Hong
Kong Med J 2019 Apr;25(2):159.e1–2
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
PICTORIAL MEDICINE
Catheterised hutch diverticulum masquerading as
intraperitoneal bladder perforation
Victor SH Chan, MB, BS, FRCR (UK)1; WM
Kwok, MB, BS2; Stephen CW Cheung, MRCP, FHKAM (Radiology)1
1 Department of Radiology, Queen Mary
Hospital, Pokfulam, Hong Kong
2 Department of Accident and Emergency,
Queen Mary Hospital, Pokfulam, Hong Kong
Corresponding author: Dr Victor SH Chan (victorchansh@gmail.com)
A computed tomography (CT) scan was performed in a
64-year-old man with a history of end-stage renal failure to evaluate
recent acute-on-chronic graft failure. To conserve remnant renal function,
no intravenous contrast was administered. There was no hydronephrosis but
the balloon of the indwelling Foley catheter was seen adjacent to but
exterior to the bladder (Fig 1). No evidence of pneumoperitoneum was seen.
Free fluid was noted in the pelvis, compatible with the history of
peritoneal dialysis. The suspicion of perforated urinary bladder was
conveyed to the referring physicians, and the patient was admitted for
further evaluation. No abdominal distension, tenderness or guarding was
elicited on physical examination. Urine output via the indwelling catheter
was within normal limits. The patient was haemodynamically stable with no
leukocytosis.
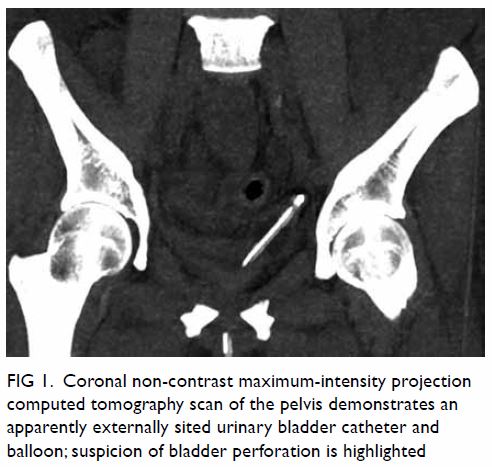
Figure 1. Coronal non-contrast maximum-intensity projection computed tomography scan of the pelvis demonstrates an apparently externally sited urinary bladder catheter and balloon; suspicion of bladder perforation is highlighted
Computed tomography cystography was performed: 20
mL of water-soluble contrast medium (Omnipaque 300) was diluted in 500 mL
of normal saline. Transurethral perfusion of 250 mL of the prepared
contrast medium was performed by free gravitational flow. Pre-instillation
and post-instillation CT cystography (5 minutes and delayed 10 minutes)
was performed. No intravenous contrast was administered.
Cross-sectional imaging revealed two large urinary
bladder diverticula sited posteriorly, close to the native vesicoureteric
junctions. The right diverticulum measured 3.8 × 4.6 cm with a 0.9-cm
neck; the left diverticulum measured 4.5 × 5.8 cm with a 1.1-cm neck. On
coronal images, a “Mickey-Mouse” appearance was noted, compatible with
bilateral hutch diverticula. The inflated balloon of the urinary catheter
was sited within the left diverticulum (Figs 2 3 4). The bladder contour was smooth. No evidence of
intraperitoneal rupture was demonstrated. On pre-cystography images, the
appearance had mimicked an externally sited catheter balloon due to the
collapsed state of the bladder.
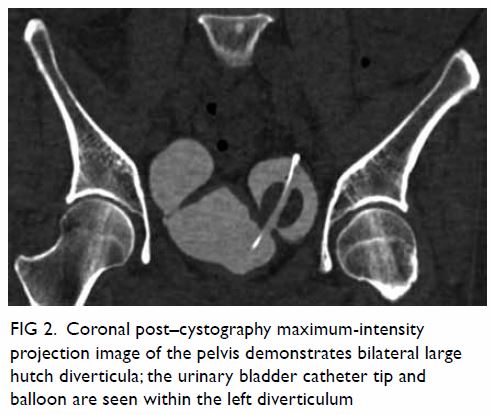
Figure 2. Coronal post–cystography maximum-intensity projection image of the pelvis demonstrates bilateral large hutch diverticula; the urinary bladder catheter tip and balloon are seen within the left diverticulum
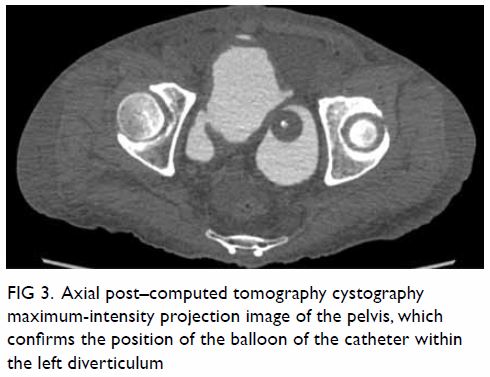
Figure 3. Axial post–computed tomography cystography maximum-intensity projection image of the pelvis, which confirms the position of the balloon of the catheter within the left diverticulum
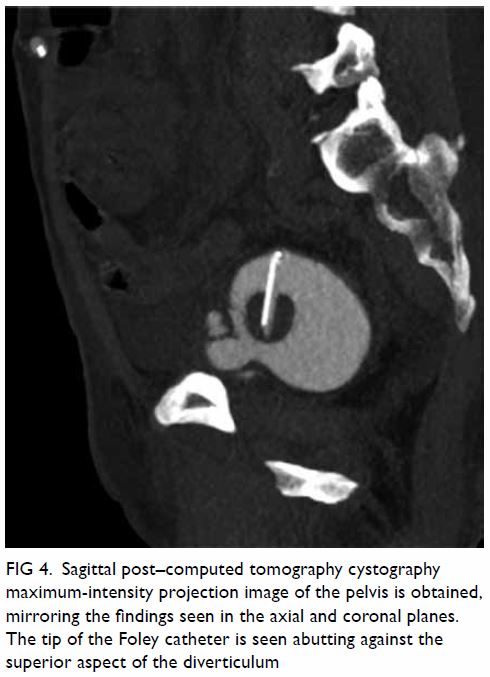
Figure 4. Sagittal post–computed tomography cystography maximum-intensity projection image of the pelvis is obtained, mirroring the findings seen in the axial and coronal planes. The tip of the Foley catheter is seen abutting against the superior aspect of the diverticulum
Spontaneous bladder perforation is rare but
potentially fatal. Most such cases present with features of peritonitis.
Some possible aetiologies include gonorrhoeal infection, radiation
therapy, diabetes mellitus, neurogenic bladder, bladder diverticula, and
indwelling urinary catheter.1 2 As our patient was largely pain-free with minimal
abdominal symptoms, the overall clinical evidence did not favour bladder
rupture even though the CT images were alarming.
Saline instillation and bedside ultrasound for
rapid disposition of polytrauma patients and early diagnosis of bladder
rupture has been described in the literature, with sensitivity reaching
90%.3 In cases with low clinical
risk for perforation and when the patient is unfit for immediate CT,
instillation of sterile saline to distend the bladder followed by
ultrasound assessment provides a possible alternative to exclude bladder
perforation. However, ultrasound results are highly operator-dependent and
this procedure should be performed only in carefully selected patients. In
experienced hands, following retrograde instillation of approximately 300
mL of sterile saline via the catheter, this imaging modality can be used
to determine presence of ascites, evaluate the distension and
configuration of the urinary bladder, look for bladder diverticula, and
determine the position of the catheter balloon. This can be performed at
the bedside for critically ill patients, involves no radiation and removes
the risk of intravenous contrast-related anaphylaxis.
Author contributions
All authors contributed to the concept, image
acquisition, image and data interpretation, manuscript drafting and
critical revision for important intellectual content. All authors had full
access to the data, contributed to the study, approved the final version
for publication, and take responsibility for its accuracy and integrity.
Conflicts of interest
The authors have no conflicts of interest to
disclose.
Funding/support
This research received no specific grant from any
funding agency in the public, commercial, or not-for-profit sectors.
Ethics approval
Relevant patient consent was obtained for the
purpose of this case study.
References
1. Sawalmeh H, Al-Ozaibi L, Hussein A,
Al-Badri F. Spontaneous rupture of the urinary bladder (SRUB); A case
report and review of literature. Int J Surg Case Rep 2015;16:116-8. Crossref
2. Ogawa S, Date T, Muraki O.
Intraperitoneal urinary bladder perforation observed in a patient with an
indwelling urethral catheter. Case Rep Urol 2013;2013:765704. Crossref
3. Karim T, Topno M. Bedside sonography to
diagnose bladder trauma in the emergency department. J Emerg Trauma Shock
2010;3;305. Crossref

