© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
CASE REPORT
Multifocal mucosa–associated lymphoid tissue lymphoma
involving the lungs and the stomach: a rare clinical entity: a case report
Carla PM Lam, MB, BS1; CF Wong, FHKCP,
FRCP (Edin)2
1 Department of Medicine, Queen Mary
Hospital, Pokfulam, Hong Kong
2 Tuberculosis and Chest Medicine Unit,
Grantham Hospital, Wong Chuk Hang, Hong Kong
Corresponding author: Dr CF Wong (meicarlalam@gmail.com)
Case report
A 77-year-old male ex-smoker initially presented to
Queen Mary Hospital, Hong Kong in April 2009 with an abnormal lung lesion
at the left lower lobe on computed tomography (CT) scan of the abdomen
during workup for abdominal aorta aneurysm (Fig 1). The lung lesion persisted despite antibiotic
treatment. Flexible bronchoscopy, bronchial brushings and aspirate were
unremarkable. It was decided to keep the patient under observation.
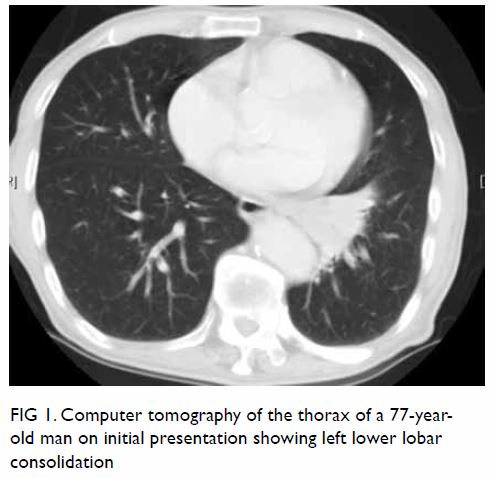
Figure 1. Computer tomography of the thorax of a 77-year-old man on initial presentation showing left lower lobar consolidation
One year later he developed per-rectal bleeding.
Colonoscopy was unremarkable but upper endoscopy revealed a 5-cm
ulcerative growth in the posterior wall of the proximal gastric body.
Histology showed sheets of small abnormal lymphoid cells with pale
cytoplasm and cleaved nuclear outline, strongly positive for CD20 and
CD79a, and negative for CD3, CD5, CD23, CD10, CD43, and Cyclin-D1. There
was lambda light chain restriction. The Ki-67 proliferation index was less
than 10%. Lymphoepithelial lesions were identified. Helicobacter pylori
was not detected and the patient was treated as a case of isolated primary
H pylori–negative gastric mucosa-associated lymphoid tissue (MALT)
lymphoma with H pylori eradication followed by rituximab for eight
cycles. The response was suboptimal and he was subsequently prescribed
three cycles of rituximab, cyclophosphamide, vincristine, and
prednisolone.
He was admitted to our chest unit in July 2017 for
treatment of chest infection. Review of serial chest X-ray and CT scans
showed progressive deterioration of the lung lesion that had extended to
the whole left lower lobe with consolidative changes, air bronchogram,
multiple cystic changes and bronchial dilatation (Fig 2). Serial positron emission tomography–CT scans
showed that the lung lesion was metabolically active with partial
improvement upon chemotherapy correlating with that of the gastric MALT
lymphoma. Repeat fibre-optic bronchoscopy and transbronchial lung biopsy
revealed respiratory mucosa with diffuse dense lymphoid proliferation in
the stroma. Lymphoepithelial lesions were again observed, positive for
CD20 and negative for CD3, CD5, CD10, CD23, and Cyclin-D1. Lambda light
chain restriction was demonstrated, compatible with MALT lymphoma.
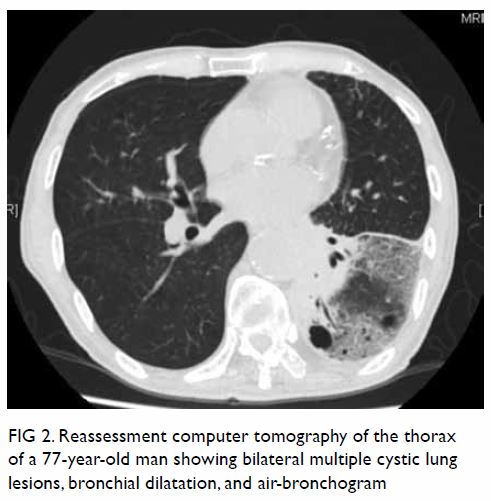
Figure 2. Reassessment computer tomography of the thorax of a 77-year-old man showing bilateral multiple cystic lung lesions, bronchial dilatation, and air-bronchogram
Discussion
Mucosa-associated lymphoid tissue lymphoma is a
relatively rare disease with an annual incidence estimated at 1/313 000;
MALT lymphoma accounts for 6% to 8% of all non-Hodgkin lymphomas.
Histologically, MALT lymphoma is characterised by neoplastic cell
infiltration around reactive secondary lymphoid follicles in a marginal
zone distribution and centrocyte-like cells that are small-to-medium in
size with small irregular nuclei. Neoplastic cells frequently have
abundant pale cytoplasm and a distinct cell border, resembling small
mature lymphocytes. Lymphoepithelial lesions have been frequently
described. The immunophenotype of MALT lymphoma is virtually identical to
that of non-neoplastic marginal-zone B cells. They are positive for CD20
but negative for IgD, CD5, CD10, Bcl6, and Cyclin-D1. Demonstration of
immunoglobulin light chain restriction is also helpful to exclude reactive
lymphoid infiltrate. No specific immunohistochemical marker has been
identified for MALT lymphoma with different tissues of origin.1
The most common site of involvement of MALT
lymphoma is the stomach, accounting for half of all cases. Other sites
include the small intestine (20%-30%), colon (10%), salivary glands,
thyroid, lung, bladder, and skin. Gastric MALT lymphoma is strongly
associated with H pylori that has been implicated in its
pathogenesis. The majority (92%-98.3%) of gastric MALT lymphomas are
positive for H pylori, and H pylori eradication alone
achieves complete remission of gastric MALT lymphoma in 80% of cases.
Pulmonary MALT lymphoma is a very rare condition,
accounting for aproximately 1% of cases. Pulmonary MALT lymphoma is
usually an indolent disease and has no association with H pylori
but is associated with chronic inflammatory conditions instead.
Radiological features of pulmonary MALT lymphoma are diverse and include
air bronchogram, bronchial dilation, nodular lesions, lung mass,
ground-glass opacities, and cystic lung lesions. Lesions are likely
multiple, bilateral without lobar predilection with maximum standardised
uptake value varying from 2.8 to 9.4.2
Although MALT lymphoma was once thought to be an
indolent disease due to its tendency to remain localised for a prolonged
period to the tissue of origin, multifocal involvement of MALT lymphoma at
presentation has been increasingly reported in recent years.3 4 In a case
series of 304 patients with MALT lymphoma in Japan,3 seven (2%) had multifocal involvement, mostly involving
the gastrointestinal tract. In another case series in Austria involving 72
patients with non-gastric MALT lymphoma, 23 (32%) had multifocal disease
either on presentation or during the study period. Site-specific
involvement was reported. The stomach was involved at staging upper
endoscopy and histologically confirmed (P<0.0001) in seven of 13
patients with primary lung MALT lymphoma.4
There are no specific histological or
immunostaining characteristics for MALT lymphoma at different sites.
Sequence analysis of immunoglobulin heavy chain gene (IgH) may help
demonstrate multifocality of MALT lymphoma. In a study that recruited 170
patients with MALT lymphoma over 8 years, 11 had multifocal involvement
and paired tumour biopsy samples were analysed in four.5 Monoclonal rearrangement of the IgH gene was detected
in all four tumour pairs of which three had different VDJ sequences,
indicating that there was no clonal relationship between the tumour pairs
whereas the fourth demonstrated clonal identity. That study implied that
MALT lymphomas involving different organ systems more often represent
different clones and arise independently instead of disseminating from one
system to another.5
In our case, we believe that the MALT lymphoma was
multifocal in origin and the pulmonary lesion preceded that of the stomach
based on the temporal sequence (appearance of lung lesion long before
clinical manifestation of gastric MALT lymphoma). Further analysis of the
VDJ sequence of the IgH of the tumour samples is needed to demonstrate the
clonal relationship between them.
Conclusion
Mucosa-associated lymphoid tissue lymphoma was once
thought to be an indolent disease localised to one tissue origin, but
occurrence of multifocal disease has been increasingly reported. Our case
illustrates multifocal MALT lymphoma involving the lungs and the stomach
with classic histology, radiological features, and clinical behaviour.
Author contributions
All authors had full access to the data,
contributed to the study, approved the final version for publication, and
take responsibility for its accuracy and integrity.
Concept or design: All authors.
Acquistition of data: CPM Lam.
Analysis or interpretation of data: CPM Lam.
Drafting of the manuscript: CPM Lam.
Critical revision for important intellectual content: All authors.
Acquistition of data: CPM Lam.
Analysis or interpretation of data: CPM Lam.
Drafting of the manuscript: CPM Lam.
Critical revision for important intellectual content: All authors.
Conflicts of interest
The authors have disclosed no conflict of interest.
Funding/support
This research received no specific grant from any
funding agency in the public, commercial, or not-for-profit sectors.
Ethics approval
This study was conducted in accordance with the
principles outlined in the Declaration of Helsinki. The patient provided
verbal informed consent.
References
1. Bacon CM, Du MQ, Dogan A.
Mucosa-associated lymphoid tissue (MALT) lymphoma: a practical guide for
pathologists. J Clin Pathol 2007;60:361-72. Crossref
2. Zhang WD, Guan YB, Li CX, Huang XB,
Zhang FJ. Pulmonary mucosa-associated lymphoid tissue lymphoma: computed
tomography and 18F fluorodeoxyglucose-positron emission
tomography/computed imaging findings and follow-up. J Comput Assist Tomogr
2011;35:608-13. Crossref
3. Yoshino T, Ichimura K, Mannami T, et al.
Multiple organ mucosa-associated lymphoid tissue lymphomas often involve
the intestine. Cancer 2001;91:346-53. Crossref
4. de Boer JP, Hiddink RF, Raderer M, et
al. Dissemination patterns in non-gastric MALT lymphoma. Haematologica
2008;93:201-6. Crossref
5. Konoplev S, Lin P, Qiu X, Medeiros LJ,
Yin CC. Clonal relationship of extranodal marginal zone lymphomas of
mucosa-associated lymphoid tissue involving different sites. Am J Clin
Pathol 2010;134:112-8. Crossref

