© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
COMMENTARY
Success rate of resuscitation after out-of-hospital
cardiac arrest
Anthony MH Ho, FRCPC, FCCP1; Glenio B
Mizubuti, MSc, MD1; Adrienne K Ho, MB, BS2; Song
Wan, MD, FRCS3; Devin Sydor, MD, FRCPC1; David C
Chung, MD, FRCPC4
1 Department of Anesthesiology and
Perioperative Medicine, Queen’s University, Canada
2 Department of Oncology, The Christie
NHS Foundation Trust, Manchester, United Kingdom
3 Division of Cardiac Surgery,
Department of Surgery, The Chinese University of Hong Kong, Shatin, Hong
Kong
4 Department of Anaesthesia and
Intensive Care, The Chinese University of Hong Kong, Shatin,
Hong Kong
Corresponding author: Prof Glenio B Mizubuti (gleniomizubuti@hotmail.com)
A recent study in Hong Kong documented the low
success rate of resuscitation after adult out-of-hospital cardiac arrest
(OHCA). Survival to hospital discharge with good neurological outcome was
1.5%.1 A median delay of 12 minutes
for defibrillation was one factor that contributed to poor outcomes.1 In ventricular fibrillation or pulseless ventricular
tachycardia, every minute without defibrillation drastically reduces the
chance of successful resuscitation.2
To partially mitigate the delayed arrival of trained personnel to
administer defibrillation,1
widespread deployment of automated external defibrillators (AEDs) in
public places in conjunction with public education is a worthwhile
strategy.3
A 10-year review reported the incidence of OHCA in
Hong Kong children to be 5.37/100 000 person-years.4 Most causes were respiratory (for which immediate
action should be assessment and management of Airway, Breathing, and
Circulation), and only 9.4% of individuals had a shockable rhythm.
Survival with good neurological outcome was 13.2%.4
Cardiopulmonary resuscitation (CPR) is immediately
required while awaiting defibrillation, or when defibrillation is
unsuccessful, when the arrest is of respiratory origin (some 6% of adult
OHCAs and the majority of paediatric arrests4)
or if rhythm is not shockable. The goal of CPR is to oxygenate the heart
and brain until a life-sustaining rhythm and spontaneous circulation can
be restored. Traditionally, CPR started with rescue breathing followed by
breathing and chest compression cycles. However, the current untrained
bystander CPR protocol includes compression-only CPR (CO-CPR) with no
rescue breathing. The reduced emphasis on traditional rescue breathing
aims to increase bystander participation and avoid hyperventilation, and
is based in part on recognition that the blood oxygen level is sufficient
during the first few minutes of abrupt ventricular fibrillation or
pulseless ventricular tachycardia (although this may not apply when the
cardiac arrest is secondary to respiratory causes). Importantly, it
enables chest compression to start immediately and without interruption, a
lack of which is linked to poor outcomes.5
However, because 60% of adult and 38% of paediatric OHCAs in Hong Kong are
unwitnessed,1 4 these first few minutes of sufficient oxygen in the
blood (for sudden arrest of cardiac origin) may have already elapsed. This
raises the question of whether a one-size-fits-all bystander CPR with no
breathing component is advisable. It is not surprising that the rates of
survival with good neurological outcomes are low. Until recently, the Hong
Kong emergency medical services did not provide over-the-phone
instructions on bystander CPR, thus precluding the incorporation of a
breathing component (even when ventilation is clearly necessary) prior to
the arrival of trained personnel. Since last year, however, Hong Kong has
established a dispatcher instruction hotline which should hopefully allow
improved guidance for untrained bystanders to provide better quality CPR.
There thus exists a conflict: the need to promptly
initiate chest compression that should be uninterrupted, and the need to
oxygenate that itself may delay and interrupt chest compression. By
promoting CO-CPR for untrained bystanders in OHCA, the International
Liaison Committee on Resuscitation has apparently chosen to assign a lower
priority to arrests that are unwitnessed and those of respiratory origin
without acknowledging that there are two components of rescue breathing:
airway patency and mouth-to-mouth breathing. It is only the mouth-to-mouth
breathing component that deters public participation, causes
hyperventilation, and delays and interrupts chest compression. We have
argued that the need for respiration and for prompt uninterrupted chest
compression can both be accommodated if the mouth-to-mouth breathing only
is removed, but not the airway patency component.6
The simple manoeuvre that healthcare personnel
routinely use to open the airway of a comatose patient is the chin lift,
with or without insertion of an oropharyngeal airway. The chin lift
elevates the hyoid bone and in turn the epiglottis by means of the
hyoid-epiglottic ligament. It also prevents the tongue from being sucked
into the path of airflow during inhalation. Both chin lift and the
oropharyngeal airway are extremely effective. With a patent airway,
gasping, which is associated with improved survival,7 and passive ventilation from chest compression8 9 are
facilitated. Passive ventilation via an orotracheal tube during CPR has
been shown to be superior to CPR with bag-mask ventilation.10 When airway patency is maintained using chin lift or
an oropharyngeal airway, passive ventilation should theoretically have a
similar beneficial effect. Chin lift is feasible when there is a second
bystander. For single-bystander CPR, a less reliable technique is to turn
the patient’s head as far as possible to one side before promptly
commencing uninterrupted CPR. In anaesthetised or deeply sedated patients
with obstructive sleep apnoea, the head turn may reduce airway
obstruction.11 12 The Figure illustrates the effectiveness of chin lift
and head turn in maintaining airway patency in a healthy deeply sedated
patient. From experience, a head turn is less consistent or efficient in
opening the airway but given its simplicity, should be performed
immediately prior to the commencement of uninterrupted CO-CPR by a single
bystander.
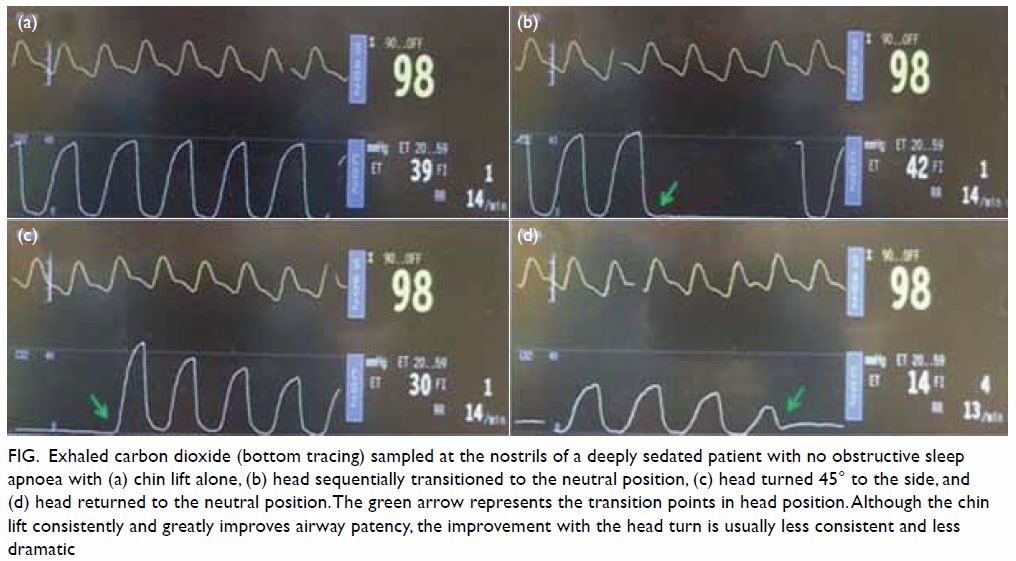
Figure. Exhaled carbon dioxide (bottom tracing) sampled at the nostrils of a deeply sedated patient with no obstructive sleep apnoea with (a) chin lift alone, (b) head sequentially transitioned to the neutral position, (c) head turned 45° to the side, and (d) head returned to the neutral position. The green arrow represents the transition points in head position. Although the chin lift consistently and greatly improves airway patency, the improvement with the head turn is usually less consistent and less dramatic
Strategies for increasing OHCA survival include
widespread deployment of AEDs in public places and education campaigns. It
has been recently proposed that oropharyngeal airways across the age
spectrum be included in public AED boxes.13
An instruction sheet with illustrations on how to size an oropharyngeal
airway should be included for quick reference. The airway can be inserted
by a second bystander while the primary rescuer is applying the
defibrillator pads or performing CO-CPR. If only one bystander is present,
the oropharyngeal airway can be inserted immediately prior to commencing
uninterrupted CO-CPR. Because more than half of adult OHCAs in Hong Kong
occur in the home,1 the government
should consider providing one size 9 (9 cm, yellow) and one size 8 (8 cm,
green) oropharyngeal airways for all households and dwellings with a
resident who is an elderly person or has cardiac problems; these two
airway sizes are suitable for almost all men and women, respectively.14 Consideration should also be given to providing
paediatric oropharyngeal airways for households with a seriously ill
child, who comprise a significant proportion of paediatric OHCAs in Hong
Kong.4
Out-of-hospital cardiac arrest is a serious public
health problem worldwide. Despite great effort and expense (eg,
therapeutic hypothermia15),
improvements in meaningful survival after cardiac arrest have been only
marginal. The steps and strategies we have suggested may have a large
impact at extremely low cost. Hong Kong should take a lead in exploring
ways to improve OHCA outcomes by incorporating airway patency and passive
ventilation in the untrained bystander CPR protocol, running public
education and training campaigns, and conducting observational (eg,
before-after) and randomised controlled studies to validate the concept.
Author contributions
All authors had full access to the data,
contributed to the study, approved the final version for publication, and
take responsibility for its accuracy and integrity.
Concept and design of study: AMH Ho, GB Mizubuti.
Acquisition of data: AMH Ho, GB Mizubuti, D Sydor.
Analysis or interpretation of data: AMH Ho, GB Mizubuti.
Drafting of the manuscript: AMH Ho, GB Mizubuti, AK Ho.
Critical revision for important intellectual content: D Sydor, S Wan, DC Chung.
Acquisition of data: AMH Ho, GB Mizubuti, D Sydor.
Analysis or interpretation of data: AMH Ho, GB Mizubuti.
Drafting of the manuscript: AMH Ho, GB Mizubuti, AK Ho.
Critical revision for important intellectual content: D Sydor, S Wan, DC Chung.
Conflicts of interest
All authors have disclosed no conflicts of
interest.
Funding/support
This research received no specific grant from any
funding agency in the public, commercial, or not-for-profit sectors.
References
1. Fan KL, Leung LP, Siu YC.
Out-of-hospital cardiac arrest in Hong Kong: a territory-wide study. Hong
Kong Med J 2017;23:48-53. Crossref
2. Chan PS, Krumholz HM, Nichol G,
Nallamothu BK; American Heart Assocation National Registry of
Cardiopulmonary Resuscitation Investigators. Delayed time to
defibrillation after in-hospital cardiac arrest. N Engl J Med
2008;358:9-17. Crossref
3. Weisfeldt ML, Sitlani CM, Ornato JP, et
al. Survival after application of automatic external defibrillators before
arrival of the emergency medical system: evaluation in the resuscitation
outcomes consortium population of 21 million. J Am Coll Cardiol
2010;55:1713-20. Crossref
4. Law AK, Ng MH, Hon KL, Graham CA.
Out-of-hospital cardiac arrest in the pediatric population in Hong Kong: a
10-year review at a university hospital. Pediatr Emerg Care
2018;34:179-84.
5. Brouwer TF, Walker RG, Chapman FW,
Koster RW. Association between chest compression interruptions and
clinical outcomes of ventricular fibrillation out-of-hospital cardiac
arrest. Circulation 2015;132:1030-7. Crossref
6. Ho AM, Mizubuti GB, Wan S. Improving the
success rate of chest compression-only CPR by untrained bystanders in
adult out-of-hospital cardiac arrest: maintaining airway patency may be
the way forward. Anesth Analg 2018;126:351-3. Crossref
7. Debaty G, Labarere J, Frascone RJ, et
al. Long-term prognostic value of gasping during out-of-hospital cardiac
arrest. J Am Coll Cardiol 2017;70:1467-76. Crossref
8. Safar P, Brown TC, Holtey WJ. Failure of
closed chest cardiac massage to produce pulmonary ventilation. Dis Chest
1962;41:1-8. Crossref
9. Deakin CD, O’Neill JF, Tabor T. Does
compression-only cardiopulmonary resuscitation generate adequate passive
ventilation during cardiac arrest? Resuscitation 2007;75:53-9. Crossref
10. Bobrow BJ, Ewy GA, Clark L, et al.
Passive oxygen insufflation is superior to bag-valve-mask ventilation for
witnessed ventricular fibrillation out-of-hospital cardiac arrest. Ann
Emerg Med 2009;54:656-62. Crossref
11. Safiruddin F, Koutsourelakis I, de
Vries N. Upper airway collapse during drug induced sleep endoscopy: head
rotation in supine position compared with lateral head and trunk position.
Eur Arch Otorhinolaryngol 2015;272:485-8. Crossref
12. Walsh JH, Maddison KJ, Platt PR,
Hillman DR, Eastwood PR. Influence of head extension, flexion, and
rotation on collapsibility of the passive upper airway. Sleep
2008;31:1440-7.
13. Ho AK. Should oropharyngeal airways be
included with public automatic external defibrillators? Circulation
2018;138:1620-2. Crossref
14. Kim HJ, Kim SH, Min JY, Park WK.
Determination of the appropriate oropharyngeal airway size in adults:
Assessment using ventilation and an endoscopic view. Am J Emerg Med
2017;35:1430-4. Crossref
15. Moler FW, Silverstein FS, Holubkov R,
et al. Therapeutic hypothermia after in-hospital cardiac arrest in
children. N Engl J Med 2017;376:318-29. Crossref

