© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
CASE REPORT
Lysergic acid diethylamide–associated intoxication in
Hong Kong: a case series
C Li, MB, BS1,2; Magdalene HY Tang, PhD1;
YK Chong, FHKCPath, FHKAM (Pathology)1,2; Tina YC
Chan, MB, ChB, PhD1,2; Tony WL Mak, FRCPath, FHKAM (Pathology)1,2
1 Hospital Authority Toxicology
Reference Laboratory, Hong Kong
2 Chemical Pathology Laboratory,
Department of Pathology, Princess Margaret Hospital, Laichikok, Hong Kong
Corresponding author: Dr Tony WL Mak (makwl@ha.org.hk)
Case series
Lysergic acid diethylamide (LSD) is a powerful
hallucinogenic drug that was first synthesised in 1938.1 Although LSD is considered a conventional drug of
abuse, cases of LSD intoxication are scarce in Hong Kong. The Hospital
Authority Toxicology Reference Laboratory—the only tertiary referral
laboratory for toxicological analysis in Hong Kong, established in
2004—did not encounter cases of LSD intoxication until 2015. Between 2015
and 2018, eight cases of LSD-associated intoxication were identified at
five acute hospitals in Hong Kong when LSD and its metabolites were
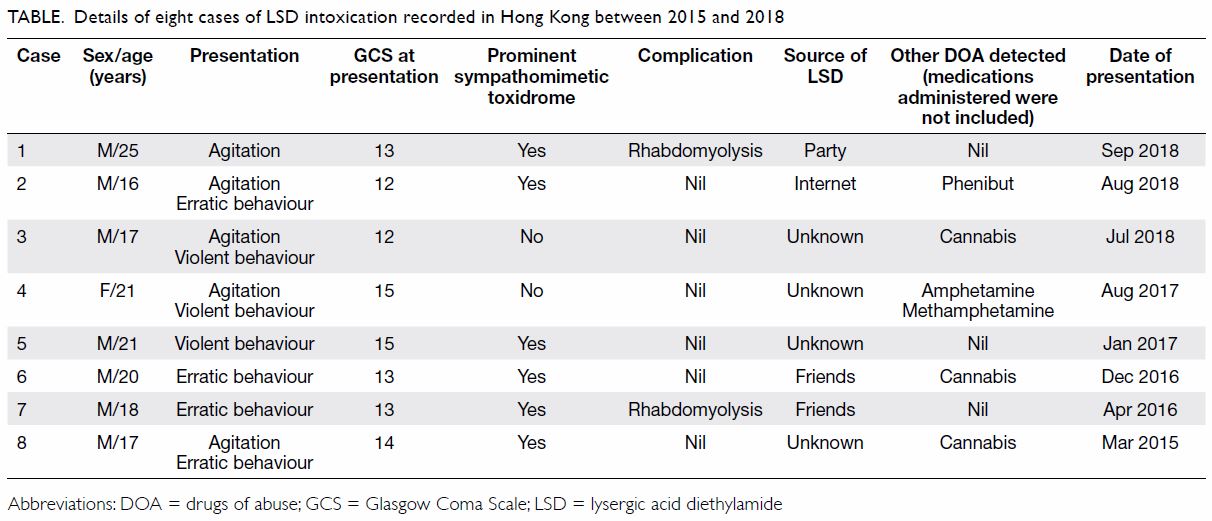
detected in patient urine samples. Details of these eight patients (7
male, 1 female; age range, 16-25 years) are presented in the Table.
The most common presentation of LSD intoxication in these patients was
agitation (63%), followed by erratic behaviour (50%) and violent behaviour
(38%). Impaired level of consciousness (75%) and apparent sympathomimetic
toxidrome (75%) were documented in most patients. History of LSD use was
elicited in all cases. However, only four patients were willing to
volunteer the sources of LSD: one bought LSD from the Internet, one
obtained LSD at a party, and two obtained LSD from friends. The most
common co-ingestant was cannabis, which was detected in three cases.
Amphetamine and methamphetamine were detected in one case. In one patient,
phenibut (3-phenyl-4-aminobutyric acid), a central nervous system
depressant structurally related to gamma-aminobutyric acid, was detected.
Two cases were complicated by rhabdomyolysis and one of them required
intensive care unit admission. The clinical details of these two cases are
presented below.
Case 1
A 25-year-old man who had a history of childhood
asthma presented to Princess Margaret Hospital, Hong Kong, in September
2018 with agitation after sublingual use of LSD on a stamp at a party. At
presentation, his Glasgow Coma Scale was 13/15 (E4, V4, M5). The patient’s
blood pressure was 116/80 mm Hg, heart rate was 150 beats per minute, body
temperature was 39.2℃, and pupil sizes were 5 mm bilaterally. Biochemical
investigations showed a peak creatine kinase (CK) value of 6260 U/L, and
urine myoglobin was positive. The patient was intubated and treated with
alkaline diuresis in the intensive care unit. The urine specimen was
analysed in the Toxicology Reference Laboratory, where LSD, its metabolite
(2-oxo-3-hydroxy-LSD), diazepam, nordiazepam, temazepam, midazolam and
propofol were detected.
Case 2
An 18-year-old man who enjoyed good past health
presented to United Christian Hospital, Hong Kong, in April 2016 with
erratic behaviour after sublingual use of LSD on a stamp obtained from his
friends. At presentation, his Glasgow Coma Scale was 13/15 (E4, V4, M5).
The patient’s blood pressure was 127/50 mm Hg, heart rate was 167 beats
per minute, body temperature was 38.7℃, and pupil sizes were 6 mm
bilaterally. Biochemical investigations showed metabolic acidosis, a peak
CK value of 14 732 U/L, and urine myoglobin was positive. In the urine
specimen, LSD, its metabolite (2-oxo-3-hydroxy-LSD), and lidocaine were
detected.
Discussion
Classically described as a psychedelic or
hallucinogenic agent, LSD is structurally similar to serotonin
(5-hydroxytryptamine), an important neurotransmitter in the central
nervous system. It acts as a serotonin receptor agonist in the central
nervous system and may produce prominent visual hallucinations,
audiovisual synaesthesia, and derealisation. Significant sympathomimetic
stimulation has also been observed.2
The effects typically begin within 30 to 60 minutes, peak at around 2
hours and can last for up to 12 hours after intake.2 These effects are consistent with the current findings
that most patients presented with apparent sympathomimetic toxidrome,
characterised by tachycardia, hypertension, mydriasis, and pyrexia.
There is a general impression promulgated over the
Internet and by celebrities that LSD is harmless and even beneficial to
personal development. Recently, LSD has re-emerged as a micro-dosing
psychedelic. People consume regular low doses of LSD in an attempt to
boost their creativity.3 However,
this practice, also described as the Silicon Valley trend, lacks
scientific evidence. These factors appear to have misled the public into
underestimating the potential sequelae of LSD abuse. In contrast, our case
series clearly demonstrates that LSD intoxication is associated with
severe sequelae. In both cases complicated with rhabdomyolysis, no other
stimulant-class drugs of abuse were detected, including conventional and
emerging drugs of abuse.4 No better
alterative causes of rhabdomyolysis were identified from the medical or
drug history and biochemical investigations; LSD intoxication was the
major contributing factor to rhabdomyolysis in both cases. Other cases of
LSD-associated rhabdomyolysis have been reported in the literature.5 6 Fortunately,
all patients in our series recovered uneventfully. However, at least one
fatal case has been reported elsewhere.7
Frontline clinicians should be aware that LSD has
re-appeared, disguised as a “safe” drug of abuse associated with multiple
local intoxication cases with severe sequelae including rhabdomyolysis.
Thorough investigations and serial monitoring are required to detect
complications. Urine toxicology is useful to confirm the exposure to drugs
of abuse. However, owing to its high potency, the dosage of LSD taken is
small (in micrograms) and urine levels may be very low.2 A sensitive analytical system is required to detect the
presence of LSD and its metabolite. Public education on the dangers or LSD
abuse, and effective regulatory control by the government sectors are
recommended.
Author contributions
All authors had full access to the data,
contributed to the study, approved the final version for publication, and
take responsibility for its accuracy and integrity.
Concept or design of study: All authors.
Acquisition of data: All authors.
Analysis or interpretation of data: All authors.
Drafting of the article: C Li, MHY Tang, TWL Mak.
Critical revision for important intellectual content: All authors.
Acquisition of data: All authors.
Analysis or interpretation of data: All authors.
Drafting of the article: C Li, MHY Tang, TWL Mak.
Critical revision for important intellectual content: All authors.
Conflicts of interest
All authors have disclosed no conflicts of
interest.
Funding/support
This research received no specific grant from any
funding agency in the public, commercial, or not-for-profit sectors.
Ethics approval
Ethics approval for this study was granted by the
Hong Kong Hospital Authority Kowloon West Cluster Research Ethics
Committee (Ref KW/EX-19-003). The Committee exempted the study group from
obtaining patient consent.
References
1. Nichols DE, Grob CS. Is LSD toxic?
Forensic Sci Int 2018;284:141-5. Crossref
2. Dolder PC, Schmid Y, Steuer AE, et al.
Pharmacokinetics and pharmacodynamics of lysergic acid diethylamide in
healthy subjects. Clin Pharmacokinet 2017;56:1219-30. Crossref
3. Anderson T, Petranker R, Rosenbaum D, et
al. Microdosing psychedelics: personality, mental health, and creativity
differences in microdosers. Psychopharmacology (Berl) 2019;236:731-40. Crossref
4. Tang M, Ching CK, Tse ML, et al.
Surveillance of emerging drugs of abuse in Hong Kong: validation of an
analytical tool. Hong Kong Med J 2015;21:114-23. Crossref
5. Mercieca J, Brown EA. Acute renal
failure due to rhabdomyolysis associated with use of a straitjacket in
lysergide intoxication. Br Med J (Clin Res Ed) 1984;288:1949-50. Crossref
6. Berrens Z, Lammers J, White C.
Rhabdomyolysis after LSD ingestion. Psychosomatics 2010;51:356-356.e3. Crossref
7. Fysh RR, Oon MC, Robinson KN, Smith RN,
White PC, Whitehouse MJ. A fatal poisoning with LSD. Forensic Sci Int
1985;28:109-13. Crossref