© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
COMMENTARY
Appendiceal endometriosis: a greater mimicker of
appendicitis
David H Jeong, MD; Hyojin Jeon, MD, MPH; Karen
Adkins, MD
Department of Surgery, Trinity School of Medicine,
Ribishi, Saint Vincent
Corresponding author: Mr David H Jeong (kb_1991@hotmail.com)
Endometriosis is defined as the presence of
functioning endometrial glandular cells outside the uterine cavity. It is
a common cause of pelvic pain that is worse during the menstruation cycle.
Endometriosis is extremely difficult to diagnose based on clinical
features, because the location of the ectopic endometrial cells could lead
to diagnosis of other common pathological causes of abdominal pain
specific to that area. Although some female patients remain asymptomatic,
endometriosis is usually associated with dysmenorrhea, chronic pelvic
pain, and infertility and can lead to bowel obstruction or abdominal mass.1
Although endometriosis within the uterine muscle
wall is commonly seen in about 10% of women of menstrual age, ectopy of
endometrial cells into the appendix is rare. The true prevalence of
extragenital endometriosis is unclear, owing to the lack of studies or
cases; the incidence of appendiceal endometriosis has been reported to be
as low as 0.054% and as high as 0.8%.2
Although endometriosis has been reported in almost any part of the human
body, to the best of our knowledge no cases have yet reported
endometriosis in the spleen.3
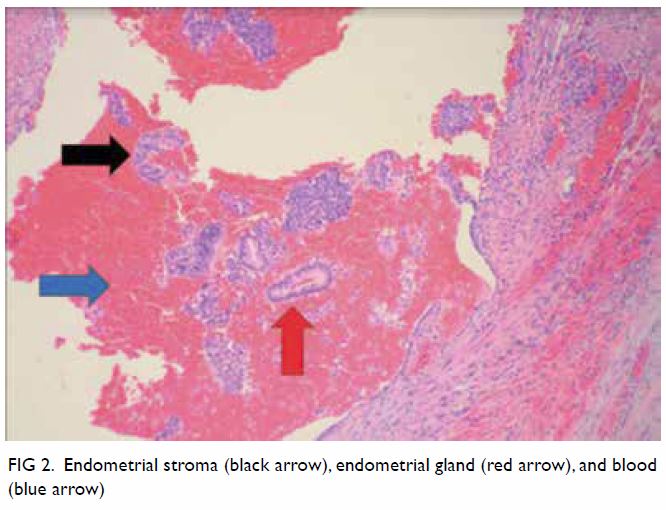
Appendiceal endometriosis is diagnosed
pathologically. The presence of glandular tissue, endometrial stroma, and
haemorrhage are typical findings in patients with endometriosis regardless
of the location.4 There is no
correlation between the location of the endometriotic foci and clinical
symptoms5 and endometriosis is much
likely to mimic primary inflammatory diseases. In the patient described in
this case report, ectopic endometrial cells mimicked inflammation inside
the appendiceal cavity and the patient presented with clinical symptoms
that were consistent with acute appendicitis.
In 2018, we experienced a 34-year-old woman who
presented with right lower quadrant abdominal pain for 1 day. The patient
described the localised pain as crampy and rated the pain severity as “10”
on a scale of 1 to 10. The patient presented with nausea, vomiting,
headache, constipation, menorrhagia, and dizziness. She also reported that
she was actively menstruating and that these symptoms typically occurred
monthly with menstruation, but had been particularly severe in that month.
The patient has two children and reported not using any form of
contraception. The patient’s medical history included inflammatory bowel
disease, migraine, chronic lower back pain, and asthma. The patient had a
Caesarean section delivery in 2000 and left fallopian tube/ovary removal
secondary to ruptured ectopic pregnancy in 2008. The patient denied use of
alcohol, tobacco, or illicit drugs. There was no relevant family history
of gastrointestinal diseases or malignancies and the patient was allergic
to morphine and azithromycin.
Physical examination showed mild distension of the
abdomen and tenderness to palpation on both right and left lower
quadrants. No rebounding tenderness or guarding was noted. Vital signs and
laboratory test results were all within normal limits with the exception
of slightly elevated white blood cell at 11.69 K/mm3. Although
5.32 M/mm3 of red blood cell was observed in the urinalysis,
the results were considered within normal limits since the patient was
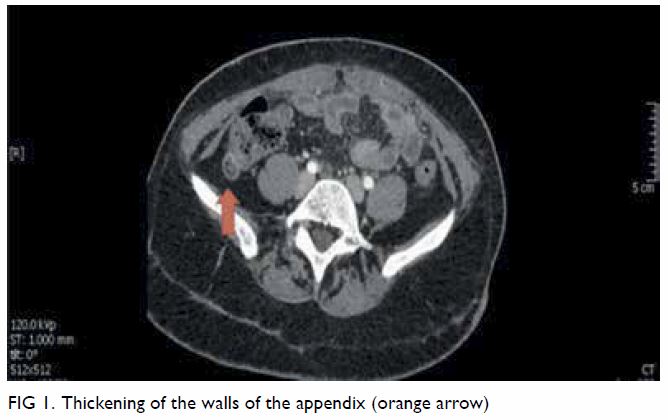
actively menstruating at the time of the test. Computed tomography scan of
the patient’s abdomen and pelvis (Fig 1) showed thick-walled appendix (>7 mm)
consistent with acute appendicitis.
The patient was taken to the operation room for
laparoscopic appendectomy. When the laparoscope was inserted inside the
patient’s abdominal cavity, significant adhesion of the entire abdominal
wall was noted. The appendix was unable to be visualised even after lysis
of adhesion was attempted using electrocautery. A decision was made to
proceed to open appendectomy. Further lysis of adhesions had to be done to
visualise the appendix, which did not show any gross inflammation. The
appendix was excised and sent to pathology lab for further investigation.
The appendix did not show any signs of
inflammation, and the preoperative diagnosis of acute appendicitis was
changed to possible endometriosis or ruptured cyst. However, 3 days after
the appendectomy, pathology results showed infiltration of endometrial
glands, endometrial stroma, and blood into the appendix (Fig
2). On the basis of these findings, appendiceal endometriosis was
finally diagnosed. After the appendectomy, the patient reported
substantial improvement of the right lower quadrant pain.
Appendiceal endometriosis is rare and its
preoperative diagnosis based on clinical features and/or imaging is
extremely difficult. Differential diagnosis in female patients who present
with acute pain in the right lower quadrant, especially those who are of
menstruating age, should include appendiceal endometriosis. Laparoscopy is
useful for the diagnosis since no gross inflammation is observed in the
appendix itself and appendectomy relieves the acute symptoms.
Author contributions
All authors contributed to the concept of study,
acquisition and analysis of data, drafting of the article, and critical
revision for important intellectual content. All authors had full access
to the data, equally contributed to the study, approved the final version
for publication and take responsibility for the accuracy and integrity of
the content.
Conflicts of interest
The authors have no conflicts of interest to
disclose.
Funding/support
This research has received no specific grant from
any funding agency in the public, commercial, or not-for-profit sectors.
Ethics approval
The patient was treated in accordance with the
Declaration of Helsinki. The patient provided informed consent for all
procedures.
References
1. Yantiss RK, Clement PB, Young RH.
Endometriosis of the intestinal tract: a study of 44 cases of a disease
that may cause diverse challenges in clinical and pathological evaluation.
Am J Surg Pathol 2001;25:445-54. Crossref
2. Collins DC. A study of 50,000 specimens
of the human vermiform appendix. Surg Gynecol Obstet 1955;101:437-45.
3. Berker B, Lashay N, Davarpanah R,
Marziali M, Nezhat CH, Nezhat C. Laparoscopic appendectomy in patients
with endometriosis. J Minim Invasive Gynecol 2005;12:206-9. Crossref
4. Apostolidis S, Michalopoulos A,
Papavramidis TS, Papadopoulos VN, Paramythiotis D, Harlaftis N. Inguinal
endometriosis: three cases and literature review. South Med J
2009;102:206-7. Crossref
5. Uncu H, Taner D. Appendiceal
endometriosis: two case reports. Arch Gynecol Obstet 2008;278:273-5. Crossref