© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
COMMENTARY
Colonic actinomycosis: a pseudo-tumour that mimics
colonic neoplasm
KW Hui, MB, ChB; Bryant SY Chan, MB, BS, FRCS;
Kenny KY Yuen, MB, BS, FRCS
Department of Surgery, Tseung Kwan O Hospital,
Tseung Kwan O, Hong Kong
Corresponding author: Dr KW Hui (karen.hui@icloud.com)
Introduction
Actinomyces is a class of Gram-positive,
non-acid-fast, anaerobic-to-microaerophilic bacteria commonly
found in the oral cavity. It is known for its causative role in oral
infections after dental procedures. Abdominopelvic involvement is
uncommon, with few reported cases. Risk factors of intra-abdominal
actinomycosis include use of intrauterine device, abdominal or pelvic
procedures, and various causes of intestinal necrosis.1 Current understanding on intra-abdominal actinomycosis
has highlighted its inclination to mimic neoplasm. Reported cases on organ
dissemination and progression to fistulae formation further confound this
diagnostic challenge in clinical practice. Although perforation of
neoplasm remains the primary concern in septic manifestations of an
abdominal mass lesion, infective differentials such as actinomycosis
should be considered. Because the presentation of acute abdomen
necessitates timely treatment, early operative treatment is often favoured
by clinicians, particularly when complications such as sepsis and
intestinal obstruction arise. This leaves limited scope for
investigations. As a result, the diagnosis of intra-abdominal
actinomycosis is often established from pathological assessment after
cure.
Exemplar local case
A 35-year-old woman with good past health presented
to Tseung Kwan O Hospital, Hong Kong, in December 2017, with 1-month
history of right lower abdominal discomfort and low-grade fever. Abdominal
examination identified an 8-cm tender right lower quadrant mass with local
guarding and rebound tenderness. Blood tests showed neutrophil predominant
leukocytosis (17.2 × 109/L). Urgent contrast enhanced computed
tomography scan of the pelvis revealed an ill-defined heterogeneously
enhancing mass at right lower abdomen with matted manifestations in its
vicinity, involving an oedematous terminal ileal segment and
gynaecological organs (Fig 1). The patient underwent diagnostic laparoscopy
with revelation of an 8-cm locally invasive firm mass arising from the
caecum. Dense adhesions to the colonic mesentery and terminal ileum were
dissected free. The right infundibulopelvic ligament and right base of
ovary appeared to be invaded by the colonic pseudo-tumour. The procedure
proceeded to an en bloc resection including formal right hemicolectomy and
right salpingo-oophorectomy. The patient had an uneventful postoperative
recovery course. Pathological examination of the specimen (Fig
2) unveiled histological diagnosis of disseminated actinomycosis
with abscess, fibrosis, and inflammation extending into adjacent
mesenteric tissue, mesoappendix, mesosalpinx, and adhering fibrofatty
tissue.
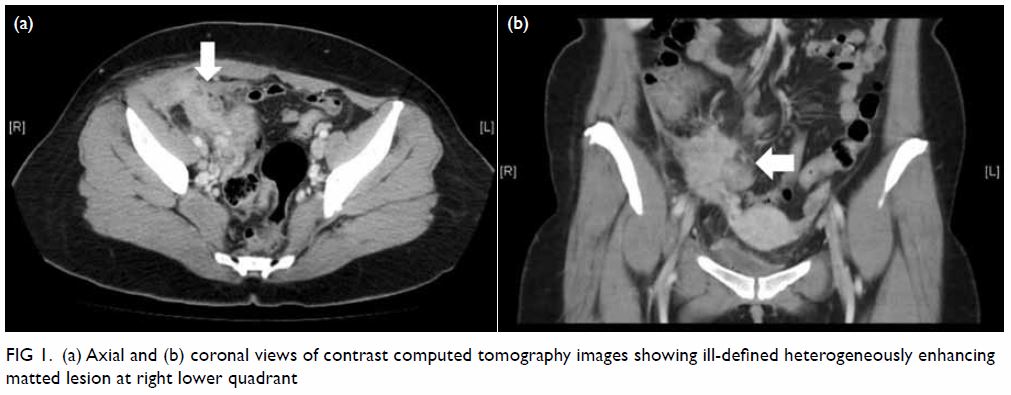
Figure 1. (a) Axial and (b) coronal views of contrast computed tomography images showing ill-defined heterogeneously enhancing matted lesion at right lower quadrant
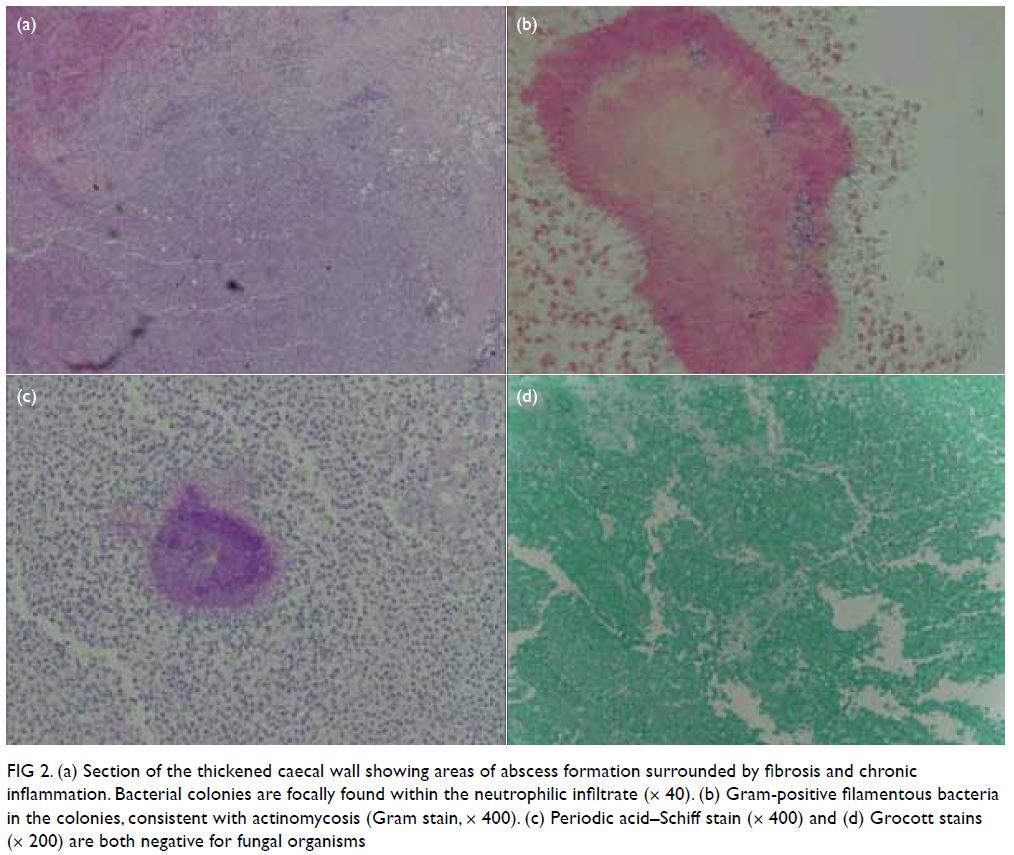
Figure 2. (a) Section of the thickened caecal wall showing areas of abscess formation surrounded by fibrosis and chronic inflammation. Bacterial colonies are focally found within the neutrophilic infiltrate (× 40). (b) Gram-positive filamentous bacteria in the colonies, consistent with actinomycosis (Gram stain, × 400). (c) Periodic acid–Schiff stain (× 400) and (d) Grocott stains (× 200) are both negative for fungal organisms
How to investigate actinomycosis
The current role of imaging in the diagnosis of
intra-abdominal or pelvic actinomycosis is poorly defined. Limited studies
have suggested some computed tomographic features of actinomycosis
describing its infiltrative nature and tendency to invade across tissue
plane and boundaries. Dense inhomogeneous contrast enhancement in walls or
solid component of masses and minimal lymphadenopathy may also be
characteristic.2 However, the
features are often insufficient to help distinguish the condition from
most other differentials. Kim et al3
investigated the efficacy of combining colonoscopy and computed
tomography. In future, combined investigations are expected to gain
popularity, to take advantage of complementary imaging modalities. Degree
of stenosis and mucosal abnormalities are other areas being further
evaluated for imaging studies. Cytological investigations are effective
but limited to variants of actinomycosis such as multi-cystic subtypes.
Image-guided fine needle aspiration may identify actinomycotic granules on
microscopy and facilitate bacterial culture.4
Currently, most clinicians remain reluctant to consider cytological or
tissue samples to avoid the possibility of tumour seeding before a certain
diagnosis has been made.5
How to treat actinomycosis
Owing to the scarcity of reported cases of
actinomycosis, a standardised management protocol is lacking to date.
Evans et al5 advocate antibiotic therapy to obliterate the disease, while
proceeding to extensive resection for the purpose of debulking. High-dose
penicillin is an established first-line regimen in the treatment of
actinomycosis. Doxycycline and clindamycin are alternatives, especially in
patients with penicillin allergy. Prolonged course of antibiotics
postoperatively up to 6 to 12 months until sign of disease clearance is
advocated by some. In view of the tendency of actinomycosis to spread
across tissue planes and disseminate to other organs, surgical resection
may be extensive. Preoperative counselling on possible extent of surgery
is crucial in all cases where actinomycosis is considered.
Prospects
Intra-abdominal actinomycosis is uncommon
worldwide. Imaging and cytological investigations are shown to be useful
but their roles in establishing definitive diagnosis are yet to be
defined. Preliminary studies on combined imaging have demonstrated
promising results. However, a lack of consensus remains over antibiotic
therapy alone versus antibiotic therapy with additional debulking surgery.
Prognosis of the disease entity remains unclear. An evidence-based
management protocol will help standardise care of this rare disease entity
as we gain more understanding from additional cases over time.
Author contributions
All authors had full access to the data,
contributed to the study, approved the final version for publication, and
take responsibility for its accuracy and integrity.
Concept or design of the study: KW Hui, BSY Chan.
Acquisition of data: KW Hui, BSY Chan.
Analysis or interpretation of data: KW Hui, BSY Chan.
Drafting of the article: KW Hui.
Critical revision for important intellectual content: All authors.
Acquisition of data: KW Hui, BSY Chan.
Analysis or interpretation of data: KW Hui, BSY Chan.
Drafting of the article: KW Hui.
Critical revision for important intellectual content: All authors.
Conflicts of interest
The authors have no conflicts of interest to
disclose.
Funding/support
This research received no specific grant from any
funding agency in the public, commercial, or not-for-profit sectors.
Ethics approval
This study was conducted in accordance with the
principles outlined in the Declaration of Helsinki. Informed consent has
been obtained from patient for the treatment.
References
1. Filippou D, Psimitis I, Zizi D, Rizos S.
A rare case of ascending colon actinomycosis mimicking cancer. BMC
Gastroenterol 2005;5:1. Crossref
2. Ha HK, Lee HJ, Kim H, et al. Abdominal
actinomycosis: CT findings in 10 patients. AJR Am J Roentgenol
1993;161:791-4. Crossref
3. Kim JC, Ahn BY, Kim HC, et al.
Efficiency of combined colonoscopy and computed tomography for diagnosis
of colonic actinomycosis: a retrospective evaluation of eight consecutive
patients. Int J Colorectal Dis 2000;15:236-42. Crossref
4. Cameron AE, Menon GG, Wyatt AP.
Abdominal actinomycosis mimicking carcinomatosis. J R Soc Med
1988;81:231-2. Crossref
5. Evans J, Chan C, Gluch L, Fielding I,
Eckstein R. Inflammatory pseudotumour secondary to actinomyces infection.
Aust N Z J Surg 1999;69:467-9. Crossref

