Hong Kong Med J 2019 Dec;25(6):453–9 | Epub 4 Dec 2019
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE
Uterine Fibroid Symptom and Health-related Quality of
Life Questionnaire: a Chinese translation and validation study
SY Yeung, FHKAM (Obstetrics and Gynaecology),
FHKCOG; Janice WK Kowk, BSc; SM Law, FHKAM (Obstetrics and Gynaecology), FHKCOG;
Jacqueline PW Chung, FHKAM (Obstetrics and Gynaecology), FHKCOG; Symphorosa SC Chan, FHKAM
(Obstetrics and Gynaecology), FHKCOG
Department of Obstetrics and Gynaecology, Prince of
Wales Hospital, The Chinese University of Hong Kong, Shatin,
Hong Kong
Corresponding author: Dr SY Yeung (carolyeung@cuhk.edu.hk)
Abstract
Introduction: The Uterine
Fibroid Symptom and Health-related Quality of Life (UFS-QOL)
questionnaire is a validated tool in English language to assess
treatment outcomes for women with fibroids. We performed a Chinese
(traditional) translation and cultural adaptation of it and evaluated
its reliability, validity, and responsiveness.
Methods: Overall, 223 Chinese
women aged ≥18 years with uterine fibroids self-administered the
UFS-QOL, Short-Form Health Survey-12, pictorial blood loss assessment
chart (PBAC), and a visual analogue scale (VAS) on fibroid-related
symptom severity. Demographics and haemoglobin levels were recorded;
physical examination and ultrasound for size of fibroids were performed.
Half of the women were followed up 6 months later for responsiveness.
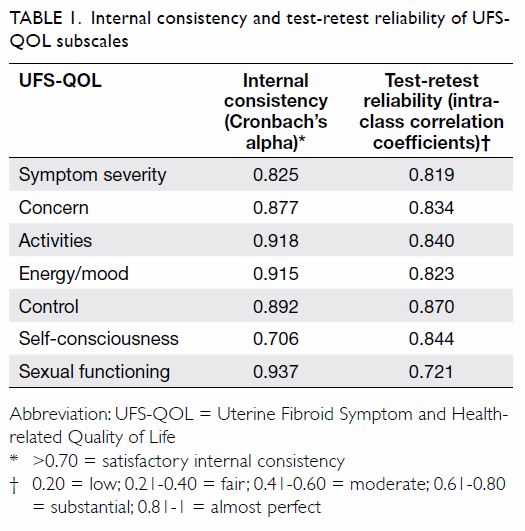
Results: Cronbach’s alpha
coefficients ranged from 0.706 to 0.937, demonstrating high internal
reliability. The intra-class correlation coefficients to measure
test-retest reliability implied excellent stability of symptom scores
(0.819, P<0.001), health-related quality of life scores (0.897,
P<0.001), and all subscales (range 0.721-0.870, P<0.001).
Convergent validity was demonstrated by positive correlations between
the findings of various symptom severity assessment tools (PBAC, VAS on
fibroid-related symptoms severity) and the symptom severity domain of
Chinese UFS-QOL. In addition, there were positive correlations between
health-related quality of life scores of Chinese UFS-QOL and the
corresponding subscales of the Short-Form Health Survey-12.
Responsiveness was shown by reduction of symptom severity scores and
improvement of health-related quality of life scores after treatment.
Conclusions: The Chinese version
of the UFS-QOL is valid, reliable, and responsive to changes after
treatment.
New knowledge added by this study
- The Chinese version of the Uterine Fibroid Symptom and Quality of Life Questionnaire (UFS-QOL) questionnaire is a valid and reliable tool to assess the impact of uterine fibroids on women’s quality of life, and it can be used to evaluate the response after treatment for uterine fibroids.
- The Chinese version of the UFS-QOL questionnaire can be used to evaluate the impact of uterine fibroids on quality of life to guide treatment and evaluate response during daily clinical practice. It is also a useful research tool to assess quality of life improvements after various fibroid treatments.
Introduction
Fibroids are the most common benign uterine tumour
affecting reproductive age women, and the lifetime risk is up to 60% in
women aged over 45 years.1 2 They are associated with menorrhagia,3 4 which results
in anaemia and reduced vitality.5
They also exert mass effects, leading to significantly increased urinary
frequency and stress urinary incontinence compared with the general
population.6 Moreover, women with
fibroids may experience deep dyspareunia.7
All the above have negative effects on quality of life.
Measuring the symptoms and quality of life of women
with fibroids is important, as it is a major indicator for treatment. The
Uterine Fibroid Symptom and Health-related Quality of Life Questionnaire
(UFS-QOL) is an English questionnaire published in 2002 that was specially
designed to assess the whole spectrum of fibroid-related symptoms and its
impact on quality of life.8 It
consists of eight items on symptoms and 29 on health-related quality of
life (HRQL) with six subscales (concern, activities, energy/mood, control,
self-consciousness, and sexual functioning). A raw score ranging from 1 to
5 is assigned to each of the items. To calculate the symptom severity
score and HRQL score, the sum of the raw scores of the related items is
transformed into a final score (range, 0-100) based on a specific formula.
A higher symptom severity score indicates more severe symptoms, while a
higher HRQL score indicates better quality of life. The UFS-QOL has been
validated, and its responsiveness was also assessed.8 9 10 It has been widely adopted in different studies to
assess fibroid treatment outcomes11
12 and translated into multiple
languages.13
The objective of this study was to produce a valid,
reliable, culturally adapted Chinese version of the UFS-QOL. We believe
this would serve as a useful tool to assess the impact of fibroid-related
quality of life and response to treatment and facilitate future research
and clinical use in the Chinese population.
Methods
Translation
We obtained approval to use the UFS-QOL from the
Society of the Interventional Radiology Foundation. A forward-backward
procedure was applied to translate the UFS-QOL into traditional Chinese.
Two independent bilingual researchers were asked to separately produce two
forward translations aiming for conceptual translation. The two
translations were reviewed between the two researchers to produce a
provisional draft of the Chinese UFS-QOL. The provisional Chinese UFS-QOL
was then back-translated to English by two other bilingual researchers who
were blinded to the original questionnaire. The back-translated English
version was further compared to the original questionnaire by two
monolingual experts (English) with no discrepancy noted before we
finalised the Chinese version of the UFS-QOL (online Supplementary Appendix)
Study phase
The study was conducted in the gynaecology clinic
of a university hospital between July 2015 and July 2016. All women aged
≥18 years with fibroids who understood written traditional Chinese were
eligible. Women with known mental incapacity or cognitive or developmental
disability were excluded. The Mini-Mental State Examination was performed
to detect and exclude women with unreported psychiatric morbidity. Written
consent was obtained.
Women were asked to fill out the Chinese UFS-QOL
and Short-Form Health Survey-12 (SF-12) before consultation. The SF-12 is
a 12-item survey that assesses eight domains of quality of life (physical
functioning, role limitation as a result of physical and emotional
problems, bodily pain, general health, vitality, social functioning, and
mental health), and it has a validated Chinese version.14 Lower SF-12 scores are associated with worse HRQL.
The participating women were assessed by
gynaecologists who were blinded to the questionnaire information. Clinical
and socio-demographic data including age, gravidity, parity, co-existing
medical illness, menstrual status, education level, marital status,
literacy, and employment status were obtained. General examinations to
examine the subjects for pallor and measure their blood pressure, pulse,
body weight, and height were performed. Abdominal and/or gynaecological
examinations were performed to assess the uterine size and rule out other
pathology. Transabdominal and/or transvaginal ultrasound were performed to
measure uterine size and the number, location, and size of fibroids.
Complete blood work was performed. Both the women and the attending
gynaecologists were asked to grade the overall severity of symptoms on a
10-cm visual analogue scale (VAS), with higher scores indicating more
severe symptoms.
The women maintained a pictorial blood loss
assessment chart (PBAC) for two menstrual cycles. The PBAC is a validated
self-reporting tool with a score calculated every 4 weeks.15 A score ≥100 represents heavy menstrual bleeding, and
≤75 represents normal menses.
The first 60 women filled out the two
questionnaires again 2 weeks later and returned them by mail to
researchers. In addition, a question on perceived change in clinical
condition over the past 2 weeks was asked.
Women were offered appropriate treatment as
clinically indicated. In general, tranexamic acid 500 mg 4 times daily
and/or mefenamic acid 500 mg 3 times daily were prescribed for menorrhagia
unless contra-indicated. Combined oral contraceptive pills were given if
contraception was required and when there was no contraindication. If
medical treatment failed, treatment including endometrial ablation, a
levonorgestrel-containing contraceptive device, myomectomy or
hysterectomy, or uterine artery embolisation (UAE) were offered.
The first half of the recruited women were followed
up 6 months later. They were asked to perform PBAC, and complete blood
work was performed. During follow-up, the women filled out the above
questionnaires again before the gynaecologist’s assessment. The women were
also asked about improvement after treatment.
Sample size and statistical analysis
A sample size of five or more respondents per item
has been proposed for psychometric analysis.16
17 With the UFS-QOL’s total of 37
items and assuming a 20% discard rate due to incomplete filling of
questionnaires, a sample size of 220 was required to adequately assess the
questionnaire.18
We used SPSS (Windows version 20.0; IBM Corp,
Armonk [NY], United States) for statistical analysis. The psychometric
properties of the UFS-QOL were assessed following the American
Psychological Association’s Standards for Educational and Psychological
Testing.19
Reliability
Reliability was assessed by internal consistency
and test-retest correlation. Internal consistency was assessed by
Cronbach’s alpha coefficients, with >0.7 being considered acceptable.16 17
Test-retest reliability was analysed in women who reported no change to
health status over the 2-week period from the first questionnaire.
Test-retest reliability was assessed by intra-class correlation
coefficient. Values between 0.6 and 0.8 indicate substantial agreement,
and values over 0.8 indicate near-perfect agreement.20
Validity
The convergent validity of the UFS-QOL was
estimated by Pearson’s correlation, with participant-rated symptom
severity VAS score, PBAC score, and physician-rated symptom severity VAS
score as well as the quality of life domains of the SF-12. For
discriminant validity, the women were stratified into mild, moderate, and
severe symptoms according to the women-rated symptom severity VAS scores.
A score of VAS ≤4 was classified as mild, while ≥7 was classified as
severe symptomatology. The UFS-QOL scores were compared among the three
groups.
Responsiveness
Responsiveness was evaluated by comparing pre- and
post-treatment scores using paired samples t tests or Wilcoxon
signed rank tests. The effect size (ie, change in mean score divided by
the standard deviation of the baseline)20
and standardised response mean (ie, change in mean score divided by the
standard deviation of the change) were calculated. A value of 0.2 was
considered as a ‘small’ effect, 0.5 a ‘moderate’ effect, and ≥0.8 a
‘large’ effect.
Results
A total of 223 women were recruited. Their mean age
was 44.8±6.0 years (range, 28-62 years). There were multiple fibroids in
54.5% of the participants, and 51.6% of the women had uterine size ≥12
weeks. Overall, 28.3%, 73.3%, 47.1%, and 29.1% reported cycle
irregularity, menorrhagia, dysmenorrhoea, and pressure symptoms from
fibroids, respectively, while 12.1% were asymptomatic. The median UFS-QOL
score at recruitment was 40.6 (interquartile range [IQR]=25.0-56.3) and
67.2 (IQR=48.3-83.6) for symptom severity and HRQL, respectively.
Reliability
The internal consistency and test-retest
reliability values are shown in Table 1. The Cronbach’s alpha values of all
subscales were >0.7. Fifty-one women (85%) returned the questionnaire 2
weeks after the initial visit. All of them reported no health changes.
Test-retest reliability indicated substantial to perfect agreement.
Validity
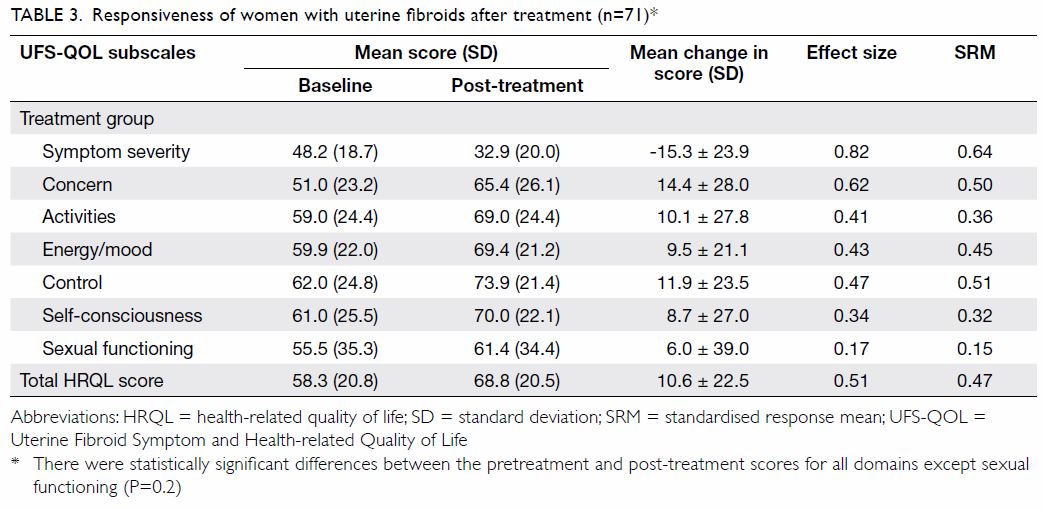
Convergent validity was assessed by the degree of
correlation of the UFS-QOL symptoms severity score on the one hand with
the women-rated and physician-rated VAS scores and PBAC score on the
other. There was a moderate degree of correlation between the UFS-QOL and
these assessment tools (Table 2).
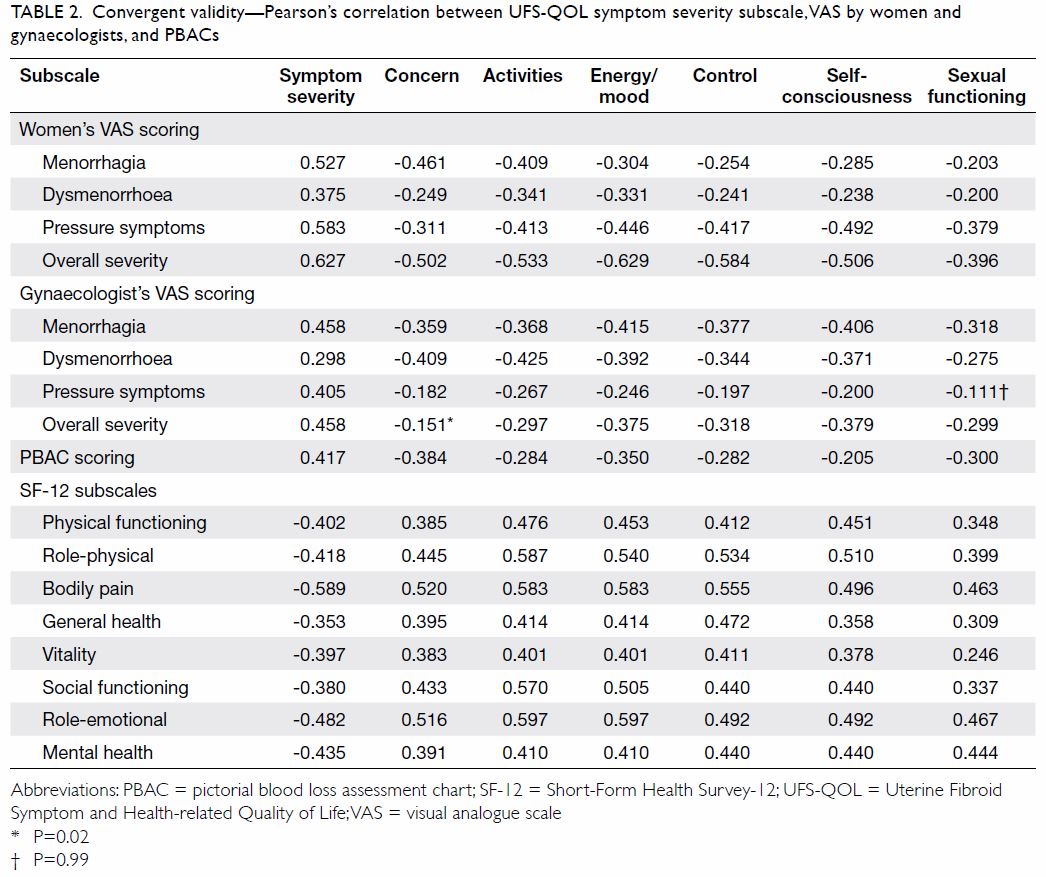
Table 2. Convergent validity—Pearson’s correlation between UFS-QOL symptom severity subscale, VAS by women and gynaecologists, and PBACs
A negative correlation was seen between the UFS-QOL
symptom severity subscale and all domains of the SF-12, and a positive
correlation was observed between the HRQL subscales and SF-12 domains. The
energy/mood and activities subscales had the strongest correlation with
the role-emotional domain of the SF-12 (r=0.597, P<0.001).
The UFS-QOL scores for symptomatic and asymptomatic
women were significantly different across all subscales (median symptom
severity score: 43.8 vs 21.9, P<0.001; median HRQL score: 79.3 vs 63.8,
P<0.001). For women with clinically palpable uterus, the scores on the
control and self-consciousness subscales were lower than those of women
with smaller uterus size (median score of control subscale: 65.0 vs 75.0,
P=0.025; median score of self-consciousness subscale: 67.0 vs 75.0,
P=0.015). Women with significant anaemia (haemoglobin level <80 g/L)
had lower energy and activity subscale scores (median energy score: 50.0
vs 67.9, P=0.014; median activity score: 42.9 vs 66.1, P=0.013) than women
who were not anaemic had.
Women were classified into three groups (mild,
moderate and severe symptoms) according to their symptom severity VAS
score (≤4, 4.1-7, and ≥7). Higher women-rated severity score was
associated with higher UFS-QOL symptom severity score, with significant
differences between different severity groups. Similarly, higher women’s
VAS severity score was associated with lower UFS-QOL HRQL scores. The
differences in UFS-QOL score among the three groups were statistically
significant (P<0.001) for all except the mild versus moderate groups on
the sexual functioning subscale (Fig).
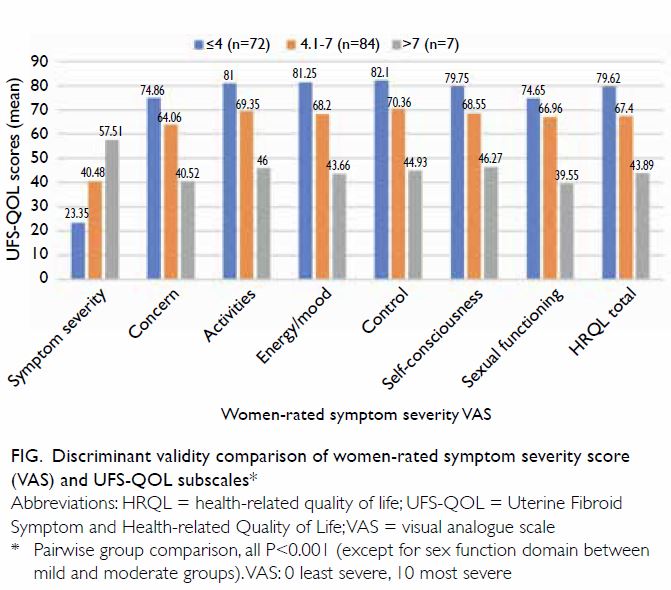
Figure. Discriminant validity comparison of women-rated symptom severity score (VAS) and UFS-QOL subscales
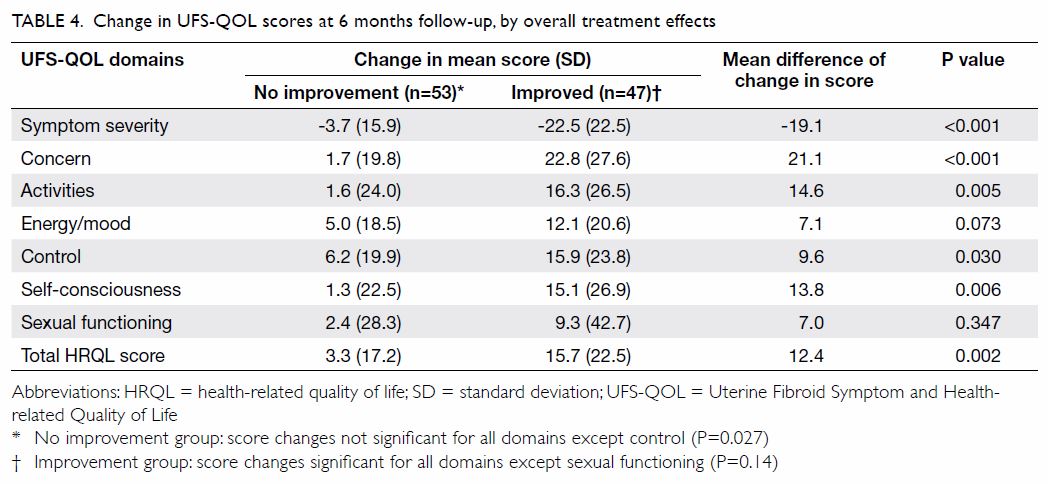
Responsiveness
Among the 100 women being followed up, 50 received
medical treatment, 21 received surgery and UAE (15 hysterectomies, 4
myomectomies, 2 UAE), and 29 did not receive any treatment. There was a
significant reduction in symptom severity score and improvement in HRQL
subscale scores after any treatment, except on the sexual functioning
subscale (Table 3). Despite the results being statistically
insignificant, the sexual functioning subscale still showed a trend
towards quality of life improvement with treatment. For surgically treated
women, the reduction in symptom severity score ranged from 22 to 38 with a
large effect size (range, 0.8-2.6).
For women reporting no improvement (n=53),
reduction in symptom severity scores and improvement in HRQL scores were
modest except for the control subscale (P=0.027). For those participants
who reported improvement (n=47), there was a significant reduction in
symptom severity score and improvement in HRQL scores. The changes were
significant except for the sexual functioning subscale (P=0.14). Women who
reported improvement demonstrated greater improvement in symptom severity
and all HRQL subscales by 7 to 19 points. The differences were significant
for all except the energy/mood and sexual functioning subscales (Table
4).
Discussion
Fibroids are common in women, and the Chinese
population is no exception. Newer treatments such as ulipristal acetate
and high intensity focused ultrasound ablation can shrink fibroids to
improve symptoms.21 22 23 24 Assessment of effects on quality of life is essential
for evaluation of the usefulness of these modalities.
The UFS-QOL is a simple, disease-specific tool that
has been used in various studies to assess treatment outcomes. The Chinese
version of the UFS-QOL needs to be validated before application for
clinical and research purposes because of cultural differences and
language-specific concerns.
Our results showed that the Chinese UFS-QOL is a
reliable tool with high internal consistency (Cronbach’s alpha >0.7 for
all subscales) and almost perfect agreement between test and retest
results (intra-class correlation coefficient >0.8 for all except the
sexual functioning subscale). These results are comparable with the
original and other translated version of the UFS-QOL.8 13
The validity of the Chinese UFS-QOL was supported
by moderate positive correlations between the women-rated VAS score,
physician-rated VAS score, PBAC score, and UFS-QOL symptom severity score
(with correlation coefficients ranging 0.3-0.6). There was also a moderate
positive correlation between the SF-12 and UFS-QOL HRQL subscale scores.
The energy/mood domain of the UFS-QOL had the strongest correlation with
the SF-12 role-emotion domain (r=0.597). Women with larger uterus
size scored lower in the control and self-consciousness domains, and those
with significant anaemia also had lower energy and activity scores. These
results reflected the ability of the Chinese UFS-QOL to assess the
underlying constructs.
The Chinese UFS-QOL also demonstrated
responsiveness towards change in women who received treatment. The mean
change in subscale scores ranged from 6 to 15 points at 6 months
post-treatment. The changes were most pronounced for women who received
surgery (myomectomy or hysterectomy), who had a mean score increase from
22 to 39 and an effect size of ≥0.8 for all subscales. Similar findings
were also reported in a previous study.23
In addition, larger score changes was observed in women who received
surgery compared with medical treatment, an effect that has also been
shown in other studies.24 The
Chinese UFS-QOL was able to discriminate between women who reported that
their treatment was effective compared with those who did not. Although
there were mean increases of 7 points in both the energy/mood and sexual
functioning subscales, they did not reach statistical significance. This
might be explained by the fact that mood and sexual satisfaction could be
affected by multiple factors other than fibroid symptoms alone.
Improvement in fibroid-related symptoms alone might not result in dramatic
changes in these aspects of quality of life.
Strengths and limitations
Our study sample included a wide range of
disease severities and a broad symptom spectrum, which allows generalisation of the
findings to the community of women with fibroids. Another strength is that
the responsiveness of the UFS-QOL was evaluated, which allows its use to
assess treatment effects. However, the study has a few limitations. The
minimal important difference, ie, the smallest clinically significant
change in score large enough to implicate treatment, was not assessed. In
addition, the majority of women who returned for follow-up received either
medical treatment or hysterectomy, whereas few underwent myomectomy
or UAE. Further studies may be required to address these issues. Finally,
there are two forms of written Chinese characters (traditional and
simplified). Because the Chinese UFS-QOL is a self-administered
questionnaire written in traditional Chinese, application to women who can
read only simplified Chinese characters may be limited.
Conclusion
Our study showed that the Chinese version of
UFS-QOL is comparable to the original and other translated version of this
questionnaire in terms of reliability, validity,8
9 13
and responsiveness.10 In
conclusion, the Chinese version of the UFS-QOL is a reliable, valid tool
for the assessment of symptom severity and HRQL. It can be used to
evaluate efficacy and treatment effects on fibroids in women in the
future.
Author contributions
All authors had full access to the data,
contributed to the study, approved the final version for publication, and
take responsibility for its accuracy and integrity.
Concept or design: SY Yeung, SM Law, SSC Chan.
Acquisition of data: SY Yeung, SM Law, JWK Kwok.
Analysis or interpretation of data: SY Yeung, JWK Kwok.
Drafting of the article: SY Yeung.
Critical revision for important intellectual content: SM Law, SSC Chan, JPW Chung.
Acquisition of data: SY Yeung, SM Law, JWK Kwok.
Analysis or interpretation of data: SY Yeung, JWK Kwok.
Drafting of the article: SY Yeung.
Critical revision for important intellectual content: SM Law, SSC Chan, JPW Chung.
Acknowledgement
The authors thank Dr Linda WY Fung for performing
the forward translation, Dr Alyssa SW Wong for the backward translation,
Professor Sonia Grover and Dr Sotirios Saravelos for evaluating the final
English version against the original questionnaire.
Conflicts of interest
As an editor of the journal, JPW Chung was not
involved in the peer review process of the article. Other authors have
disclosed no conflict of interest.
Declaration
The preliminary results of part of this study
(reliability and validity) have been presented during an oral presentation
session at the 25th Asian & Oceanic Congress of Obstetrics &
Gynaecology in Hong Kong, June 2017.
Funding/support
This research received no specific grant from any
funding agency in the public, commercial, or not-for-profit sectors.
Ethics approval
Ethics approval was obtained in April 2015 from the
Joint Chinese University of Hong Kong–New Territories East Cluster
Clinical Research Ethics Committee (CREC Ref 2015.085).
References
1. Stewart EA, Cookson CL, Gandolfo RA,
Schulze-Rath R. Epidemiology of uterine fibroids: a systematic review.
BJOG 2017;124:1501-12. Crossref
2. Okolo S. Incidence, aetiology and
epidemiology of uterine fibroids. Best Pract Res Clin Obstet Gynaecol
2008;22:571- 88. Crossref
3. Vercellini P, Vendola N, Ragni G,
Trespidi L, Oldani S, Crosignani PG. Abnormal uterine bleeding associated
with iron-deficiency anemia. Etiology and role of hysteroscopy. J Reprod
Med 1993;38:502-4.
4. Emanuel MH, Verdel MJ, Stas H, Wamsteker
K, Lammes FB. An audit of true prevalence of intra-uterine pathology: the
hysteroscopical findings controlled for patient selection in 1202 patients
with abnormal uterine bleeding. Gynaecological Endoscopy 1995;4:237-42.
5. Ando K, Morita S, Higashi T, et al.
Health-related quality of life among Japanese women with iron-deficiency
anemia. Qual Life Res 2006;15:1559-63. Crossref
6. Dancz CE, Kadam P, Li C, Nagata K, Özel
B. The relationship between uterine leiomyomata and pelvic floor symptoms.
Int Urogynecol J 2014;25:241-8. Crossref
7. Moshesh M, Olshan AF, Saldana T, Baird
D. Examining the relationship between uterine fibroids and dyspareunia
among premenopausal women in the United States. J Sex Med 2014;11:800-8. Crossref
8. Spies JB, Coyne K, Guaou Guaou N, Boyle
D, Skyrnarz-Murphy K, Gonzalves SM. The UFS-QOL, a new disease-specific
symptom and health-related quality of life questionnaire for leiomyomata.
Obstet Gynecol 2002;99:290-300. Crossref
9. Coyne KS, Margolis MK, Bradley LD, Guido
R, Maxwell GL, Spies JB. Further validation of the uterine fibroid symptom
and quality-of-life questionnaire. Value Health 2012;15:135-42. Crossref
10. Harding G, Coyne KS, Thompson CL,
Spies JB. The responsiveness of the uterine fibroid symptom and
health-related quality of life questionnaire (UFS-QOL). Health Qual Life
Outcomes 2008;6:99. Crossref
11. Smith WJ, Upton E, Shuster EJ, Klein
AJ, Schwartz ML. Patient satisfaction and disease specific quality of life
after uterine artery embolization. Am J Obstet Gynecol 2004;190:1697-703.
Crossref
12. Olive DL. Sustained relief of
leiomyoma symptoms by using focused ultrasound surgery. Obstet Gynecol
2008;111:775. Crossref
13. Oliveira Brito LG, Malzone-Lott DA,
Sandoval Fagundes MF, et al. Translation and validation of the Uterine
Fibroid Symptom and Quality of Life (UFS-QOL) questionnaire for the
Brazilian Portuguese language. Sao Paulo Med J 2017;135:107-15. Crossref
14. Lam CL, Tse EY, Gandek B. Is the
standard SF-12 health survey valid and equivalent for a Chinese
population? Qual Life Res 2005;14:539-47. Crossref
15. Higham JM, O’Brien PM, Shaw RW.
Assessment of menstrual blood loss using a pictorial chart. Br J Obstet
Gynaecol 1990;97:734-9. Crossref
16. Bryant FB, Yarnold PR. Principal
components analysis and exploratory and confirmatory factor analysis. In:
Grimm LG, Yarnold PR, editors. Reading and Understanding Multivariate
Statistics. American Psychological Association, Washington DC; 1995:
99-136.
17. Gorsuch RL. Factor Analysis. 2nd ed.
Hillsdale, NJ: Lawrence Erlbaum Associates; 1983.
18. Machin D, Campbell MJ, Tan SB, Tan SH.
Sample Size Tables for Clinical Studies, 3rd ed. Chichester, UK:
Wiley-Blackwell; 2009. Crossref
19. American Educational Research
Association, American Psychological Association, National Council on
Measurement in Education; Joint Committee on Standards for Educational and
Psychological Testing. Standards for educational and psychological
testing. Washington, DC: American Educational Research Association; 1999.
20. Cohen J. Statistical power analysis
for the behavioral sciences. Hillsdale, NJ: Lawrence Erlbaum Associates;
1988.
21. Donnez J, Hudecek R, Donnez O, et al.
Efficacy and safety of repeated use of ulipristal acetate in uterine
fibroids. Fertil Steril 2015;103:519-27.e3. Crossref
22. Donnez J, Donnez O, Matule D, et al.
Long-term medical management of uterine fibroids with ulipristal acetate.
Fertil Steril 2016;105:165-73.e4. Crossref
23. Froeling V, Meckelburg K, Schreiter
NF, et al. Outcome of uterine artery embolization versus MR-guided
highintensity focused ultrasound treatment for uterine fibroids: long-term
results. Eur J Radiol 2013;82:2265-9. Crossref
24. Chan SS, Cheung RY, Lai BP, Lee LL,
Choy KW, Chung TK. Responsiveness of the Pelvic Floor Distress Inventory
and Pelvic Floor Impact Questionnaire in women undergoing treatment for
pelvic floor disorders. Int Urogynecol J 2013;24:213-21. Crossref