© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
MEDICAL PRACTICE
Secondary prevention of fragility fractures:
instrumental role of a fracture liaison service to tackle the risk of
imminent fracture
Ronald MY Wong, MB, ChB, PhD1; SW Law,
MB, ChB, FHKAM (Orthopaedic Surgery)2; KB Lee, FRCSEd (Ortho),
FHKAM (Orthopaedic Surgery)3; Simon KH Chow, PhD1;
WH Cheung, PhD1
1 Department of Orthopaedics and
Traumatology, The Chinese University of Hong Kong, Shatin, Hong Kong
2 Department of Orthopaedics and
Traumatology, Prince of Wales Hospital, Shatin, Hong Kong
3 Department of Orthopaedics and
Traumatology, Queen Elizabeth Hospital, Jordan, Hong Kong
Corresponding author: Prof Simon KH Chow (skhchow@ort.cuhk.edu.hk)
Abstract
The occurrence of fragility fractures is strongly
associated with significant morbidity and mortality. Effective
recommendations should be set to treat these patients punctually for
secondary prevention of fractures and ultimately decrease healthcare
costs. The key pitfalls in the current management for patients with
fragility fractures are the lack of fracture liaison services, low
prescription rates for osteoporosis, inadequate referral for
rehabilitation, and low follow-up attendance leading to poor compliance
with treatment. Most imminent fractures occur within the first 2 years,
and it is therefore important to raise the awareness of fracture risk
and provide fracture liaison services to improve management. Fracture
liaison services are coordinated and have been shown to be
cost-effective. These services allow prompt identification of patients
with fragility fractures. This leads to appropriate investigations of
their bone health and fall risk. Information about and interventions for
each patient are provided for secondary prevention of fractures.
Implementation of the fracture liaison services model would play a major
role in improving patient outcomes in our community.
Introduction
Osteoporosis is a socio-economic threat, and with
the ageing population, the disease has grown into a global epidemic. The
lifetime fracture risk in patients with osteoporosis can reach 40%, and
the most common fracture regions are the hip, distal radius, and spine.1 In Hong Kong, the number of
fragility fractures is on the rise, and hospital budgets are increasing.
Currently, around 6000 hip fractures occur annually in Hong Kong, and
these numbers are projected to double by 2050.2
A recent study showed that the number of hip fractures in Asia will
increase from 1 124 060 in 2018 to 2 563 488 in 2050, a 2.28-fold
increase.3 It is also expected that
50% of hip fractures will occur in Asia, with the majority in China.4
According to the Osteoporosis Society of Hong Kong,
95% of direct costs of osteoporosis are incurred for acute management and
rehabilitation of the fracture.5
Annual hospital expenditures for hip fractures in Hong Kong amount to
approximately US$52 million and rising.6
The occurrence of fragility fractures is strongly
associated with significant morbidity and mortality. Mortality after a hip
fracture is around 5% to 10% after 1 month, and one-third of patients die
by 1 year.7 At least 10% of
patients have care issues, and most have residual disability and pain.
Many studies have also shown that mortality after vertebral compression
fractures is almost as high as that after hip fractures.8 More importantly, after the occurrence of the first
fracture, prompt measures and initiatives should be taken for secondary
prevention to decrease healthcare costs.
The single most predictive factor of a fragility
fracture is the presence of a previous fracture. The relative risk is
approximately 2-fold higher to sustain a hip or vertebral fracture after a
prior fragility fracture. The risk of vertebral fracture is 4-fold higher
for patients with prior vertebral fractures than for those without.9 The increased relative risk is not constant with time
or age, as imminent fractures occur shortly after the initial one.10 A previous large-scale prospective cohort study in
Australia showed that absolute repeat fracture risk persists up to 10
years and that 40% to 60% of surviving patients experience a subsequent
fracture. However, 41% of refractures in women and 52% of refractures in
men occur within the first 2 years.11
Effective recommendations should be made to treat these patients
punctually for secondary prevention of fractures and ultimately decrease
healthcare costs in Hong Kong.
This guideline serves to provide recommendations
about identifying patients with risk of imminent fracture. Prompt
management with the incorporation of fracture liaison services (FLS) based
on a review of the current literature is provided.
Pitfalls in Hong Kong’s current fragility fracture
management
The PubMed database (date last accessed: 28 October
2018) was searched. The keywords used for the search criteria were
“fragility fracture” and “Hong Kong” and “manage*”. Seven studies were
retrieved in the initial search. From these results, four studies related
to the management of fragility fractures in Hong Kong were included.12 13 14 15 The
remaining studies were unrelated and excluded. The key pitfalls in the
current management of patients with fragility fractures in Hong Kong are
the lack of FLS (10%-25% in public hospitals), low prescription rates for
osteoporosis on discharge (23% of hip fracture cases), inadequate referral
rates for rehabilitation (22% of hip fracture cases), and low follow-up
attendance (35.1% of hip fracture cases at 1 year). It is therefore
important to raise awareness about imminent fractures and FLS to further
improve the current management situation.
Currently, there is a large treatment gap between
osteoporotic fractures and secondary prevention. According to the
International Osteoporosis Foundation (IOF), only 10% to 25% of public
hospitals in Hong Kong have FLS.6
Furthermore, a study of six hospitals in Hong Kong located in different
clusters showed that only 23% of patients were prescribed
anti-osteoporotic medications postoperatively for hip fractures.15 Another study showed that 33% of anti-osteoporotic
medications that were prescribed were given 6 months after discharge.14 Routine preoperative orthogeriatric co-management for
hip fractures was given in only 3.5% of cases.15
A previous study had already established certain outcomes, showing a
shorter length of stay, shorter time to surgery, lower in-hospital
mortality, and lower hospital cost of US$170 224 annually with
implementation of an orthogeriatric intervention for hip fracture patients
in Hong Kong.16 Currently, there
is poor coordination among different subspecialties in delivery of
post-fragility fracture care. There is also low follow-up attendance after
discharge: 74.8% at 3 months and 35.1% at 1 year.15
Internal surveys showed only 22% of patients are referred for
rehabilitation, with inadequate fall prevention programmes provided.
As the number of patients with osteoporosis
continues to grow, regular follow-up is crucial, as long-term monitoring
for chronic disease is required. Currently, fewer than five public
hospitals have dedicated osteoporosis clinics for care of these patients.
More importantly, many patients are seen at various subspecialty clinics,
including general medicine, orthopaedics, endocrinology, and geriatrics,
causing the standard of care to be suboptimal.
There are currently seven dual-energy X-ray
absorptiometry (DXA) scanning facilities in the public setting in Hong
Kong. The average waiting time for a DXA scan is 1 to 6 years, depending
on location. The long waiting time places the patient at high risk of
imminent fractures occurring within 2 years of the initial fracture.
According to the Asian Federation of Osteoporosis
Societies Call-To-Action Committee, osteoporosis should be made a national
health priority.17 It is also
important to raise public awareness, have educational programmes for
health professionals, and ultimately prevent secondary fractures. The
current evidence suggests that a structured service delivery model (ie, an
FLS) is therefore essential to improve the care of our patients. There is
certainly a pressing need for further resource allocation to the
prevention of secondary fractures to decrease healthcare costs, patient
morbidity, and mortality.
Preventing imminent fractures
Imminent fractures, or fractures occurring within 2
years of the initial fracture, should be identified promptly to receive
anti-osteoporotic treatment and fall prevention programmes.10 18 Prompt
multidisciplinary assessment should be employed, and patients should
undergo thorough evaluation to prevent imminent fractures. It is well
documented that the cause of imminent fractures may be the increase of
frailty during hospital admission.18
Immobility due to pain and disability causes an increased loss of cortical
and trabecular bone.
The Reykjavik Study fracture registrar from Iceland
showed that the risk of a major osteoporotic fracture after a previous one
was 2.7-fold higher compared with the general population risk at 1 year,
and this risk elevation decreases to 1.4-fold at 10 years.10 The risk of a second major osteoporotic fracture also
increases by 4% for each year of age. As the absolute risk is 6.1% for
subsequent fractures at 1 year, the implementation of global fracture
prevention strategies to prevent imminent fractures is crucial.10 The concept of a recent fracture as a more predictive
risk factor than fracture history is important for future health policies.10 19
Therefore, the window of opportunity to treat imminent fractures is best
taken advantage of by FLS, as it provides a holistic approach and treats
osteoporosis from a public health perspective.20
Importance and cost-effectiveness of fracture liaison
services for patients with fragility fractures
Fracture liaison services are coordinated services
that identify patients with fragility fractures, assess and treat their
bone health, make referrals for rehabilitation, and aim to prevent
secondary fractures.21
Most patients do not receive appropriate bone
health assessment and treatment. In fact, only 9% to 50% of patients in
the US, the UK, and Canada proceed with these assessments after a
fragility fracture.21
International FLS guidelines in the US including initiatives by specialty
groups, such as the American Orthopedics Association “Own the Bone”
campaign, have been established to target these patients during the
imminent fracture time interval.22
In a US nationwide study of 273 330 patients with index fractures,
imminent fractures were common in the 1 year following hip, shoulder or
wrist fractures. Therefore, national strategies to minimise further
impairment have been urged, as subsequent fractures cause significant
morbidity and loss of quality of life. However, many hospitals worldwide
still lack this model of care.23 24
A recent meta-analysis of 74 controlled studies
showed that FLS programmes improved outcomes, with significant increases
in bone mineral density assessment (48.0% vs 23.5%), treatment initiation
(38.0% vs 17.2%) and adherence (57.0% vs 34.1%), and reductions in
re-fracture incidence (6.4% vs 13.4%) and mortality (10.4% vs 15.8%).25 In Taiwan, 22 FLS programmes have already been
established, of which 11 are accredited by the IOF.26 Taiwan has some of the best FLS coverage in the
Asia-Pacific region. Randomised controlled trials are being conducted to
assess outcomes in Taiwan.26 Other
countries that have adopted FLS programmes include Japan, where it has
been proven to be cost-effective. A recent study in Japan showed an
additional lifetime cost of US$3396 per person for an additional 0.118
quality-adjusted life year (QALY), resulting in an incremental
cost-effectiveness ratio of US$28 880 per QALY gained.27 Furthermore, a systematic review has also shown that
FLS per the IOF Best Practice Standards conducted in Canada, Australia,
the US, the UK, Japan, and Sweden were all found to be cost-effective in
comparison with usual or no treatment, regardless of programme intensity
or country.24 The costs per QALY
ranged from US$3023 to US$28 800 in Japan and from US$14 513 to US$112 877
in the US. Several studies have also shown that FLS was cost-saving, which
further reinforces that these services should be widely adopted and
introduced.24 Fracture liaison
services could effectively bridge the gap between the patient and
prevention of imminent fractures.
Creating a model for fracture liaison services in Hong
Kong
There are several published models to create an
effective model of FLS care. Many hospitals have adopted the
recommendations of the IOF Capture the Fracture Campaign, which consist of
13 Best Practice Standards.28 The
recent FLS consensus meeting in the Asia-Pacific Region endorsed by the
IOF, the Asian Federation of Osteoporosis Societies, and the Asia Pacific
Osteoporosis Foundation reinforced that there is still a wide gap in terms
of fragility fractures and secondary prevention.12
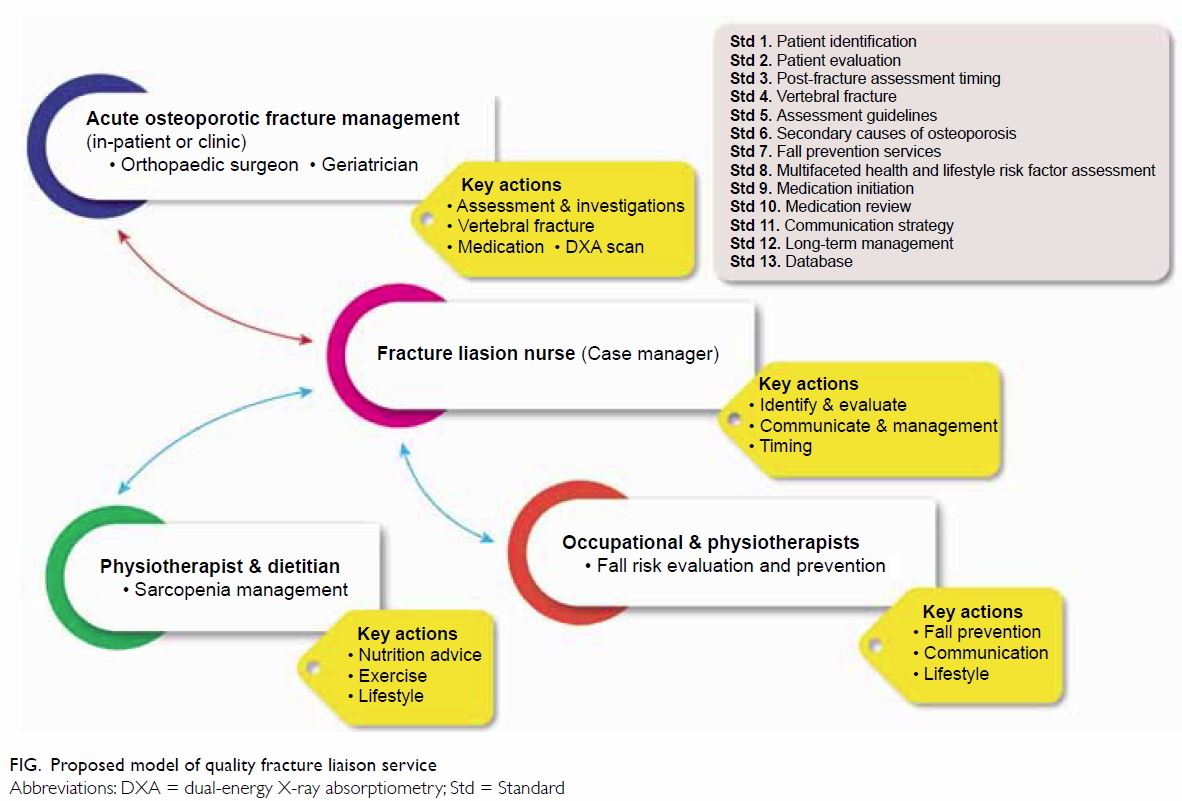
Therefore, it is essential to establish FLS in Hong
Kong (Fig). One essential element is a dedicated
coordinator, often a nurse,29 who
provides proactive recruitment of patients aged ≥50 years with new
fragility fractures or vertebral fractures. All patients should be
evaluated for future fracture risk within 3 months. In addition to DXA
scanning, the cause of osteoporosis should also be recognised, and blood
tests including serum calcium, phosphate, creatinine, and
25-hydroxyvitamin D should be performed to look for secondary
osteoporosis. All patients with osteoporosis should be treated promptly
with anti-osteoporotic medications and reviewed regularly during
follow-up. Fall risk and health and lifestyle risk factors should be
evaluated accordingly. A dedicated database with long-term management
should be established for these patients.
The implementation of an FLS model would play a
major role in improving patient outcomes to prevent imminent fractures. It
is important to have policymaker and stakeholder engagement to achieve
successful and widespread uptake of FLS in our community.
Anti-osteoporotic drug use and challenges in decreasing
imminent fractures
In Hong Kong, only 23% of hip patients discharged
are prescribed with anti-osteoporotic medications, excluding calcium and
vitamin D supplements.15 An FLS
model would be important to coordinate and improve on osteoporosis
medication initiation and adherence and improve follow-up.30 Bisphosphonates are most commonly prescribed and are
currently considered first-line drugs for treatment of osteoporosis.5 The Agency for Healthcare Research and Quality
published a systematic review showing alendronate, risedronate, zoledronic
acid, denosumab and teriparatide to be effective at reducing fractures.31 This further shows the
importance of early treatment to prevent imminent fractures. A
meta-analysis of 10 studies of five anti-osteoporotic agents (risedronate,
alendronate, strontium ranelate, zoledronic acid, and denosumab) also
showed an 11% reduction in mortality with treatment for established
fragility fractures. Mortality reduction was highest in patients who were
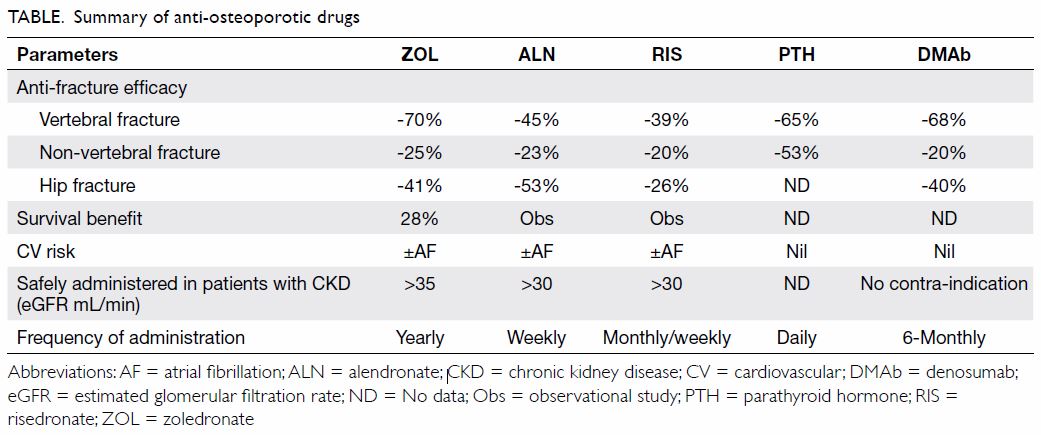
frail and older.32 The Table
summarises a selection of anti-osteoporotic drugs.
Currently, the prescription of combination
treatment has a low quality of evidence, except for the addition of
teriparatide to on-going denosumab, which produces a large increase in
bone mineral density compared with monotherapy.33
The use of bisphosphonates following teriparatide has been shown to
produce an additional bone mineral density increase in both the hip and
spine.33 34 Sequential anabolic drugs followed by
anti-remodelling agents may therefore become the standard to treat
imminent fractures in the future.35
However, poor compliance with bisphosphonates is a
major issue worldwide.18
Additional measures to tackle this problem are essential to ensure
successful patient care during the period of imminent fractures.
Improving compliance with bisphosphonates
A systematic review has shown that 50% of all
patients prescribed oral bisphosphonates stop treatment within 1 year.18 36 Although
patients receiving weekly instead of daily oral bisphosphonates had higher
compliance at 1 year, the overall treatment rate was still below the
required standard for optimal fracture prevention.37 A meta-analysis of 15 articles describing 171 063
patients revealed a 46% increase of fracture risk in non-compliant
patients compared with compliant patients.38
Adherence to bisphosphonates has become a major problem leading to
subsequent fractures, morbidity, and mortality.
International guidelines to improve adherence have
been recommended. A systematic review showed that periodic follow-up
interaction between patients and health professionals improved adherence
and persistence.39 A review of 20
studies showed the importance of simplification of the dosing regimen.40 The Denosumab Adherence Preference Satisfaction
study, a 24-month randomised, crossover comparison with alendronate in
postmenopausal women, showed less frequent non-adherence with denosumab,
which was injected every 6 months.41
Of the 250 women who enrolled, at 1 year and 2 years, 88.1% and 92.5%
adhered to denosumab, whereas only 76.6% and 63.5% adhered to alendronate,
respectively. Furthermore, of the 198 subjects who expressed treatment
preference, 92.4% favoured injections over oral therapy.41 A US study consisting of 10 863 patients with newly
initiated osteoporosis treatment showed that at 12 months of treatment,
persistence varied from 28.9% to 35.1% for oral bisphosphonate users,
59.1% for teriparatide, and 68.3% for denosumab.42
Although there has been no comparison between denosumab and zoledronic
acid, recent reviews have shown that adherence to and patient preference
for zoledronic acid were greater compared with that for oral
bisphosphonates.43 This further
reinforces that patients prefer less frequent dosing and that switching
from oral to injection therapy may improve compliance.44
Prescribing anti-osteoporotic drugs that have
higher compliance is an important consideration for clinicians, especially
during the first 2 years, when imminent fracture risk is high.
Fall prevention programmes to prevent imminent
fractures
Numerous studies have concluded that among elderly
people, fall prevention is as important as treating osteoporosis.45 It is estimated that fall prevention reduces the
number of fractures by over 50%. Fracture liaison services models have
recommended assessment of fall risk, which is essential to prevent
imminent fractures. Early referral for physiotherapy and exercise-based
intervention (including multi-component exercises with strength,
endurance, and balance training) reduces the rate and risk of falling.46 Balance training is also an important component of
fall prevention for patients with fragility fractures during
rehabilitation. Tai chi has been shown to significantly reduce fall risk
and rate.47
A recent systematic review and meta-analysis showed
that vibration therapy reduced fall rate and may prevent fractures by
reducing falls.48 Vibration
therapy provides a non-invasive, cyclic mechanical stimulation that has
been shown to improve quadriceps muscle strength, balancing, and movement
velocity.49 Incorporating the
device into multidisciplinary rehabilitation programmes for elderly
patients with hip fractures has also been shown to be effective.13 The FLS programme is able to integrate fall risk
assessments with adequate information and treatment for patients to
prevent further falls and fractures, especially during the imminent
fracture period.
Increasing awareness of sarcopenia and fragility
fractures
Sarcopenia is an age-related decline in muscle bulk
and strength, which is strongly associated with frailty.50 According to the practical definition and consensus
for age-related sarcopenia in 2010 by the European Working Group on
Sarcopenia in Older People and in 2014 by the Asian Working Group for
Sarcopenia, low muscle mass and low muscle function or low physical
performance are the criteria for diagnosis.51
52
Sarcopenia leads to falls, disability, and
increased mortality. More importantly, a recent multi-centre
cross-sectional study showed that 37% of subjects with hip fractures were
diagnosed with sarcopenia.53
Several studies have shown that osteoporosis is closely related to
sarcopenia.54 A study of 2400
Japanese women also showed sarcopenia was highly associated with
osteopenia (present in 16.8% of cases) and osteoporosis (in 20.4%).55
A local study showed that the prevalence of
sarcopenia was 73.6% in men and 67.7% in women with geriatric hip
fractures.56 This prevalence is
much higher than that in community-dwelling elderly people, and therefore,
the health status of muscle tissue should be investigated during
hospitalisation.51 A global
evaluation of nutritional status is required in addition to early
mobilisation of patients. Resistance exercises and supplements including
vitamin D should be recommended to strengthen muscle and hence reduce
falls.57 58 Studies have also shown that nutrition is important
for sarcopenia and that protein intake of 1.0 to 1.2 g/kg per day is
recommended for older adults.59
Dietary protein increases insulin-like growth factor, which has anabolic
effects on bone and muscle. Furthermore, calcium absorption is increased,
having positive effects on bone health.59
Awareness and understanding of the condition are crucial for better care
and quality of life for elderly patients.
Recommendation to establish fracture liaison services
in Hong Kong
Once an official FLS programme is established in
Hong Kong based on the 13 best practice standards, serial workshops should
be hosted to promote FLS expansion by a panel of local experts.26 Experts should be invited as clinical instructors and
coordinators to share experiences. New programmes can also share
challenges and interim progress for discussion. Furthermore, osteoporosis
treatment promotion events can be held at each participating hospital to
allow close interactions between healthcare providers and patients. After
successful implementation, accreditation by the IOF can be achieved based
on assessment of the practice guidelines.60
Conclusion
Fracture liaison service models should be adopted
in hospitals for secondary prevention of fractures, particularly imminent
fractures. Fracture liaison services can improve patient outcomes and
decrease healthcare costs. With the current lack of resources and pitfalls
in fragility fracture management in Hong Kong, major changes and
engagement with stakeholders are crucial to achieve successful and
widespread uptake of FLS to tackle the undertreatment of osteoporosis.
Author contributions
All authors had full access to the data,
contributed to the study, approved the final version for publication, and
take responsibility for its accuracy and integrity.
Concept and design of study: All authors.
Acquisition of data: RMY Wong, SKH Chow, WH Cheung.
Drafting of the manuscript: RMY Wong, SW Law, WH Cheung.
Critical revision for important intellectual content: KB Lee, SKH Chow.
Acquisition of data: RMY Wong, SKH Chow, WH Cheung.
Drafting of the manuscript: RMY Wong, SW Law, WH Cheung.
Critical revision for important intellectual content: KB Lee, SKH Chow.
Conflicts of interest
All authors have disclosed no conflicts of
interest.
Funding/support
This research received no specific grant from any
funding agency in the public, commercial, or not-for-profit sectors.
References
1. Rachner TD, Khosla S, Hofbauer LC.
Osteoporosis: now and the future. Lancet 2011;377:1276-87. Crossref
2. Lau PY. To improve the quality of life
in elderly people with fragility fractures. Hong Kong Med J 2016;22:4-5. Crossref
3. Cheung CL, Ang SB, Chadha M, et al. An
updated hip fracture projection in Asia: The Asian Federation of
Osteoporosis Societies study. Osteoporos Sarcopenia 2018;4:16-21. Crossref
4. Bow CH, Tsang SW, Loong CH, Soong CS,
Yeung SC, Kung AW. Bone mineral density enhances use of clinical risk
factors in predicting ten-year risk of osteoporotic fractures in Chinese
men: the Hong Kong Osteoporosis Study. Osteoporosis Int 2011;22:2799-807.
Crossref
5. OSHK Task Group for Formulation of 2013
OSHK Guideline for Clinical Management of Postmenopausal Osteoporosis in
Hong Kong; Ip TP, Cheung SK, Cheung TC, et al. The Osteoporosis Society of
Hong Kong (OSHK): 2013 OSHK guideline for clinical management of
postmenopausal osteoporosis in Hong Kong. Hong Kong Med J 2013;19 Suppl
2:1-40.
6. International Osteoporosis Foundation.
Asia-Pacific regional audit. Epidemiology, costs, and burden of
osteoporosis in 2013—Hong Kong. Available from:
https://www.iofbonehealth.org/sites/default/files/media/PDFs/Regional%20Audits/2013-Asia_Pacific_Audit-Hong_Kong_0_0.pdf.
Accessed 1 Jul 2018.
7. Parker M, Johansen A. Hip fracture. BMJ
2006;333:27-30. Crossref
8. Johnell O, Kanis JA, Odén A, et al.
Mortality after osteoporotic fractures. Osteoporos Int 2004;15:38-42. Crossref
9. Klotzbuecher CM, Ross PD, Landsman PB,
Abbott TA 3rd, Berger M. Patients with prior fractures have an increased
risk of future fractures: a summary of the literature and statistical
synthesis. J Bone Miner Res 2000;15:721-39. Crossref
10. Johansson H, Siggeirsdóttir K, Harvey
NC, et al. Imminent risk of fracture after fracture. Osteoporos Int
2017;28:775-80. Crossref
11. Center JR, Bliuc D, Nguyen TV, Eisman
JA. Risk of subsequent fracture after low-trauma fracture in men and
women. JAMA 2007;297:387-94. Crossref
12. Chan DD, Chang LY, Akesson KE, et al.
Consensus on best practice standards for Fracture Liaison Service in the
Asia-Pacific region. Arch Osteoporos 2018;13:59. Crossref
13. Cheung WH, Shen WY, Dai DL, et al.
Evaluation of a multidisciplinary rehabilitation programme for elderly
patients with hip fracture: a prospective cohort study. J Rehabil Med
2018;50:285-91. Crossref
14. Kung AW, Fan T, Xu L, et al. Factors
influencing diagnosis and treatment of osteoporosis after a fragility
fracture among postmenopausal women in Asian countries: a retrospective
study. BMC Womens Health 2013;13:7. Crossref
15. Leung KS, Yuen WF, Ngai WK, et al. How
well are we managing fragility hip fractures? A narrative report on the
review with the attempt to set up a Fragility Fracture Registry in Hong
Kong. Hong Kong Med 2017;23:264-71. Crossref
16. Ho WW, Dai DL, Liu KW, et al. To
investigate the effect and cost-effectiveness of implementing an
orthogeriatric intervention for elderly patients with acute hip fracture:
the experience in Hong Kong. J Am Geriatr Soc 2009;57:2153-4. Crossref
17. Yeap SS, Jaisamrarn U, Park YS,
Takeuchi Y, Xia W, AFOS Call-To-Action Committee. The Asian Federation of
Osteoporosis Societies’ call to action to improve the undertreatment of
osteoporosis in Asia. Osteoporos Sarcopenia 2017;3:161-3. Crossref
18. Roux C, Briot K. Imminent fracture
risk. Osteoporos Int 2017;28:1765-9. Crossref
19. O’Hanlon CE, Parthan A, Kruse M, et
al. A model for assessing the clinical and economic benefits of
bone-forming agents for reducing fractures in postmenopausal women at
high, near-term risk of osteoporotic fracture. Clin Ther 2017;39:1276-90.
Crossref
20. Noordin S, Allana S, Masri BA.
Establishing a hospital based fracture liaison service to prevent
secondary insufficiency fractures. Int J Surg 2018;54(Pt B):328-32. Crossref
21. Walters S, Khan T, Ong T, Sahota O.
Fracture liaison services: improving outcomes for patients with
osteoporosis. Clin Interv Aging 2017;12:117-27. Crossref
22. Bynum JP, Bell JE, Cantu RV, et al.
Second fractures among older adults in the year following hip, shoulder,
or wrist fracture. Osteoporosis Int 2016;27:2207-15. Crossref
23. Huntjens KM, van Geel TA, van den
Bergh JP, et al. Fracture liaison service: impact on subsequent
nonvertebral fracture incidence and mortality. J Bone Joint Surg Am
2014;96:e29. Crossref
24. Wu CH, Kao IJ, Hung WC, et al.
Economic impact and cost-effectiveness of fracture liaison services: a
systematic review of the literature. Osteoporos Int 2018;29:1227-42. Crossref
25. Wu CH, Tu ST, Chang YF, et al.
Fracture liaison services improve outcomes of patients with
osteoporosis-related fractures: a systematic literature review and
meta-analysis. Bone 2018;111:92-100. Crossref
26. Chang LY, Tsai KS, Peng JK, et al. The
development of Taiwan Fracture Liaison Service network. Osteoporos
Sarcopenia 2018;4:47-52. Crossref
27. Moriwaki K, Noto S. Economic
evaluation of osteoporosis liaison service for secondary fracture
prevention in postmenopausal osteoporosis patients with previous hip
fracture in Japan. Osteoporos Int 2017;28:621-32. Crossref
28. Akesson K, Marsh D, Mitchell PJ, et
al. Capture the Fracture: a Best Practice Framework and global campaign to
break the fragility fracture cycle. Osteoporos Int 2013;24:2135-52. Crossref
29. Ganda K, Puech M, Chen JS, et al.
Models of care for the secondary prevention of osteoporotic fractures: a
systematic review and meta-analysis. Osteoporos Int 2013;24:393-406. Crossref
30. Yates CJ, Chauchard MA, Liew D,
Bucknill A, Wark JD. Bridging the osteoporosis treatment gap: performance
and cost-effectiveness of a fracture liaison service. J Clin Densitom
2015;18:150-6. Crossref
31. Levis S, Theodore G. Summary of AHRQ’s
comparative effectiveness review of treatment to prevent fractures in men
and women with low bone density or osteoporosis: update of the 2007
report. J Manag Care Pharm 2012;18(4 Suppl B):S1-15. Crossref
32. Bolland MJ, Grey AB, Gamble GD, Reid
IR. Effect of osteoporosis treatment on mortality: a meta-analysis. J Clin
Endocrinol Metab 2010;95:1174-81. Crossref
33. McClung MR. Using osteoporosis
therapies in combination. Curr Osteoporos Rep 2017;15:343-52. Crossref
34. Black DM, Bilezikian JP, Ensrud KE, et
al. One year of alendronate after one year of parathyroid hormone (1-84)
for osteoporosis. N Engl J Med 2005;353:555-65. Crossref
35. Cosman F, Nieves JW, Dempster DW.
Treatment sequence matters: anabolic and antiresorptive therapy for
osteoporosis. J Bone Miner Res 2017;32:198-202. Crossref
36. Maraka S, Kennel KA. Bisphosphonates
for the prevention and treatment of osteoporosis. BMJ 2015;351:h3783. Crossref
37. Rabenda V, Mertens R, Fabri V, et al.
Adherence to bisphosphonates therapy and hip fracture risk in osteoporotic
women. Osteoporos Int 2008;19:811-8. Crossref
38. Imaz I, Zegarra P, González-Enríquez
J, Rubio B, Alcazar R, Amate JM. Poor bisphosphonate adherence for
treatment of osteoporosis increases fracture risk: systematic review and
meta-analysis. Osteoporos Int 2010;21:1943-51. Crossref
39. Gleeson T, Iversen MD, Avorn J, et al.
Interventions to improve adherence and persistence with osteoporosis
medications: a systematic literature review. Osteoporos Int
2009;20:2127-34. Crossref
40. Hiligsmann M, Salas M, Hughes DA, et
al. Interventions to improve osteoporosis medication adherence and
persistence: a systematic review and literature appraisal by the ISPOR
Medication Adherence & Persistence Special Interest Group. Osteoporos
Int 2013;24:2907-18. Crossref
41. Freemantle N, Satram-Hoang S, Tang ET,
et al. Final results of the DAPS (Denosumab Adherence Preference
Satisfaction) study: a 24-month, randomized, crossover comparison with
alendronate in postmenopausal women. Osteoporos Int 2012;23:317-26. Crossref
42. Cheng LI, Durden E, Limone B, et al.
Persistence and compliance with osteoporosis therapies among women in a
commercially insured population in the United States. J Manag Care Spec
Pharm 2015;21:824-33, 833a. Crossref
43. Lozano MJ, Sánchez-Fidalgo S.
Adherence and preference of intravenous zoledronic acid for osteoporosis
versus other bisphosphonates. Eur J Hosp Pharm 2019;26:4-9. Crossref
44. Dalle Carbonare L, Zanatta M,
Gasparetto A, Valenti MT. Safety and tolerability of zoledronic acid and
other bisphosphonates in osteoporosis management. Drug Healthc Patient Saf
2010;2:121-37. Crossref
45. Jarvinen TL, Sievänen H, Khan KM,
Heinonen A, Kannus P. Shifting the focus in fracture prevention from
osteoporosis to falls. BMJ 2008;336:124-6. Crossref
46. Vieira ER, Palmer RC, Chaves PH.
Prevention of falls in older people living in the community. BMJ
2016;353:i1419. Crossref
47. Gillespie LD, Robertson MC, Gillespie
WJ, et al. Interventions for preventing falls in older people living in
the community. Cochrane Database Syst Rev 2012;(9):CD007146. Crossref
48. Jepsen DB, Thomsen K, Hansen S,
Jørgensen NR, Masud T, Ryg J. Effect of whole-body vibration exercise in
preventing falls and fractures: a systematic review and meta-analysis. BMJ
Open 2017;7:e018342. Crossref
49. Leung KS, Li CY, Tse YK, et al.
Effects of 18-month low-magnitude high-frequency vibration on fall rate
and fracture risks in 710 community elderly—a cluster-randomized
controlled trial. Osteoporos Int 2014;25:1785-95. Crossref
50. Hong W, Cheng Q, Zhu X, et al.
Prevalence of sarcopenia and its relationship with sites of fragility
fractures in elderly Chinese men and women. PloS One 2015;10:e0138102. Crossref
51. Tarantino U, Piccirilli E, Fantini M,
Baldi J, Gasbarra E, Bei R. Sarcopenia and fragility fractures: molecular
and clinical evidence of the bone-muscle interaction. J Bone Joint Surg Am
2015;97:429-37. Crossref
52. Chen LK, Liu LK, Woo J, et al.
Sarcopenia in Asia: consensus report of the Asian Working Group for
Sarcopenia. J Am Med Dir Assoc 2014;15:95-101. Crossref
53. Steihaug OM, Gjesdal CG, Bogen B,
Kristoffersen MH, Lien G, Ranhoff AH. Sarcopenia in patients with hip
fracture: a multicenter cross-sectional study. PloS One 2017;12:e0184780.
Crossref
54. Tarantino U, Baldi J, Scimeca M, et
al. The role of sarcopenia with and without fracture. Injury 2016;47 Suppl
4:S3-10. Crossref
55. Miyakoshi N, Hongo M, Mizutani Y,
Shimada Y. Prevalence of sarcopenia in Japanese women with osteopenia and
osteoporosis. J Bone Miner Metab 2013;31:556-61. Crossref
56. Ho AW, Lee MM, Chan EW, et al.
Prevalence of pre-sarcopenia and sarcopenia in Hong Kong Chinese geriatric
patients with hip fracture and its correlation with different factors.
Hong Kong Med J 2016;22:23-9. Crossref
57. Roth SM, Ferrell RF, Hurley BF.
Strength training for the prevention and treatment of sarcopenia. J Nutr
Health Aging 2000;4:143-55.
58. Mithal A, Bonjour JP, Boonen S, et al.
Impact of nutrition on muscle mass, strength, and performance in older
adults. Osteoporos Int 2013;24:1555-66. Crossref
59. Gaffney-Stomberg E, Insogna KL,
Rodriguez NR, Kerstetter JE. Increasing dietary protein requirements in
elderly people for optimal muscle and bone health. J Am Geriatr Soc
2009;57:1073-9. Crossref
60. International Osteoporosis Foundation.
Does your fracture liaison service deserve gold-star recognition? 2014.
Available from:
https://www.iofbonehealth.org/news/does-your-fracture-liaison-service-deserve-gold-star-recognition.
Accessed 1 Jul 2018.