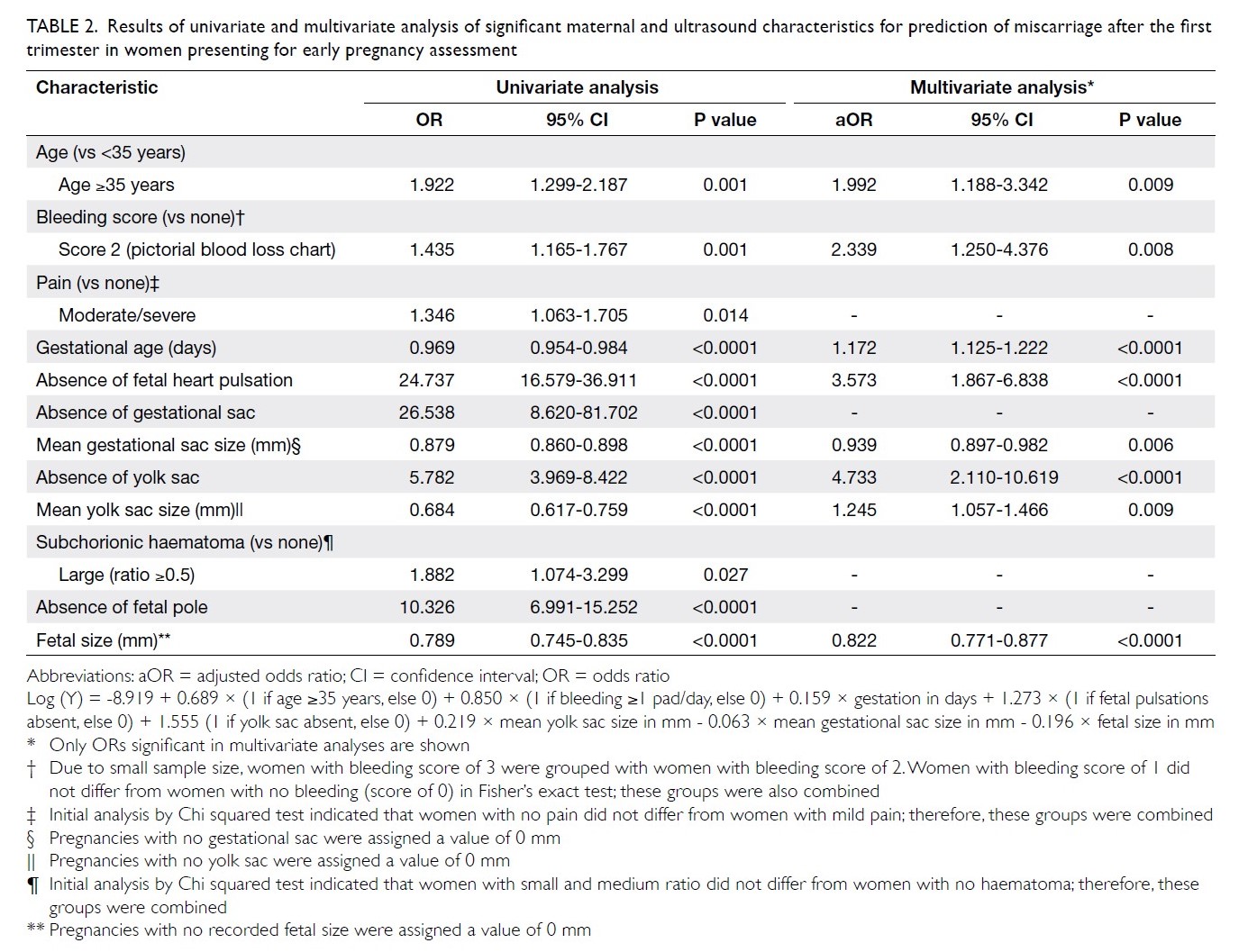
Table 2. Results of univariate and multivariate analysis of significant maternal and ultrasound characteristics for prediction of miscarriage after the first trimester in women presenting for early pregnancy assessment
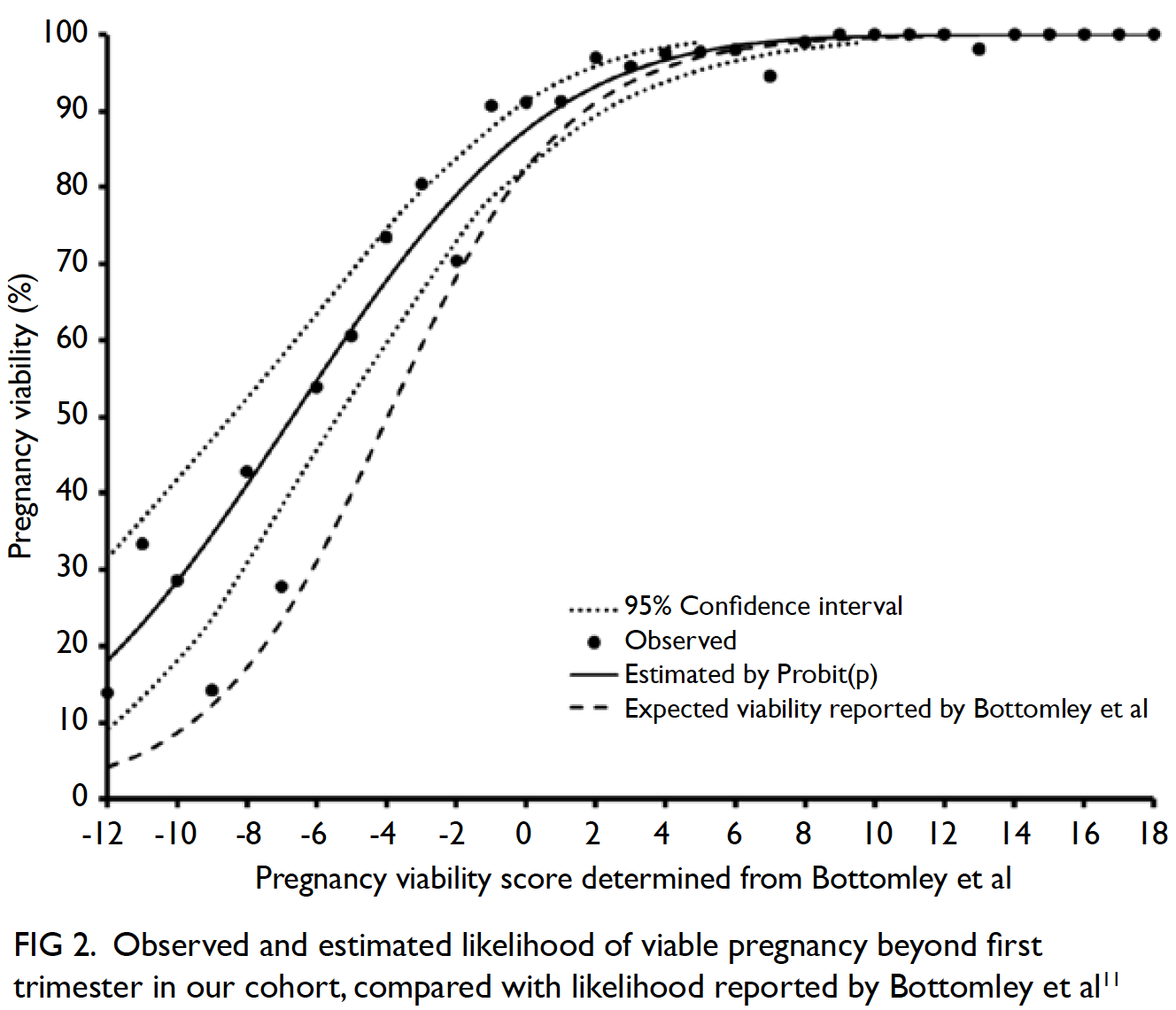
Predictive performance of Bottomley score
The area under the ROC curve of the discriminatory
performance of the Bottomley score in all women
was 0.91 (95% CI: 0.89-0.93, P<0.001). A score of ≥1
had a sensitivity of 91% (95% CI: 85.8-95.1%) and a
false positive rate of 26.7% (95% CI: 24.1-29.4%).
Figure 2 and Table 3 show the observed and
estimated viability of a pregnancy after the first
trimester, compared with the viability estimates
by Bottomley et al11 at each viability score. The
estimated probability of viability for a particular
pregnancy, based on the Bottomley score, was
determined: Probit(p) = 1.15109 + 0.17188 × score.
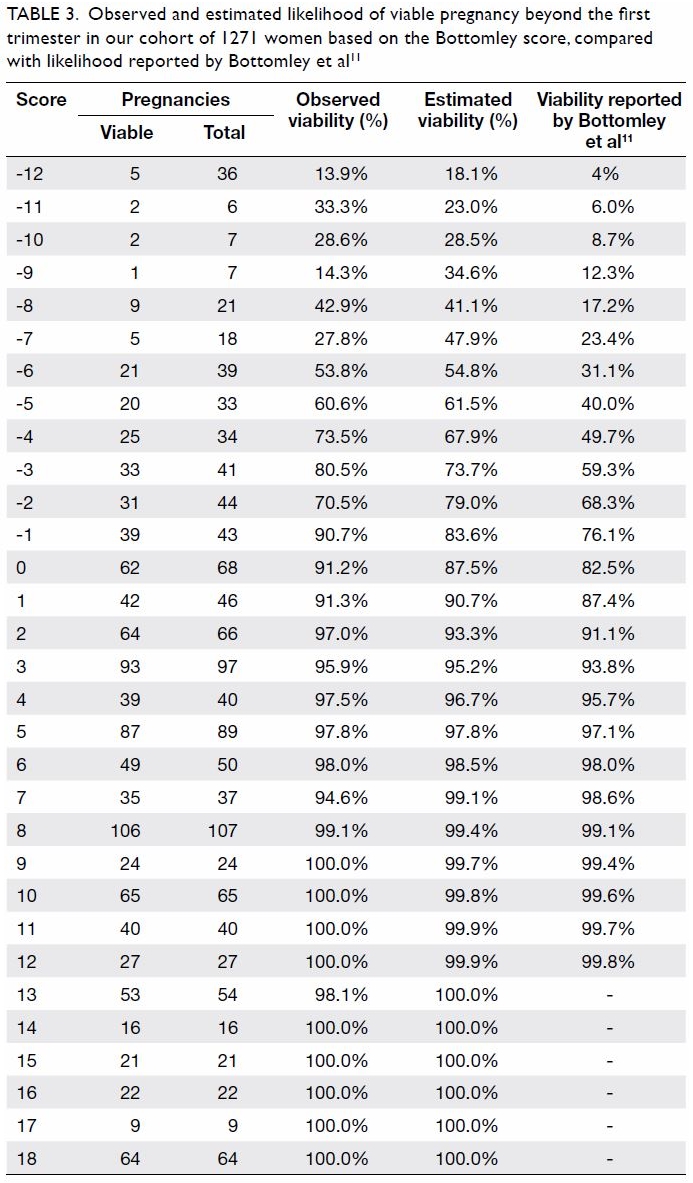
Table 3. Observed and estimated likelihood of viable pregnancy beyond the first trimester in our cohort of 1271 women based on the Bottomley score, compared with likelihood reported by Bottomley et al11
The estimated probability of viability reported
by Bottomley and colleagues11 was within the 95%
CI of the estimated probability determined by our
Probit(p) function if the viability score was ≥0. The
area under the ROC curve of the Bottomley score
in women with a pregnancy of uncertain viability at
initial presentation was only 0.74 (95% CI: 0.67-0.80).
Discussion
To the best of our knowledge, this is the first report
of independent external validation of the scoring
system proposed by Bottomley et al.11 to predict early
second trimester pregnancy viability in women with
intrauterine pregnancy before 12 weeks of gestation.
Moreover, it is the first study in a homogenous
Chinese population. Our findings indicated that the
Bottomley score could be used to predict the likely
outcome of pregnancy, thus potentially alleviating
maternal anxiety; this is particularly useful for
women with symptoms of threatened miscarriage.
The scoring system is simple to use and does
not require a calculator (in contrast to previous
models)8 11; moreover, it relies solely on information
that can be readily obtained by any gynaecologist,
without the need for blood tests.3 12 Women with
a Bottomley score of ≥1 had a >90% probability of
pregnancy viability beyond the first trimester. These
women could be reassured, and further ultrasounds
could be avoided. A low Bottomley score was
associated with increased likelihood of miscarriage,
such that half of the women with a score of -7 or -6
were expected to miscarry; this proportion reached 80% if the score was ≤-12. Proper counselling could
be offered to prepare these women psychologically,
thereby reducing the impact of pregnancy loss.
This scoring system incorporates several
different variables that interact with each other. For
example, a larger but empty gestational sac increases
the likelihood of miscarriage, thus resulting in a
lower (ie, more negative) score; however, this lower
score would be counterbalanced by the presence
of fetal heart pulsation and an appropriately sized yolk sac. In addition, although a negative score was
unexpectedly determined for pregnancies with the
presence of fetal heart pulsation, this negative score
could be counterbalanced by a positive score for a
larger gestational sac size.
Notable strengths in this study include its
use of a priori determination of sample size to
assess discriminatory performance. Moreover, the
participation rate was high and few pregnancies were
lost to follow-up. The resulting large sample size enabled assessment of discriminatory performance
of the scoring system; it also allowed identification
of predictors of miscarriage in our cohort of Chinese
women and provided estimated sensitivities (±5%)
at specific viability scores. Whereas only 10% of
included patients were of Asian ethnicity in the
study by Bottomley et al,11 our study was performed
in a homogenous Chinese population; therefore, our
findings suggest that the score is likely to be valid for
various Asian populations, although further studies
are necessary to validate its use in different Asian
subgroups.
This scoring system was designed for use in
all pregnant women with an intrauterine pregnancy
before 12 weeks of gestation. Our analysis of the
performance of this scoring system in pregnancies
with uncertain viability alone also showed reasonable
performance: pregnancy failure could be predicted in
women with pregnancies of uncertain viability, with
an area under the ROC curve of >0.5. However, this
finding should be interpreted with caution, because
there were only 223 women in this subgroup; our sample size was only sufficient to detect an area
under the ROC curve of 0.65, assuming that the
ratio of miscarriage to viability was 1:1. Of note,
while the scoring system was reliable for estimation
of pregnancy viability until 16 weeks of gestation, the
implication of each score differed, compared with
the previous study.11
Lastly, the miscarriage rate in this study was
13%, approximately 50% lower than the 20% to
30% rates reported by Kong et al1 and Bottomley
et al.11 However, the observed rate of miscarriage
among women with intrauterine pregnancy of
uncertain viability at presentation was consistent
with the rates observed in other studies.11 12 The
relatively low overall miscarriage rate could have
been due to differences in local referral practices,
because some women attending our EPAC were
asymptomatic, whereas women with heavy vaginal
bleeding or severe abdominal pain might have been
admitted directly for treatment; we were unable to
ascertain how many women with early pregnancy
loss were directly admitted without referral to the
EPAC. We excluded women with ectopic pregnancy
or pregnancy of unknown location because these
women had empty uteri. By focusing on women with
intrauterine pregnancy irrespective of viability, we
presumed that our study would be more likely to
generate useful clinical information for counselling
if the model were validated. Notably, excluded
women comprised only 0.9% of all women invited to
participate in the study.
Other potential explanations for the low
miscarriage rate could be differences in lifestyle
factors, such as smoking and alcohol consumption,
as well as incidence of obesity; in contrast to the
findings in published literature,23 24 these factors
were not associated with pregnancy outcome.
Smoking during pregnancy is rare in Chinese
women.25 Obesity is also uncommon; in the present
study only 35 women (2.7%) had a BMI ≥30 kg/m2,
while the median weight of 53.3 kg and median BMI
of approximately 21-21.5 kg/m2 in this study were
similar to the characteristics of women attending
a first trimester Down syndrome screening clinic
and of pregnant women enrolled in another
prospective study (regarding the pelvic floor) in our
centre.26 27 Lastly, the median duration of gestation
at presentation to EPAC was 55 days in our study,
whereas it was 50 days in the study by Bottomley
et al.11 This could have contributed to our lower
miscarriage rate, which decreases with gestational
age.
Consistent with the findings of other studies,
our multivariate analysis indicated that the following
factors were associated with increased likelihood of
miscarriage: increasing age, absence of fetal heart
pulsation, heavier bleeding, and a large subchorionic
haematoma. In addition to miscarriage, subchorionic haematoma increases the risk of placental abruption
and preterm premature rupture of membranes.28
We previously proposed classification of the three
sizes of the subchorionic haematoma, in relation
to gestational sac size.29 We suggested assessment
of the size of subchorionic haematoma relative to
the gestational sac, rather than the mere presence
or absolute size of subchorionic haematoma, in
accordance with the approach used by clinicians in
the United States.30 This parameter was expected
to enhance prediction of miscarriage, but this hypothesis was not supported by multivariate
analysis results; further studies are needed to
more thoroughly investigate the usefulness of this
parameter.
Conclusion
The results of our external validation study
suggested that the scoring system would reliably
predict probable pregnancy viability, despite slight
differences in score implication. Application of this
score could potentially enhance the treatment of
women who initially present with early pregnancy
complications. The cut-off value obtained in this
study may be useful when counselling pregnant
women. Further studies will be performed in our
study centre to determine whether this externally
validated scoring system could be utilised to
reduce psychological morbidity by reassuring the
women likely to maintain a viable pregnancy, while
psychologically preparing other women for expected
miscarriage.
Author contributions
Concept or design: OYK Wan, SSC Chan, JPW Chung.
Acquisition of data: OYK Wan, JWK Kwok
Analysis or interpretation of data: OYK Wan, JWK Kwok, DS Sahota.
Drafting of the manuscript: OYK Wan, DS Sahota, TTH Lao.
Critical revision of the manuscript for important intellectual content: OYK Wan, SSC Chan, JPW Chung, TTH Lao, DS Sahota.
Acquisition of data: OYK Wan, JWK Kwok
Analysis or interpretation of data: OYK Wan, JWK Kwok, DS Sahota.
Drafting of the manuscript: OYK Wan, DS Sahota, TTH Lao.
Critical revision of the manuscript for important intellectual content: OYK Wan, SSC Chan, JPW Chung, TTH Lao, DS Sahota.
All authors had full access to the data, contributed to the
study, approved the final version for publication, and take
responsibility for its accuracy and integrity.
Conflicts of interest
As an editor of the journal, JPW Chung was not involved in the peer review process. The remaining authors have no
conflicts of interest to disclose.
Declaration
The results from this research have been presented, in part, at
the following conferences:
1. Wan O, Chan SS, Kong G. A prospective observational study to validate the reliability of the early pregnancy viability scoring system. Ultrasound Obstet Gynecol 2015;46(Suppl 1):42. (Oral presentation)
2. Kwok J, Wan O, Chan SS. Subchorionic hematoma: its size and association with early pregnancy outcome. Ultrasound Obstet Gynecol 2015;46(Suppl 1):172. (Poster presentation)
3. Wan OY, Chan SS, Kong GW. A prospective observational study to validate the reliability of the early pregnancy viability scoring system. FOCUS in O&G 2015 Congress; 2015. May 30-31; Shatin, Hong Kong. The Chinese University of Hong Kong; 2015. (Oral presentation)
4. Wan OY, Chan SS, Kong GW. External validation of an early pregnancy viability prediction model via a prospective observational study. RCOG World Congress; 2016. Jun 20-22; Birmingham: United Kingdom; 2016. (Poster presentation)
1. Wan O, Chan SS, Kong G. A prospective observational study to validate the reliability of the early pregnancy viability scoring system. Ultrasound Obstet Gynecol 2015;46(Suppl 1):42. (Oral presentation)
2. Kwok J, Wan O, Chan SS. Subchorionic hematoma: its size and association with early pregnancy outcome. Ultrasound Obstet Gynecol 2015;46(Suppl 1):172. (Poster presentation)
3. Wan OY, Chan SS, Kong GW. A prospective observational study to validate the reliability of the early pregnancy viability scoring system. FOCUS in O&G 2015 Congress; 2015. May 30-31; Shatin, Hong Kong. The Chinese University of Hong Kong; 2015. (Oral presentation)
4. Wan OY, Chan SS, Kong GW. External validation of an early pregnancy viability prediction model via a prospective observational study. RCOG World Congress; 2016. Jun 20-22; Birmingham: United Kingdom; 2016. (Poster presentation)
Funding/support
This research was supported by a research grant from the
Health and Medical Research Fund of Food and Health
Bureau, Hong Kong SAR (HMRF Reference: 12131091). The
study sponsor was not involved in the collection, analysis, or
interpretation of data, or in the writing of the manuscript.
Ethics approval
Ethics approval was obtained from the Joint Chinese University of Hong Kong–New Territories East Cluster Clinical Research Ethics Committee (Ref CREC-2013.348). Written informed
consent was obtained from all the participants.
References
1. Kong GW, Lok IH, Yiu AK, Hui AS, Lai BP, Chung TK.
Clinical and psychological impact after surgical, medical
or expectant management of first-trimester miscarriage—a
randomised controlled trial. Aust N Z J Obstet Gynaecol
2013;53:170-7. Crossref
2. Lok IH, Yip AS, Lee DT, Sahota D, Chung TK. A 1-year
longitudinal study of psychological morbidity after
miscarriage. Fertil Steril 2010;93:1966-75. Crossref
3. Elson J, Salim R, Tailor A, Banerjee S, Zosmer N, Jurkovic
D. Prediction of early pregnancy viability in the absence of
an ultrasonically detectable embryo. Ultrasound Obstet
Gynecol 2003;21:57-61. Crossref
4. Volgsten H, Jansson C, Darj E, Stavreus-Evers A. Women’s
experiences of miscarriage related to diagnosis, duration,
and type of treatment. Acta Obstet Gynecol Scand
2018;97:1491-8. Crossref
5. Hong Kong College of Obstetricians and Gynaecologists.
Territory-wide Obstetrics and Gynaecology Audit
Report 2009. Hong Kong College of Obstetricians and
Gynaecologists; 2014.
6. Abdallah Y, Daemen A, Guha S, et al. Gestational sac
and embryonic growth are not useful as criteria to define
miscarriage: a multicenter observational study. Ultrasound
Obstet Gynecol 2011;38:503-9. Crossref
7. Bottomley C, Bourne T. Dating and growth in the
first trimester. Best Pract Res Clin Obstet Gynaecol
2009;23:439-52. Crossref
8. Doubilet PM. Should a first trimester dating scan be
routine for all pregnancies? Semin Perinatol 2013;37:307-9. Crossref
9. Oates J, Casikar I, Campain A, et al. A prediction model
for viability at the end of the first trimester after a single
early pregnancy evaluation. Aust N Z J Obstet Gynaecol
2013;53:51-7. Crossref
10. Stamatopoulos N, Lu C, Casikar I, et al. Prediction of
subsequent miscarriage risk in women who present with a
viable pregnancy at the first early pregnancy scan. Aust N
Z J Obstet Gynaecol 2015;55:464-72. Crossref
11. Bottomley C, Van Belle V, Kirk E, Van Huffel S, Timmerman
D, Bourne T. Accurate prediction of pregnancy viability by
means of a simple scoring system. Hum Reprod 2013;28:68-76. Crossref
12. Guha S, Van Belle V, Bottomley C, et al. External validation
of models and simple scoring systems to predict miscarriage
in intrauterine pregnancies of uncertain viability. Hum
Reprod 2013;28:2905-11. Crossref
13. Ku CW, Allen JC Jr, Malhotra R, et al. How can we better
predict the risk of spontaneous miscarriage among women
experiencing threatened miscarriage? Gynecol Endocrinol
2015;31:647-51. Crossref
14. Pillai RN, Konje JC, Richardson M, Tincello DG, Potdar
N. Prediction of miscarriage in women with viable
intrauterine pregnancy—a systematic review and
diagnostic accuracy meta-analysis. Eur J Obstet Gynecol
Reprod Biol 2018;220:122-31. Crossref
15. Mukherjee S, Velez Edwards DR, Baird DD, Savitz DA,
Hartmann KE. Risk of miscarriage among black women
and white women in a U.S. prospective cohort study. Am J
Epidemiol 2013;177:1271-8. Crossref
16. Khalil A, Rezende J, Akolekar R, Syngelaki A, Nicolaides
KH. Maternal racial origin and adverse pregnancy
outcome: a cohort study. Ultrasound Obstet Gynaecol
2013;41:278-85. Crossref
17. Royal College of Obstetricians and Gynaecologists.
The Management of Early Pregnancy Loss. Green-top
Guideline No 25, 2006. Available from: http://www.jsog.
org/GuideLines/The_management_of_early_pregnancy_
loss.pdf. Accessed 7 Aug 2019.
18. Royal College of Obstetricians and Gynaecologists.
Addendum to GTG No 25 (Oct 2006). Available from:
https://www.rcog.org.uk/globalassets/documents/news/
addendum-to-gtg-no-25.pdf. Accessed 7 Aug 2019.
19. National Institute for Health and Care Excellence.
Ectopic pregnancy and miscarriage: diagnosis and initial
management. Clinical guideline [CG154]. Available from:
https://www.nice.org.uk/Guidance/CG154. Accessed 7
Aug 2019.
20. National Institute for Health and Care Excellence. Smoking:
stopping in pregnancy and after childbirth. Public Health
guideline [PH26]. Available from: https://www.nice.org.
uk/guidance/ph26. Accessed 7 Aug 2019.
21. National Institute for Health and Care Excellence. Antenatal care for uncomplicated pregnancies. Clinical
guideline [CG62]. Available from: https://www.nice.org.
uk/Guidance/CG62. Accessed 7 Aug 2019.
22. WHO Expert Consultation. Appropriate body-mass index
for Asian populations and its implications for policy and
intervention strategies. Lancet 2004;363:157-63. Crossref
23. Pan Y, Zhang S, Wang Q, et al. Investigating the association
between prepregnancy body mass index and adverse
pregnancy outcomes: a large cohort study of 536 098
Chinese pregnant women in rural China. BMJ Open
2016;6:e011227. Crossref
24. Pineles BL, Park E, Samet JM. Systematic review and metaanalysis
of miscarriage and maternal exposure to tobacco
smoke during pregnancy. Am J Epidemiol 2014;179:807-
23. Crossref
25. Kong GW, Tam WH, Sahota DS, Nelson EA. Smoking
pattern during pregnancy in Hong Kong Chinese. Aust N
Z J Obstet Gynaecol 2008;48:280-5. Crossref
26. Sahota DS, Leung WC, Chan WP, To WW, Lau ET,
Leung TY. Prospective assessment of the Hong Kong
Hospital Authority universal Down syndrome screening
programme. Hong Kong Med J 2013;19:101-8.
27. Chan SS, Cheung RY, Yiu AK, et al. Prevalence of levator
ani muscle injury in Chinese women after first delivery.
Ultrasound Obstet Gynecol 2012;39:704-9. Crossref
28. Tuuli MG, Norman SM, Odibo AO, Macones GA, Cahill
AG. Perinatal outcomes in women with subchorionic
hematoma: a systematic review and meta-analysis. Obstet
Gynecol 2011;117:1205-12. Crossref
29. Kwok J, Wan O, Chan SS. P16.02: Subchorionic hematoma:
its size and association with early pregnancy outcome.
Ultrasound Obstet Gynecol 2015;46(Suppl 1):172. Crossref
30. Heller HT, Asch EA, Durfee SM, et al. Subchorionic
hematoma: correlation of grading techniques with
first-trimester pregnancy outcome. J Ultrasound Med
2018;37:1725-32. Crossref