Hong
Kong Med J 2019 Aug;25(4):330.e1-2
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
PICTORIAL MEDICINE
Cardiac magnetic resonance imaging in the diagnosis of
biventricular non-compaction in a young but failing heart
Victor SH Chan, MB, BS, FRCR1; Carmen
WS Chan, MB, BS, FRCP (Lond)2; Stephen CW Cheung, MRCP, FHKAM
(Radiology)1
1 Department of Radiology, Queen Mary
Hospital, Pokfulam, Hong Kong
2 Department of Medicine, Queen Mary
Hospital, Pokfulam, Hong Kong
Corresponding author: Dr Victor SH Chan (victorchansh@gmail.com)
A 15-year-old Chinese girl with a history of
scoliosis presented to Queen Mary Hospital, Hong Kong in April 2016 with
an incidental finding of an ejection systolic murmur at the left lower
sternal border. No history of chest pain, syncope, reduced effort
tolerance, or significant family history of congenital cardiac disease was
present. Echocardiography revealed heavy trabeculations over the left
ventricular (LV) apical region. Colour Doppler revealed abnormal
in-and-out flow at the deep crypts. Overall features were suspicious of LV
non-compaction (NC). The patient subsequently underwent cardiac magnetic
resonance imaging for further assessment, using a 1.5-T magnetic resonance
imaging scanner (Magnetom Aera; Siemens Healthcare, Forchheim, Germany).
Cardiac magnetic resonance confirmed the diagnosis of biventricular NC
with diffuse involvement (Fig 1). The ratio of non-compacted to compacted
diastolic myocardium was 2.95 (>2.3). The LV ejection fraction (EF) was
32.6%, and the right ventricular (RV) EF was 32.5%. Moderate global
hypokinesia of both ventricles was observed. Mild mitral regurgitation was
present. No significant left to right cardiac shunt or late gadolinium
enhancement was seen at the LV wall to suggest presence of scar or
fibrosis (Fig 2). No abnormal thinning of the wall,
focal/regional RV wall motion abnormality, or aneurysmal change was noted.
No thrombus was present within the cardiac chambers. A normal
configuration of a left-sided aortic arch was observed with absence of
coarctation. Subsequent genetic testing for pathogenic mutations for NC
was negative in this patient.
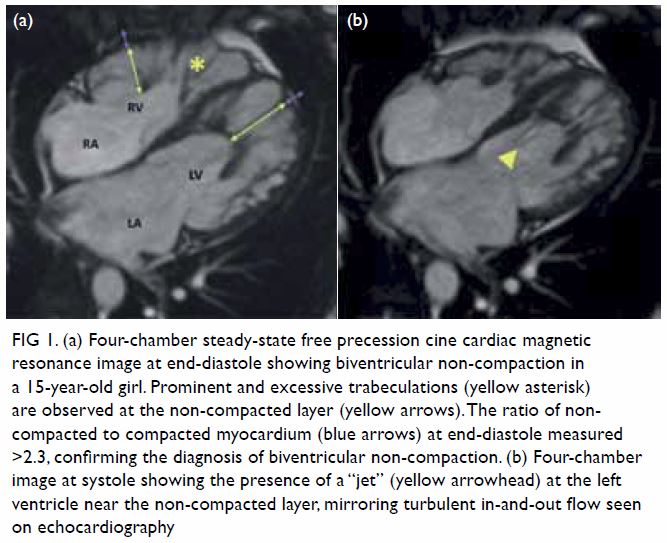
Figure 1. (a) Four-chamber steady-state free precession cine cardiac magnetic resonance image at end-diastole showing biventricular non-compaction in a 15-year-old girl. Prominent and excessive trabeculations (yellow asterisk) are observed at the non-compacted layer (yellow arrows). The ratio of noncompacted to compacted myocardium (blue arrows) at end-diastole measured >2.3, confirming the diagnosis of biventricular non-compaction. (b) Four-chamber image at systole showing the presence of a “jet” (yellow arrowhead) at the left ventricle near the non-compacted layer, mirroring turbulent in-and-out flow seen on echocardiography
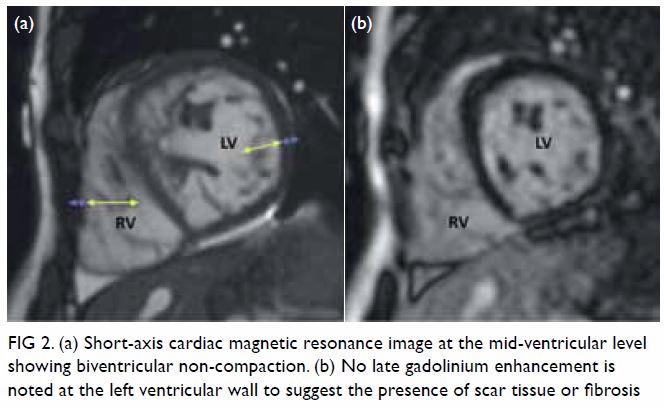
Figure 2. (a) Short-axis cardiac magnetic resonance image at the mid-ventricular level showing biventricular non-compaction. (b) No late gadolinium enhancement is noted at the left ventricular wall to suggest the presence of scar tissue or fibrosis
Ventricular NC of the myocardium, also known as
spongiform cardiomyopathy, is a rare cardiomyopathy arising from arrested
endomyocardial development during embryogenesis,1
with an incidence of approximately 0.05%.2
Non-compaction is a group of genetically heterogeneous disorders and can
be inherited in autosomal dominant, autosomal recessive and X-linked
recessive pattern.3 However, the
majority of NC have idiopathic pathogenesis, and the diagnostic yield of
gene panel testing in LVNC is low (~9%). Patients with isolated NC are
less likely to have a positive genetic test result.3 Morphologically, NC is characterised by an altered
myocardial wall with resultant prominent trabeculae and deep
intertrabecular recesses,4 leading
to an abnormal thickened bilayer of compacted and non-compacted
myocardium. The LV is more frequently involved and biventricular
involvement is less commonly encountered. The absence of wall thinning, RV
wall motion abnormality or aneurysmal change, although not diagnostic,
suggests an alternative diagnosis to that of arrhythmogenic RV dysplasia.
Principal clinical manifestations of NC include: heart failure,
arrhythmia, cardioembolic events, syncope, and sudden cardiac death.4 Even though our patient had remained asymptomatic prior
to diagnosis, there were notable reductions in LVEF and RVEF, suggesting
heart failure.
Cardiac magnetic resonance in establishing
suspected NC cases would be crucial in: (1) confirming the diagnosis, (2)
establishing residual cardiac function, and (3) determining presence of
other associated cardiac malformations, such as LV outflow tract
abnormalities (eg, bicuspid aortic valve), Ebstein anomaly, tetralogy of
Fallot (more commonly diagnosed at a younger age-group) or coarctation of
the aorta. Cardiac magnetic resonance is also superior to echocardiography
in delineating RV anatomy and function, evaluating RV involvement of NC,
determining presence of intracardiac thrombus and myocardial scarring.
After the above diagnostic considerations have been addressed, management
of biventricular NC may include anticoagulation, treatment of heart
failure, and the placement of implantable cardioverter defibrillator or
pacemaker where clinically appropriate. However, cardiac transplantation
remains as the only definitive treatment of biventricular NC.
Author contributions
All authors had full access to the data,
contributed to the study, approved the final version for publication, and
take responsibility for its accuracy and integrity. All authors
contributed to the concept, image acquisition, image and data
interpretation, drafting of the article, and critical revision for
important intellectual content.
Conflicts of interest
The authors have no conflicts of interest to
disclose.
Funding/support
This research received no specific grant from any
funding agency in the public, commercial, or not-for-profit sectors.
Ethics approval
Patient consent was obtained for the purpose of
this case report.
References
1. Maron BJ, Towbin JA, Thiene G, et al.
Contemporary definitions and classification of the cardiomyopathies: an
American Heart Association scientific statement from the Council on
Clinical Cardiology, Heart Failure and Transplantation Committee; Quality
of Care and Outcomes Research and Functional Genomics and Translational
Biology Interdisciplinary Working Groups; and Council on Epidemiology and
Prevention. Circulation 2006;113:1807-16. Crossref
2. Richardson P, McKenna RW, Bristow M, et
al. Report of the 1995 World Health Organization/International Society and
Federation of Cardiology task force on the definition and classification
of cardiomyopathies. Circulation 1996;93:841-2. Crossref
3. Miller EM, Hinton RB, Czosek R, et al.
Genetic testing in pediatric left ventricular noncompaction. Circ
Cardiovasc Genet 2017;10. pii:e001735. Crossref
4. Odiete O, Nagendra R, Lawson MA, Okafor
H. Biventricular noncompaction cardiomyopathy in a patient presenting with
new onset seizure: case report. Case Rep Cardiol article 2012;2012:924865.
Crossref

