Hong
Kong Med J 2019 Aug;25(4):271–8 | Epub 5 Aug 2019
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE
Prevalence of obstetric anal sphincter injury following
vaginal delivery in primiparous women: a retrospective analysis
Sonia PK Kwok, MB, ChB, MRCOG; Osanna YK Wan,
FHKAM (Obstetrics and Gynaecology), FHKCOG; Rachel YK Cheung, FHKAM
(Obstetrics and Gynaecology), FHKCOG; LL Lee, MSc; Jacqueline PW Chung,
FHKAM (Obstetrics and Gynaecology), FHKCOG; Symphorosa SC Chan, MD, FRCOG
Department of Obstetrics and Gynaecology, The
Chinese University of Hong Kong, Shatin, Hong Kong
Corresponding author: Dr Symphorosa SC Chan (symphorosa@cuhk.edu.hk)
Abstract
Introduction: Obstetric anal
sphincter injuries (OASIS) may be underdetected in primiparous women.
This study evaluated the prevalence of OASIS in primiparous women after
normal vaginal delivery or instrumental delivery using endoanal
ultrasound (US) during postnatal follow-up.
Methods: This study
retrospectively analysed endoanal US data collected during postnatal
follow-up (6-12 months after vaginal delivery) at a tertiary hospital in
Hong Kong. Offline analysis to determine the prevalence of OASIS was
performed by two researchers who were blinded to the clinical diagnosis.
Symptoms of faecal and flatal incontinence were assessed with the Pelvic
Floor Distress Inventory.
Results: Of 542 women included
in the study, 205 had normal vaginal delivery and 337 had instrumental
delivery. The prevalence of OASIS detected by endoanal US was 7.8% (95%
confidence interval [CI]=4.1%-11.5%) in the normal vaginal delivery
group and 5.6% (95% CI=3.1%-8.1%) in the instrumental delivery group.
Overall, 82.9% of women with OASIS on endoanal US did not show clinical
signs of OASIS. Birth weight was significantly higher in the OASIS group
(P=0.012). At 6 to 12 months after delivery, 5.5% of women reported
faecal incontinence and 17.9% reported flatal incontinence, but OASIS
was not associated with these symptoms.
Conclusions: Additional training
for midwives and doctors may improve OASIS detection.
New knowledge added by this study
- The prevalence of obstetric anal sphincter injury in primiparous women was 7.8% in the normal vaginal delivery group and 5.6% in the instrumental delivery group.
- Most obstetric anal sphincter injuries, as determined by endoanal ultrasound, were not detected clinically. At 6 to 12 months after delivery, obstetric anal sphincter injuries were not associated with symptoms of faecal or flatal incontinence, but a longer-term study is needed to confirm these findings.
- Obstetric anal sphincter injuries occur at similar rates during normal vaginal delivery and instrumental delivery. Detailed vaginal and rectal examinations are recommended after both types of deliveries.
- Additional training for midwives and doctors may improve the detection of obstetric anal sphincter injury.
Introduction
Obstetric anal sphincter injuries (OASIS) is a
serious complication of vaginal delivery that is associated with an
increased risk of anal incontinence (complaint of involuntary loss of
faeces or flatus).1 The incidence
of OASIS is reportedly much lower in Hong Kong (0.32%) than in other
countries, such as the United Kingdom, Norway, and Sweden (2.9%-4.2%).2 3 4 5 This could be
affected by a number of factors. First, delivery practices in Hong Kong
are quite different from elsewhere in the world, such that they include
the use of a hands-on approach to protect the perineum and liberal use of
episiotomy.6 The episiotomy rates
are reportedly high in Hong Kong: 83.7% for primiparous women and 54.8%
for multiparous women.5 Moreover,
in Hong Kong, a left mediolateral episiotomy is used, whereas midline
episiotomy or right mediolateral episiotomy are used in many other parts
of the world.7 Second, there may be
ethnic differences in pelvic floor biometry. In particular, Chinese women
have a smaller hiatal dimension and reduced pelvic organ mobility.8 It is unclear how these differences in practice and
pelvic floor biometry influence the incidence of OASIS.
Importantly, it is also possible that the reduced
incidence of OASIS in Hong Kong is a result of underdetection. In a recent
local prospective observational study, women were assessed by a single
experienced clinician via rectal examination after either normal or
instrumental vaginal delivery; the results of that study showed that the
incidence of OASIS in primiparous Asian women in Hong Kong was 10%,6 which suggests that the OASIS rate might be higher than
previously published. Obstetric anal sphincter injuries that are
identified after an extended interval (such as during postnatal follow-up)
is regarded as occult OASIS. There is limited information in the
literature regarding occult OASIS; thus far, studies have been conducted
in the United Kingdom and Australia.9
10
The use of endoanal ultrasound (US) may facilitate
identification of OASIS.11
Endoanal US comprises a non-invasive assessment modality and is regarded
as the gold standard in studies of anal sphincter injury.9 11 Moreover,
all cases of clinically identified OASIS can also be identified on
endoanal US.9 The aim of this study
was to determine the prevalence of OASIS in primiparous women after normal
vaginal delivery or instrumental delivery using endoanal US during
postnatal follow-up. Understanding the prevalence and detection rates of
OASIS can help inform training policies for midwives and doctors on the
awareness and detection of OASIS.
Methods
Patients and study design
This was a retrospective analysis of archived US
volumes from two previously published studies that were performed at a
tertiary university hospital in Hong Kong. The initial study recruited 442
nulliparous women in the first trimester, during the period from August
2009 to September 2010.12 13 The second study recruited 292 primiparous women at 1
to 3 days after instrumental delivery, during the period from September
2011 to May 2012. None of the women in either study reported symptoms of
pelvic floor disorders, including faecal incontinence to solid or loose
stool, before pregnancy.14 Details
of deliveries, including any occurrence of perineal tearing, were recorded
after each delivery. Ethics approval was obtained from The Joint Chinese
University of Hong Kong–New Territories East Cluster Clinical Research
Ethics Committee (Ref CRE-2013.332). The STROBE (Strengthening the
Reporting of Observational Studies in Epidemiology) guidelines were
followed in the preparation of this report.15
Delivery and immediate assessment
Generally, each woman underwent perineal
examination by the attending midwife or doctor who conducted the delivery,
immediately after vaginal delivery. This information was immediately
recorded in the medical record. Third- or fourth-degree tears were
assessed and repaired by a trained obstetrician. The anorectal mucosa was
repaired by continuous or interrupted sutures with 3-O Vicryl. Internal
anal sphincter tears were repaired separately by interrupted end-to-end
sutures with 2-O Vicryl. External anal sphincter (EAS) tears were repaired
by overlapping or end-to-end sutures with 2-O Vicryl. Perineal muscles and
the vagina were repaired with 2-O Vicryl. The diagnosis and operative
record of each woman were immediately entered into the electronic medical
record. The degree of perineal tear was defined using Sultan’s
classification of perineal trauma.16
Follow-up assessment
During postnatal follow-up (6-12 months after
delivery), the urinary, bowel, and prolapse symptoms of each woman, as
well as their quality of life, were assessed using the Chinese Pelvic
Floor Distress Inventory (PFDI) and Pelvic Floor Impact Questionnaire
(PFIQ).17 Assessment of the anal
sphincter was performed with endoanal US using a 10-MHz 360-degree
rotating probe (Focus 400, BK Medical; Gentofte, Denmark) with the woman
in the lithotomy position. Automatic image acquisition was performed with
two volumes stored for each woman.
Blinded offline analysis of endoanal ultrasound
Offline analysis of the endoanal US volumes was
performed in 2018 by two experienced obstetricians (OYKW, SSCC) who were
blinded to the clinical diagnosis and questionnaire information. An anal
sphincter defect was defined as a discontinuity of >30 degrees in
endosonographic images of the internal (hypoechoic ring) and/or external
(mixed echogenic ring) sphincters.18
A partial-thickness EAS injury was defined as a defect of <50%
thickness of the EAS, whereas a defect of >50% of the EAS was regarded
as a full-thickness injury. We considered any EAS and/or internal anal
sphincter injury to be OASIS. This follows the clinical classification of
OASIS by Sultan.16 Each researcher
reviewed all endoanal US volumes independently. Any discrepancies were
resolved by consensus review of the relevant US volumes.
Definitions of incontinence
The PFDI and PFIQ are comprehensive validated
instruments which assess the symptoms and impact of pelvic floor
disorders.17 In this study, faecal
incontinence was defined as an affirmative response to either item 38 (“Do
you usually lose stool beyond your control if your stool is well formed?”)
or item 39 (“Do you lose stool beyond your control if your stool is loose
or liquid?”) of the PFDI. Flatal incontinence was defined as an
affirmative response to item 40 (“Do you usually lose gas from the rectum
beyond your control?”) of the PFDI.
Statistical analysis
Data were analysed by SPSS (Window version 22.0;
IBM Corp, Armonk [NY], United States). Descriptive analyses were used to
study the prevalence of OASIS on endoanal US. Means were compared between
groups using the independent-samples t test. Comparisons of
frequencies were made using the Chi squared test or Fisher’s exact test,
where appropriate. Univariate analysis was performed to evaluate the
influence of potential risk factors on OASIS. Differences with P<0.05
were considered to be statistically significant. Power calculations were
not performed with regard to this specific research question, as this
study comprised a subanalysis of two prior projects, as described earlier
in this paper.
Results
Patient characteristics
A total of 544 women who had vaginal delivery were
enrolled in this study; 207 had normal vaginal delivery and 337 had
instrumental delivery (285 vacuum extraction, 52 forceps). Ultrasound
images were suboptimal for two women who had normal vaginal delivery;
these women were excluded from the analysis.
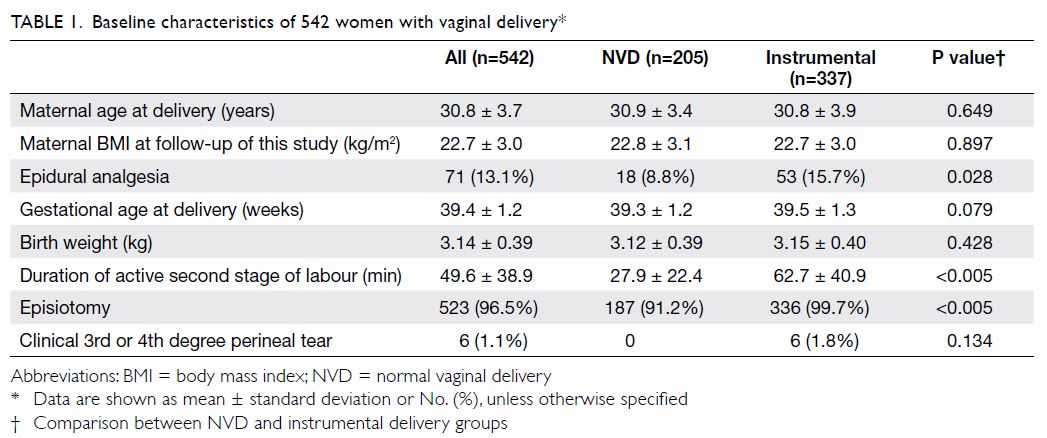
The demographic data and delivery information are
shown in Table 1. Left mediolateral episiotomy was performed
in 187 (91.2%) women in the normal vaginal delivery and 336 (99.7%) women
in the instrumental delivery group. The duration of active second stage
was longer in the instrumental delivery group than in the normal vaginal
delivery group (62.7 ± 40.9 min vs 27.9 ± 22.4 min, P<0.005), as a
prolonged second stage was the most common indication for instrumental
delivery in this cohort (48.4%). More women had epidural analgesia in the
instrumental delivery group than in the normal vaginal delivery group
(15.7% vs 8.8%, P=0.028). There was no significant difference between the
normal vaginal delivery and instrumental delivery groups regarding the
timing of endoanal US assessment (P=0.22).
Endoanal ultrasound findings and relationship of
obstetric anal sphincter injuries with delivery factors
The Figure shows endoanal US images of intact anal
sphincters, as well as sphincters with different degrees of OASIS. There
were discrepancies or uncertainties in the endoanal US analysis of 16
women with respect to the diagnosis of OASIS. The two researchers
determined the diagnoses of these women by consensus review; six were
diagnosed with OASIS and 10 were regarded as normal.
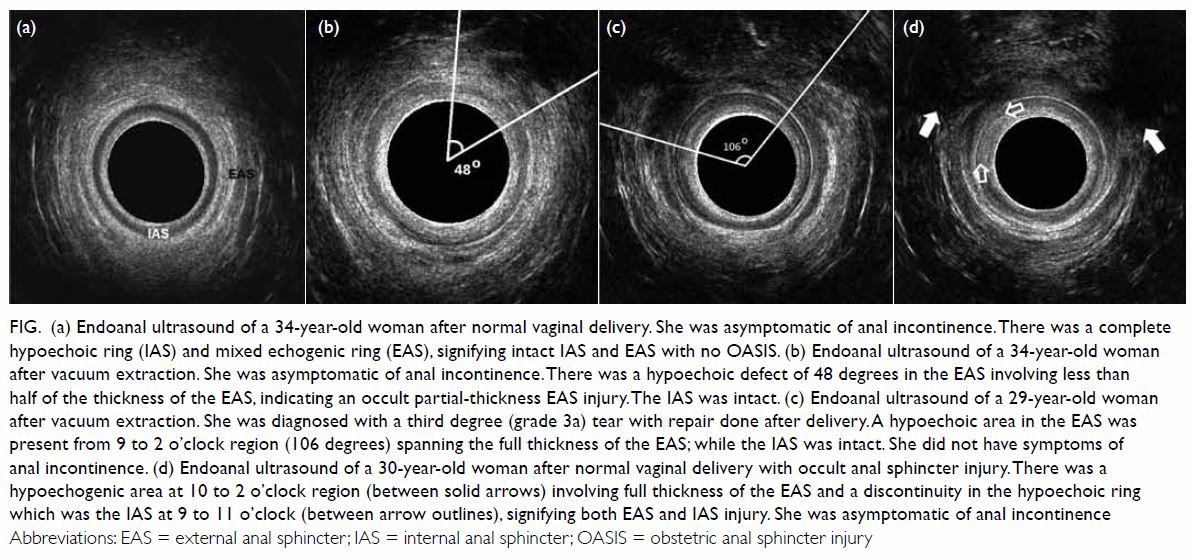
Figure. (a) Endoanal ultrasound of a 34-year-old woman after normal vaginal delivery. She was asymptomatic of anal incontinence. There was a complete hypoechoic ring (IAS) and mixed echogenic ring (EAS), signifying intact IAS and EAS with no OASIS. (b) Endoanal ultrasound of a 34-year-old woman after vacuum extraction. She was asymptomatic of anal incontinence. There was a hypoechoic defect of 48 degrees in the EAS involving less than half of the thickness of the EAS, indicating an occult partial-thickness EAS injury. The IAS was intact. (c) Endoanal ultrasound of a 29-year-old woman after vacuum extraction. She was diagnosed with a third degree (grade 3a) tear with repair done after delivery. A hypoechoic area in the EAS was present from 9 to 2 o’clock region (106 degrees) spanning the full thickness of the EAS; while the IAS was intact. She did not have symptoms of anal incontinence. (d) Endoanal ultrasound of a 30-year-old woman after normal vaginal delivery with occult anal sphincter injury. There was a hypoechogenic area at 10 to 2 o’clock region (between solid arrows) involving full thickness of the EAS and a discontinuity in the hypoechoic ring which was the IAS at 9 to 11 o’clock (between arrow outlines), signifying both EAS and IAS injury. She was asymptomatic of anal incontinence
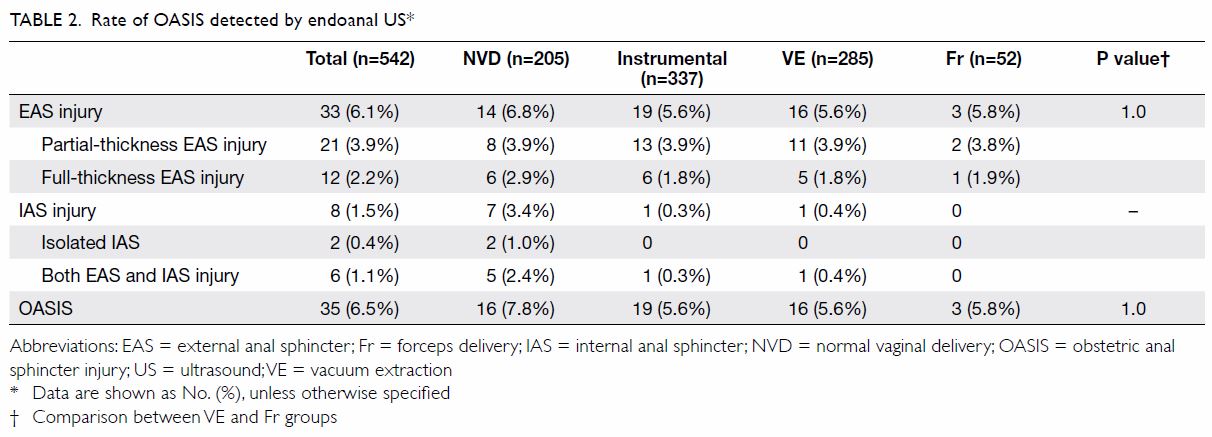
The prevalence of clinically detected OASIS was 0%
in the normal vaginal delivery group and 1.8% (n=6) in the instrumental
delivery group. Table 2 shows that the prevalence of OASIS detected
by endoanal US was 7.8% (n=16; 95% confidence interval [CI]=4.1%-11.5%) in
the normal vaginal delivery group and 5.6% (n=19; 95% CI=3.1%-8.1%) in the
instrumental delivery group (P=0.415). Twenty-nine (82.9%) women had
OASIS, as detected by endoanal US, that was not diagnosed during clinical
assessment immediately after delivery. Therefore, the occult OASIS rate
was 7.8% (95% CI=4.1%-11.5%) in the normal vaginal delivery group and 3.8%
(95% CI=1.8%-5.8%) in the instrumental delivery group. In addition, 63.6%
(n=21) of occult EAS injuries comprised partial-thickness EAS injuries,
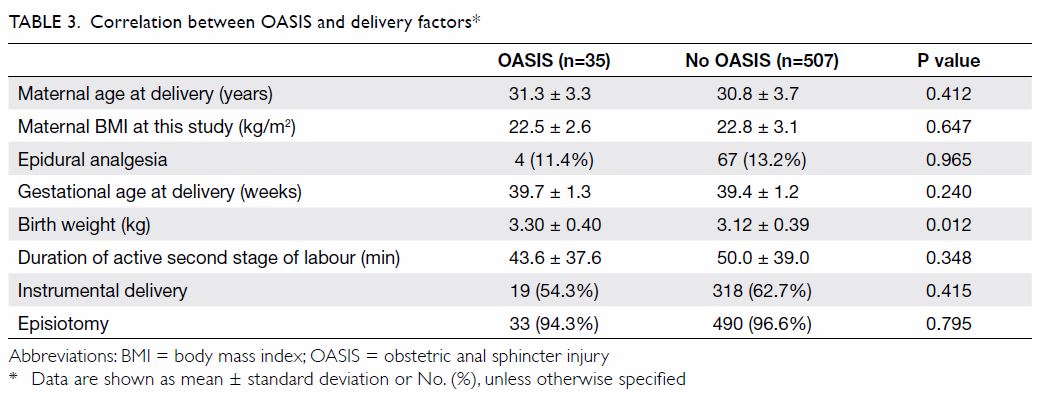
whereas 36.4% (n=12) comprised full-thickness EAS injuries. When women
with OASIS were compared to those without OASIS, increased birth weight
was the only delivery factor associated with an increased risk of OASIS
(odds ratio [OR]=3.1, 95% CI=1.3%-7.6%, P=0.012) [Table 3].
Relationships of faecal and flatal incontinence
symptoms with obstetric anal sphincter injuries
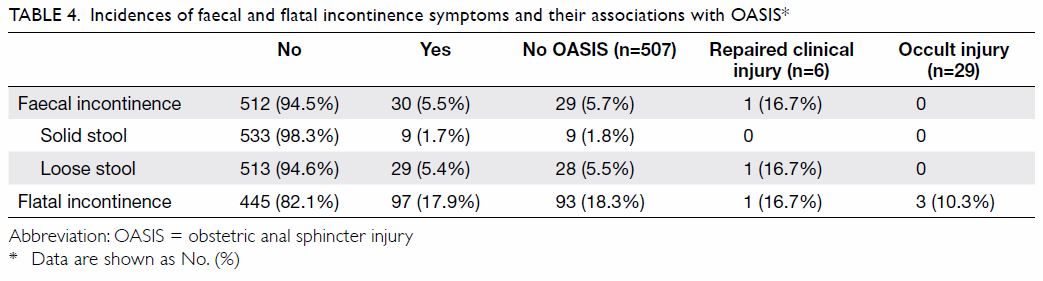
Overall, nine (1.7%) and 29 (5.4%) women reported
faecal incontinence to solid and loose stool, whereas 97 (17.9%) women
reported flatal incontinence (Table 4). All affected women reported mild symptoms.
Among the women with OASIS, only one (2.9%) with a repaired third degree
(3a) tear reported symptoms of both (faecal incontinence to loose stool
and flatal incontinence). Three women (10.3%) who had occult injury
reported flatal incontinence. There were no associations between the
presence of OASIS and faecal incontinence (P=0.71) or between the presence
of OASIS and flatal incontinence (P=0.37).
Discussion
Primiparity has been associated with increased
risks of OASIS (ORs of 2.39 and 8.34) in large retrospective studies.19 20 In the
present study, which included large number of primiparous women, the
findings on endoanal US were compared with women’s reported symptoms of
faecal and flatal incontinence. Importantly, there were no associations
between faecal or flatal incontinence and the presence of OASIS.
After assessment by endoanal US, the prevalence of
OASIS in the normal vaginal delivery group increased from 0% to 7.8% and
that in the instrumental delivery group increased from 1.8% to 5.6%.
Overall, 82.9% of women with OASIS detected by endoanal US had not been
diagnosed with OASIS during clinical assessment immediately after
delivery. This finding is consistent with the results of the study by
Andrews et al.9 In that study, the
prevalence of OASIS markedly increased from 11% to 24.5% when women were
re-examined by an experienced research fellow; 87% of OASIS diagnoses were
missed by midwives and 28% were missed by junior doctors.9 In our study, normal vaginal deliveries were primarily
attended by midwives, whereas instrumental deliveries were performed by
residents. The higher rate of occult OASIS in the normal vaginal delivery
group suggests that midwives currently receive inadequate training for
clinical identification of OASIS. Thus, to improve the detection of OASIS,
midwives and doctors should be trained to recognise OASIS by performing a
standardised vaginal and rectal examination after delivery.
Compared with previous studies, the rate of OASIS
determined by endoanal US in our study (6.5%) was lower than the rate of
10% determined by a single examiner in a prospective observational study
conducted in the same unit.6 This
could be a result of the small sample size (70 subjects) in the prior
study. Furthermore, most patients with OASIS (5/7) in that study were
reported to have small 3a tears. There were no 3c or fourth-degree tears
in that study. Following the same delivery practices, clinically detected
small 3a tears may therefore appear normal in endoanal US. Furthermore,
these tears might not result in long-term consequences.6 21
The finding of an overall lower OASIS rate in Hong
Kong, compared with that in Asian women who deliver in Caucasian
countries, is not new.6 Asian women
who deliver in locations with more restrictive policies regarding
episiotomy have shown higher rates of OASIS.22
23 24
In a study conducted in the United States, OASIS was found significantly
more frequently in Asian women than in women of other ethnicities.23 In Australia, nulliparous women born in South Asia
and South-East Asia were 2.6-fold and 2.1-fold more likely to exhibit
OASIS than women born in Australia or New Zealand women.24 It is uncertain whether the increased rate of
episiotomy might protect against OASIS in Asian women and contribute to
the relative reduction in the rate of OASIS in Hong Kong. Thus, our unit
is currently conducting a randomised controlled trial to compare
restrictive and routine episiotomy. In addition to episiotomy, the
delivery technique and hands-on approach might contribute to the relative
reduction in the rate of OASIS. All deliveries in our study were conducted
with women in a lithotomy position, with their feet on footplates or in
stirrups. All midwives and doctors conducting the deliveries used hands-on
techniques to protect the perineum in each woman. Either firm pressure or
pressure with squeezing of the perineum, also known as the modified Ritgen
manoeuvre, was used.6 Warm
compresses were not commonly used by midwives and doctors in our study.
The OASIS rate in the normal vaginal delivery group
was higher than that in the the instrumental delivery group, but this
difference was not statistically significant. The majority of deliveries
by women in the instrumental delivery group were performed using vacuum
extraction. The rate of OASIS in these women could be similar to that of
women in the normal vaginal delivery group. The OASIS rates were similar
in women who delivered with the aid of vacuum extraction or with forceps,
whereas previous studies showed that forceps delivery was associated with
an increased risk of OASIS.19 20 25
The small number of forceps deliveries in this study might have led to
insufficient statistical power to detect a difference between the two
types of instrumental deliveries. Furthermore, the use of forceps was
primarily restricted to patients who were low risk, and mostly comprised
outlet/low-cavity forceps deliveries. Previous studies reported that
macrosomia, higher birth weight (OR=1.14, 95% CI=1.0-1.3, P=0.039), and
shorter perineal length were risk factors for OASIS.6 19 20 The present study had similar findings, in that
higher birth weight was a risk factor for OASIS (OR=3.1, 95% CI=1.3-7.6,
P=0.012). However, perineal length was not assessed, which is an important
limitation of this study.
Flatal incontinence was present in 17.9% of women
after delivery, which is comparable to the rate reported in previous
studies.26 27 In addition to OASIS, irritable bowel syndrome, high
body mass index, and mode of delivery constitute factors associated with
flatal incontinence.20 21 Overall, 5.5% of women reported faecal incontinence;
most of these women reported faecal incontinence to loose stool and mild
symptoms only. Most obstetric anal sphincter injuries were not detected
during clinical examination. Shortly after delivery, the presence of OASIS
was not associated with symptoms of faecal or flatal incontinence, but a
longer-term study is needed to confirm these findings. However, we
previously found that only antenatal faecal incontinence symptoms
increased the likelihood of faecal incontinence at 12 months after
delivery (OR=6.1, 95% CI=1.8-21.5, P=0.005), whereas maternal
characteristics, mode of delivery, and the presence of OASIS did not.28 In longer-term follow-up (3-5 years after delivery),
2.1% and 5.9% of women who had one vaginal delivery reported faecal
incontinence to solid and loose stool, respectively.29
To the best of our knowledge, there have been no
randomised controlled trials regarding the optimal timing for the use of
endoanal US to assess OASIS after vaginal delivery. One randomised
controlled trial has been conducted to compare clinical examination alone
(control group) and clinical examination with additional endoanal US
immediately after delivery (intervention group).30
31 The results of that study
showed that US performed immediately after delivery—before repair—might
detect more cases of OASIS: 5.6% of women were found to have
full-thickness OASIS that was not recognised during clinical examination
alone.31 However, the study also
showed that five of 21 women underwent unnecessary intervention, as the
sonographic defect could not be clinically located, despite surgical
exploration.31 Therefore, the use
of endoanal US immediately after delivery and before repair was not
recommended.
Women with OASIS should undergo follow-up after
delivery to assess symptoms of faecal incontinence. Currently, there is no
consensus regarding the optimal mode of delivery for these women in
subsequent pregnancies. Scheer et al32
and Karmarkar et al33 assessed
women who had OASIS in subsequent pregnancies using a questionnaire,
endoanal US, and manometry. Vaginal delivery was recommended for
asymptomatic women with normal findings. Women were reassessed after
subsequent deliveries. There were no statistically significant differences
in anal manometry findings, anal symptoms, or quality of life following
subsequent vaginal delivery or caesarean section.32
33 In the study by Scheer et al,32 new OASIS occurred in only one
woman after a vaginal delivery. Therefore, decisions regarding the mode of
delivery for subsequent pregnancies after OASIS should be based on
clinical symptoms, anal manometry, and endoanal US. This would help to
preserve anal sphincter function and avoid unnecessary caesarean sections.
Currently, the value of the above assessments is limited in Hong Kong. The
significance of an incidental finding of occult anal sphincter defect
remains uncertain.
Conclusion
The prevalence of OASIS determined by endoanal US
was higher than the rate determined by clinical practice. This may
indicate that additional training for midwives and doctors may be required
to improve the detection of OASIS. At 6 to 12 months after delivery, OASIS
was not associated with symptoms of faecal or flatal incontinence, but a
longer-term study is needed to confirm these findings.
Author contributions
All authors had full access to the data,
contributed to the study, approved the final version for publication, and
take responsibility for its accuracy and integrity.
Concept or design of the study: RYK Cheung, SSC
Chan.
Acquisition of data: OYK Wan, RYK Cheung, LL Lee, SSC Chan.
Analysis or interpretation of data: SPK Kwok, SSC Chan.
Drafting of the article: All authors.
Critical revision for important intellectual content: SPK Kwok, OYK Wan, RYK Cheung, SSC Chan.
Acquisition of data: OYK Wan, RYK Cheung, LL Lee, SSC Chan.
Analysis or interpretation of data: SPK Kwok, SSC Chan.
Drafting of the article: All authors.
Critical revision for important intellectual content: SPK Kwok, OYK Wan, RYK Cheung, SSC Chan.
Declaration
The results from this research have been presented,
in part, at the following conferences:
1. Wan OYK, Cheung RYK, Chan SSC. 6th Annual Meeting of the Asia-Pacific Urogynecology Association and 13th Japanese Society of Pelvic Organ Prolapse Surgery Joint Conference–Young Doctors Session. Okinawa, Japan, 22-24 March 2019 (oral abstract presentation).
2. Wan OYK, Kwok SPK, Cheung RYK, Chan SSC. Hospital Authority Convention 2019, Hong Kong, 14-15 May 2019 (e-poster presentation).
3. Kwok SPK, Wan OYK, Cheung RYK, Lee LL, Chung JPW, Chan SSC. Obstetrical and Gynaecological Society of Hong Kong Annual Scientific Meeting 2019, Hong Kong, 1-2 June 2019 (oral presentation).
1. Wan OYK, Cheung RYK, Chan SSC. 6th Annual Meeting of the Asia-Pacific Urogynecology Association and 13th Japanese Society of Pelvic Organ Prolapse Surgery Joint Conference–Young Doctors Session. Okinawa, Japan, 22-24 March 2019 (oral abstract presentation).
2. Wan OYK, Kwok SPK, Cheung RYK, Chan SSC. Hospital Authority Convention 2019, Hong Kong, 14-15 May 2019 (e-poster presentation).
3. Kwok SPK, Wan OYK, Cheung RYK, Lee LL, Chung JPW, Chan SSC. Obstetrical and Gynaecological Society of Hong Kong Annual Scientific Meeting 2019, Hong Kong, 1-2 June 2019 (oral presentation).
Conflicts of interest
As an editor of the journal, JPW Chung was not
involved in the peer review process. Other authors have disclosed no
conflicts of interest.
Funding/support
This research received no specific grant from any
funding agency in the public, commercial, or not-for-profit sectors.
Ethics approval
Ethics approval was obtained from local institute,
The Joint Chinese University of Hong Kong–New Territories East Cluster
Clinical Research Ethics Committee (Ref CRE-2013.332). Written informed
consent was obtained from all participants.
References
1. Fenner DE, Genberg B, Brahma P, Marek L,
DeLancey JO. Fecal and urinary incontinence after vaginal delivery with
anal sphincter disruption in an obstetrics unit in the United States. Am J
Obstet Gynecol 2003;189:1543-50. Crossref
2. Thiagamoorthy G, Johnson A, Thakar R,
Sultan AH. National survey of perineal trauma and its subsequent
management in the United Kingdom. Int Urogynecol J 2014;25:1621-7. Crossref
3. Baghestan E, Irgens LM, Børdahl PE,
Rasmussen S. Trends in risk factors for obstetric anal sphincter injuries
in Norway. Obstet Gynecol 2010;116:25-34. Crossref
4. Ekéus C, Nilsson E, Gottvall K.
Increasing incidence of anal sphincter tears among primiparas in Sweden: a
population-based register study. Acta Obstet Gynecol Scand 2008;87:564-73.
Crossref
5. Hong Kong College of Obstetricians and
Gynaecologists. Territory-wide audit in Obstetrics & Gynaecology;
2009.
6. Bates LJ, Melon J, Turner R, Chan SS,
Karantanis E. Prospective comparison of obstetric anal sphincter injury
incidence between an Asian and Western hospital. Int Urogynecol J
2019;30:429-37. Crossref
7. Carroli G, Mignini L. Episiotomy for
vaginal birth. Cochrane Database Syst Rev 2009;(1):CD000081. Crossref
8. Cheung RY, Shek KL, Chan SS, Chung TK,
Dietz HP. Pelvic floor muscle biometry and pelvic organ mobility in East
Asian and Caucasian nulliparae. Ultrasound Obstet Gynecol 2015;45:599-604.
Crossref
9. Andrews V, Sultan AH, Thakar R, Jones
PW. Occult anal sphincter injuries—myth or reality? BJOG 2006;113:195-200.
Crossref
10. Guzmán Rojas RA, Shek KL, Langer SM,
Dietz HP. Prevalence of anal sphincter injury in primiparous women.
Ultrasound Obstet Gynecol 2013;42:461-6. Crossref
11. Sultan AH, Kamm MA, Hudson CN, Thomas
JM, Bartram CI. Anal-sphincter disruption during vaginal delivery. N Engl
J Med 1993;329:1905-11. Crossref
12. Chan SS, Cheung RY, Yiu KW, Lee LL,
Leung TY, Chung TK. Pelvic floor biometry during first singleton pregnancy
and the relationship with symptoms of pelvic floor disorders: a
prospective observational study. BJOG 2014;121:121-9. Crossref
13. Chan SS, Cheung RY, Yiu KW, Lee LL,
Chung TK. Pelvic floor biometry in Chinese primiparous women 1 year after
delivery: a prospective observational study. Ultrasound Obstet Gynecol
2014;43:466-74. Crossref
14. Chung MY, Wan OY, Cheung RY, Chung TK,
Chan SS. Prevalence of levator ani muscle injury and health-related
quality of life in primiparous Chinese women after instrumental delivery.
Ultrasound Obstet Gynecol 2015;45:728-33. Crossref
15. von Elm E, Altman DG, Egger M, Pocock
SJ, Gøtzsche PC, Vandenbroucke JP; STROBE Initiative. The Strengthening
the Reporting of Observational Studies in Epidemiology (STROBE) statement:
guidelines for reporting observational studies. J Clin Epidemiol
2008;61:344-9. Crossref
16. Sultan AH. Obstetric perineal injury
and anal incontinence. Clinical Risk 1999;5:193-6. Crossref
17. Chan SS, Cheung RY, Yiu AK, et al.
Chinese validation of Pelvic Floor Distress Inventory and Pelvic Floor
Impact Questionnaire. Int Urogynecol J 2011;22:1305-12. Crossref
18. Roos AM, Thakar R, Sultan A. Outcome
of primary repair of obstetric anal sphincter injuries (OASIS): does the
grade of tear matter? Ultrasound Obstet Gynecol 2010;36:368-74. Crossref
19. de Leeuw JW, Struijk PC, Vierhout ME,
Wallenburg HC. Risk factors for third degree perineal ruptures during
delivery. BJOG 2001;108:383-7. Crossref
20. Aukee P, Sundström H, Kairaluoma MV.
The role of mediolateral episiotomy during labour: analysis of risk
factors for obstetric anal sphincter tears. Acta Obstet Gynecol Scand
2006;85:856-60. Crossref
21. Ramalingam K, Monga AK. Outcomes and
follow-up after obstetric anal sphincter injuries. Int Urogynecol J
2013;24:1495-500. Crossref
22. Hauck YL, Lewis L, Nathan EA, White C,
Doherty DA. Risk factors for severe perineal trauma during vaginal
childbirth: a Western Australian retrospective cohort study. Women Birth
2015;28:16-20. Crossref
23. Grobman WA, Bailit JL, Rice MM, et al.
Racial and ethnic disparities in maternal morbidity and obstetric care.
Obstet Gynecol 2015;125:1460-7. Crossref
24. Davies-Tuck M, Biro MA, Mockler J,
Stewart L, Wallace EM, East C. Maternal Asian ethnicity and the risk of
anal sphincter injury. Acta Obstet Gynecol Scand 2015;94:308-15.Crossref
25. Stedenfeldt M, Øian P, Gissler M, Blix
E, Pirhonen J. Risk factors for obstetric anal sphincter injury after a
successful multicentre interventional programme. BJOG 2014;121:83-91. Crossref
26. Boreham MK, Richter HE, Kenton KS, et
al. Anal incontinence in women presenting for gynecologic care:
prevalence, risk factors, and impact upon quality of life. Am J Obstet
Gynecol 2005;192:1637-42. Crossref
27. Melville JL, Fan MY, Newton K, Fenner
D. Fecal incontinence in US women: a population-based study. Am J Obstet
Gynecol 2005;193:2071-6. Crossref
28. Chan SS, Cheung RY, Yiu KW, Lee LL,
Chung TK. Prevalence of urinary and fecal incontinence in Chinese women
during and after first pregnancy. Int Urogynecol J 2013;24:1473-9. Crossref
29. Ng K, Cheung RY, Lee LL, Chung TK,
Chan SS. An observational follow-up study on pelvic floor disorders to 3-5
years after delivery. Int Urogynecol J 2017;28:1393-9. Crossref
30. Walsh KA, Grivell RM. Use of endoanal
ultrasound for reducing the risk of complications related to anal
sphincter injury after vaginal birth. Cochrane Database Syst Rev
2015;(10):CD010826. Crossref
31. Faltin DL, Boulvain M, Floris LA,
Irion O. Diagnosis of anal sphincter tears to prevent fecal incontinence:
a randomized controlled trial. Obstet Gynecol 2005;106:6-13. Crossref
32. Scheer I, Thakar R, Sultan AH. Mode of
delivery after previous obstetric anal sphincter injuries (OASIS)—a
reappraisal? Int Urogynecol J Pelvic Floor Dysfunct 2009;20:1095-101. Crossref
33. Karmarkar R, Bhide A, Digesu A,
Khullar V, Fernando R. Mode of delivery after obstetric anal sphincter
injury. Eur J Obstet Gynecol Reprod Biol 2015;194:7-10. Crossref