Hong
Kong Med J 2019 Aug;25(4):329.e1-2
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
PICTORIAL MEDICINE
Radiological progression of penicillin-sensitive Staphylococcus
aureus aortitis
S Zheng, MB, BS, MRCP
Department of General Medicine, Sengkang General
Hospital, Singapore
Corresponding author: Dr S Zheng (
zheng.shuwei@singhealth.com.sg)
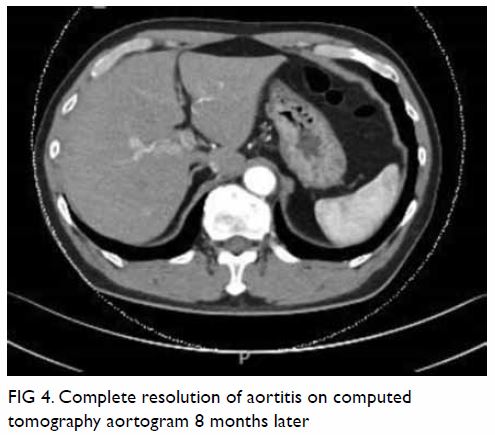
In June 2017, a 58-year-old man, with no known
cardiovascular risk factors, was admitted to a hospital in Singapore, presenting with a 1-week history of fever and progressively
worsening epigastric pain. On the first day of his symptoms, he had
visited the emergency department at another hospital where a computed
tomography (CT) scan of the abdomen performed had not revealed significant
pathology (Fig 1). He was treated symptomatically as for a
viral infection, but he represented to our hospital a week later without
significant symptomatic improvement. The patient had a known history of
reaction to penicillin and a history of traumatic spinal injury more than
20 years ago requiring spinal instrumentation at the L4/5 level. On
examination, the patient was febrile but haemodynamically stable.
Abdominal examination revealed epigastric tenderness on deep palpation.
Cardiorespiratory examination was unremarkable. The patient had
leucocytosis of 15.37 × 103/uL, raised C-reactive protein level
of 109.2 mg/L, and erythrocyte sedimentation rate of 46 mm/h. Renal and
liver function tests, and serum amylase and lipase levels were
unremarkable. He was started empirically on intravenous ceftriaxone
following blood cultures.
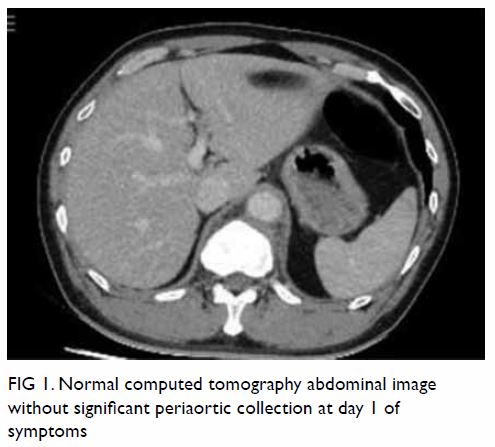
Figure 1. Normal computed tomography abdominal image without significant periaortic collection at day 1 of symptoms
A new CT scan of the abdomen was performed,
revealing an anterior pre- and para-vertebral soft tissue mass with focal
hypodensities surrounding the aorta at the T12-L1 level (Fig
2). Blood culture results (which were received 3 days later) were
positive for penicillin-sensitive Staphylococcus aureus. Magnetic
resonance imaging of the thoracolumbar spine illustrated paravertebral
soft tissue thickening at level of T12-L1 that appears multiloculated with
rim enhancement, suggestive of an underlying paravertebral abscess without
epidural extension. A transthoracic echocardiogram did not reveal any
valvular lesions. The presence of an inflammatory collection around the
aorta prompted concerns for an infectious aortitis.
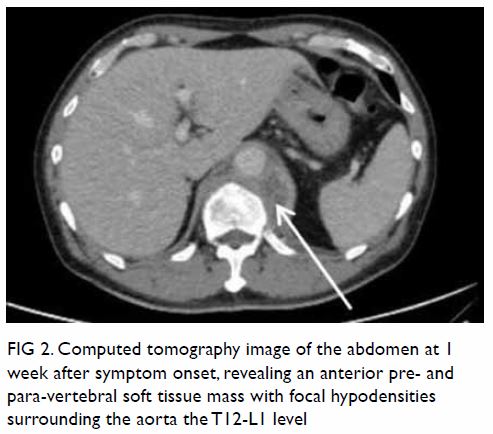
Figure 2. Computed tomography image of the abdomen at 1 week after symptom onset, revealing an anterior pre- and para-vertebral soft tissue mass with focal hypodensities surrounding the aorta the T12-L1 level
Antimicrobial therapy was switched to intravenous
cefazolin, which was continued for 6 weeks with symptomatic improvement.
Repeated blood cultures did not show evidence of persistent S aureus
bacteraemia. Monitoring of C-reactive protein level and erythrocyte
sedimentation rate showed gradual improvement. A CT aortogram, after 6
weeks of parenteral antibiotics, showed interval improvement of the
paravertebral collections and soft tissue thickening around the aorta,
suggesting improving aortitis (Fig 3). Antibiotics were switched to oral
trimethoprim and sulfamethoxazole. Another CT aortogram 8 months later
showed complete resolution of aortitis and paravertebral abscess (Fig
4).
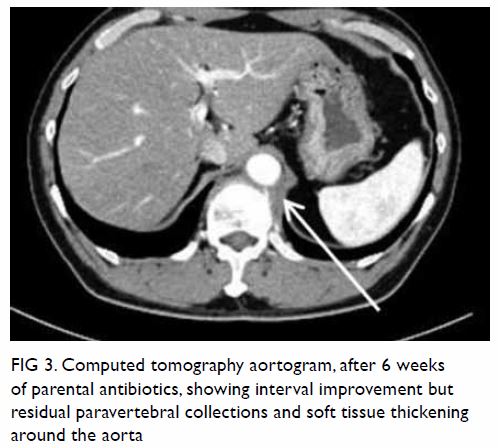
Figure 3. Computed tomography aortogram, after 6 weeks of parental antibiotics, showing interval improvement but residual paravertebral collections and soft tissue thickening around the aorta
In the antibiotic era, infectious aortitis is a
rare clinical entity. Gram-positive micro-organisms are most commonly
implicated, in up to 60% of cases, with S aureus being the most
frequently encountered micro-organism. Other micro-organisms commonly
implicated include Enterococcus species, Streptococcus
pneumoniae, Salmonella species, Mycobacterium tuberculosis, and in
the more distant past, syphilis.1
Rare case reports have featured the radiological evolution of infectious
aortitis while on conservative treatment, and these often illustrate
peri-aortic soft tissue masses progressing to aneurysmal formation from S
aureus or Salmonella species infection.1 2 3 4 5 Prompt antimicrobial therapy is crucial along with
endovascular or surgical intervention.5
Our patient demonstrated radiological normality to pathology within a week
of symptom onset and subsequent improvement while on conservative therapy
alone, followed by full radiological resolution. We believe that his
successful recovery is in part due to early appropriate and prolonged
antimicrobial therapy.
Author contributions
The author designed the study, contributed to
acquisition and analysis of data, drafted the article, and contributed to
the critical revision for important intellectual content. The author had
full access to the data, contributed to the study, approved the final
version for publication, and takes responsibility for its accuracy and
integrity.
Conflicts of interest
The author has disclosed no conflicts of interest.
Funding/support
This research received no specific grant from any
funding agency in the public, commercial, or not-for-profit sectors.
Ethics approval
This study was conducted in accordance with the
principles outlined in the Declaration of Helsinki.
References
1. Cevasco M, Menard MT, Bafford R, McNamee
CJ. Acute infectious pseudoaneurysm of the descending thoracic aorta and
review of infectious aortitis. Vasc Endovascular Surg 2010;44:697-700. Crossref
2. Carreras M, Larena JA, Tabernero G,
Langara E, Pena JM. Evolution of salmonella aortitis towards the formation
of abdominal aneurysm. Eur Radiol 1997;7:54-6. Crossref
3. Rozenblit A, Bennett J, Suggs W.
Evolution of the infected abdominal aortic aneurysm: CT observation of
early aortitis. Abdom Imaging 1996;21:512-4. Crossref
4. Wein M, Bartel T, Kabatnik M, Sadony V,
Dirsch Olaf, Erbel R. Rapid progression of bacterial aortitis to an
ascending aortic mycotic aneurysm documented by transesophageal
echocardiography. J Am Soc Echocardiogr 2001;14:646-9. Crossref
5. Kan CD, Lee HL, Yang YJ. Outcome after
endovascular stent graft treatment for mycotic aortic aneurysm: a
systematic review. J Vasc Surg 2007;46:906-12. Crossref