Hong
Kong Med J 2019 Apr;25(2):134–41 | Epub 10 Apr 2019
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
REVIEW ARTICLE
Rubella (German measles) revisited
Alexander KC Leung, FRCP (UK), FRCPCH1;
KL Hon, MD, FAAP2; KF Leong, MB, BS, MRCPCH3
1 Department of Pediatrics, University
of Calgary, Canada
2 Department of Paediatrics, The Chinese
University of Hong Kong, Hong Kong
3 Department of Pediatric Institute,
Kuala Lumpur General Hospital, Malaysia
Corresponding author: Prof Alexander KC Leung (aleung@ucalgary.ca)
Abstract
Rubella is generally a mild and self-limited
disease in children. During pregnancy, rubella can have
potentially devastating effects on the developing fetus. Postnatal
rubella is transmitted primarily by inhalation of virus-laden airborne
droplets or direct contact with infected nasopharyngeal secretions. In
susceptible pregnant women, the virus may cross the placenta and spread
through the vascular system of the developing fetus. Postnatally
acquired rubella typically begins with fever and lymphadenopathy,
followed by an erythematous, maculopapular rash. The rash classically
begins on the face, spreads cephalocaudally, becomes generalised within
24 hours, and disappears within 3 days. Maternal rubella, especially
during early pregnancy, may lead to miscarriage, intrauterine fetal
death, premature labour, intrauterine growth retardation, and congenital
rubella syndrome. Cataracts, congenital heart defects, and sensorineural
deafness are the classic triad of congenital rubella syndrome and they
typically occur if the fetal infection occurs in the first 11 weeks of
gestation. Laboratory confirmation of rubella virus infection can be
based on a positive serological test for rubella-specific immunoglobulin
M antibody; a four-fold or greater increase in rubella-specific
immunoglobulin G titres between acute and convalescent sera; or
detection of rubella virus RNA by reverse transcriptase-polymerase chain
reaction. Treatment is mainly symptomatic. Universal childhood
immunisation and vaccination of all susceptible patients with rubella
vaccine to decrease circulation of the virus are cornerstones to
prevention of rubella and, more importantly, congenital rubella
syndrome.
Introduction
Rubella, also called German measles, is a
communicable viral illness that typically begins with mild fever and
lymphadenopathy followed by a characteristic brief appearance of a
generalised erythematous, maculopapular rash.1
The disease was described by two German physicians, De Bergen in 1752 and
Orlow in 1758, leading to the term “German measles”.2 The term “rubella” was coined by Henry Veale, a
Scottish physician in 1866.2 The
word “rubella” is derived from the Latin word “rubellus” meaning “reddish”
or “little red”. In the absence of pregnancy, rubella is generally a mild,
self-limited, and relatively benign infection. However, maternal rubella
infection during the first trimester of pregnancy can be catastrophic and
can result in fetal death or the birth of an infant with a constellation
of congenital anomalies referred to as congenital rubella syndrome.3 This article provides an update on current knowledge
about rubella and outlines an approach to its evaluation, prevention, and
management.
A PubMed search was conducted in November 2018
using Clinical Queries with the key terms “Rubella” and “German measles”.
The search strategy included randomised controlled trials, meta-analyses,
observational studies, clinical trials, and reviews. Only papers published
in the English literature were included in this review. The information
retrieved from the above search was used in the compilation of the present
article.
Aetiology
The causative organism is the rubella virus, which
is a non-arthropod-borne member of the family Togaviridae and the sole
member of the genus Rubivirus.4
5 It is an enveloped,
single-stranded, positive sense ribonucleic acid (RNA) virus.6 The virus is easily destroyed by detergents, heat
(temperature >56°C), ultraviolet light, and extremes of pH (pH <6.8
or >8.1).4
The rubella virus is spherical, measuring 50 to 85
nm in diameter and shows pleomorphism.5
The viral genome encodes three structural proteins (C, E1, and E2) and two
non-structural proteins (p90 and p150).6
7 The nucleocapsid is composed of
the capsid protein C which surrounds the single-stranded RNA.6 8 The outer
envelope contains two glycosylated lipoproteins E1 and E2 which form
transmembrane spikes anchored to the external layer of the membrane.5 The humoral response is induced particularly by these
two glycosylated proteins which are important for the virulence of the
virus.9 The E1 protein contains
antigenic determinants that induce major immune responses.7 The protein is responsible for receptor binding,
receptor-mediated endocytosis, and induction of membrane fusion.5 6 The E2
protein forms connections between rows of E1 proteins.5 The two non-structural proteins are related to
transcription and replication which take place in the cytoplasm of the
host cells.5 6
Epidemiology
Humans are the only known reservoir for rubella
infection.7 10 Postnatal rubella is transmitted primarily by
inhalation of virus-laden airborne droplets or direct contact with
infected nasopharyngeal secretions.1
Peak infection rates tend to occur in late winter and early spring.3 4 9
Prior to the introduction of the rubella vaccine,
rubella was endemic worldwide, epidemics occurred at 6- to 9-year
intervals, and major pandemics occurred every 10 to 30 years.6 11 During the
last major pandemic from 1962 to 1965, approximately 10% of pregnant women
were infected and 30% of infants born to the infected mothers ultimately
manifested features of congenital rubella syndrome.11 In the US alone, there were at least 12.5 million
cases of clinically acquired rubella with more than 13 000 fetal or early
infant deaths, and 20 000 cases of congenital rubella syndrome during the
pandemic from 1962 to 1965.11
Since the introduction of the live attenuated rubella vaccine in 1969,
rubella has become increasingly rare in North America and many developed
countries.8 From 1969 to 1989, the
annual number of reported cases of rubella in the US decreased 99.6% and
the annual number of reported cases of congenital rubella syndrome
decreased 97.4%.11 From 1998 to
2000, 2001 to 2004, and 2005 to 2011, the median number of reported
rubella cases in the US was 272, 13, and 11 per year, respectively.10 On 29 April 2015, the Pan American Health
Organization officially declared elimination of rubella from the whole of
the American region.12 Nowadays,
rubella cases in developed countries are mainly “imported” from those
countries where rubella is endemic and occur mostly in incompletely
vaccinated or unvaccinated individuals.7
13
Globally, rubella continues to occur, with more
than 100 000 cases reported worldwide, especially in countries where
routine childhood rubella vaccination is either not available or has just
been recently introduced.14 In
2011, the World Health Organization (WHO) updated its guidance on the
preferred strategy for introduction of rubella-containing vaccine into the
national immunisation schedules and recommended a vaccination campaign,
targeting mainly children aged 9 months to 14 years.15 The number of WHO member states that include a
rubella-containing vaccine in their routine childhood immunisation
schedule has increased from 83 (43%) of 193, to 132 (68%) of 194, to 141
(72.7%) of 194, and to 152 (78.4%) of 194, in 1996, 2012, 2014, and 2016,
respectively.16 17 This is encouraging as there was a net increase of 20
countries that introduced the rubella-containing in their routine
childhood immunisation schedule from 2012 to 2016. Despite this,
intermittent rubella outbreaks continue to occur in some parts of the
world, even in countries with a national immunisation if there is a
substantial proportion of the population that are susceptible.8 18 The recent
outbreak of rubella in Japan can be primarily attributed to susceptible
men who were not included in the initial rubella immunisation schedule as
the initial immunisation strategy provided rubella vaccine only to
adolescent girls.5 8 In 2018, there were 2186 cases of rubella in Japan as
of 29 November with more than 70% of cases reported in Tokyo and its
surrounding prefectures. This is a significant increase from 1103 cases of
rubella reported on 7 October 2018.19
As of 22 October 2018, the Centre for Health Protection of the Department
of Health in Hong Kong recorded only six local cases of rubella infection
in 2018 affecting two male and four female patients with age ranging from
3 to 65 years.20
In children, rubella affects both sexes equally
whereas in adults, rubella affects more women than men. In the pre-vaccine
era, rubella was most common in children aged 5 to 9 years.6 7 16 Currently, individuals aged ≥20 years account for
most reported cases.11 Risk
factors for rubella include partially vaccinated or unvaccinated
individuals, travelling to endemic areas, exposure to household members
with rubella, and immunodeficiency.21
22
Pathogenesis
Postnatally acquired rubella is transmitted mainly
via inhalation of aerosolised particles from the respiratory tract
secretions of an infected individual.8 The virus infects cells in the
upper respiratory tract of the susceptible host through receptor-mediated
endocytosis.6 23 Initial replication occurs in the nasopharyngeal
cells and lymphoid tissue of the nasopharynx and upper respiratory tract.6 8
23 Infected individuals may shed
virus from the oropharynx and are contagious before the infection becomes
clinically evident.8 Viraemia
occurs 5 to 7 days after inoculation, disseminating the virus to multiple
organs including the skin, lymph nodes, and, in a gravid patient, the
placenta.8 9 The maculopapular rash occurs 2 to 8 days after the
onset of viraemia and resolves as the humoral immune response develops and
at this stage, the viraemia is terminated.6
23
Maternal immunity, either naturally derived or
after vaccination, is generally protective against intrauterine rubella
infection.24 In a susceptible
gravid patient, after infecting the placenta, the virus may cross the
placenta, and spread through the vascular system of the developing fetus.6 14
25 Fetal damage may result from
necrosis in the epithelium of chorionic villi, direct viral damage of
infected cells by apoptosis, viral inhibition of mitosis and restricted
development of precursor cells, and cytopathic damage to endothelial cells
of blood vessels with resultant ischaemia in developing organs.14 23 24 25 Maternal
rubella infection during pregnancy does not always result in vertical
transmission of the virus to the fetus.9
The risk of fetal infection varies depending upon the time of maternal
infection.11 25 Fetal infection rates are approximately 80% in the
first trimester, 25% in the late second trimester, 35% at 27 to 30 weeks’
gestation, and close to 100% beyond 36 weeks’ gestation.10 11 24 It is important to note that although a fetus becomes
infected, fetal malformation may not necessarily develop.11 The estimated risk for fetal malformation is
approximately 90%, 33%, 11%, 24% and 0% when maternal infection occurs
before 11 weeks, at 11 to 12 weeks, at 13 to 14 weeks, at 15 to 16 weeks,
and after 20 weeks of gestation, respectively.10
24 25
This can be explained by passive transfer of maternal antibodies and by
development of fetal humoral and cell-mediated immune responses with time.23
Clinical manifestations
Postnatally acquired rubella
The incubation period for postnatally acquired
rubella is approximately 14 to 21 days (usually 16 to 18 days) after
exposure to an individual with rubella.1
Approximately 25% to 50% of patients are asymptomatic (subclinical
infection).1 4 10 24 The period of infectivity is maximal 7 days before to
7 days after onset of rash, coinciding with peak levels of rubella virus
in the respiratory tract and viraemia which facilitate transmission.1 6 24
Prodromal symptoms typically precede the rash by 1
to 5 days.6 24 The symptoms, though common in adolescents and
adults, are unusual in young children.3
6 8
The prodromal illness is characterised by low-grade fever, anorexia,
nausea, malaise, lethargy, coryza, cough, headaches, non-exudative
conjunctivitis, sore throat, myalgia, and tender lymph nodes.4 The lymphadenopathy typically involves retroauricular,
suboccipital, and posterior cervical lymph nodes which often become more
pronounced with the onset of rash (Fig 1).1 3 8
At times, the lymphadenopathy can be generalised.1
10 In approximately 20% of cases,
petechiae can be observed on the soft palate (Forchheimer spots).6 8

Figure 1. Photograph of a 2-year-old boy with rubella showing bilateral suboccipital lymph nodes and a maculopapular rash on the back. One of the lymph nodes is indicated by a white arrow
The exanthem consists of pinpoint erythematous,
maculopapules which classically begin on the face, spread caudally to the
trunk and extremities, and become generalised within 24 hours (Fig
2).24 It is not unusual for
the rash to be mildly pruritic.24
Occasionally, the rash is scarlatiniform or purpuric.7 The rash usually lasts for 3 days and fades in the same
directional pattern as it appears.3
24

Figure 2. Photograph of a 2-year-old boy with rubella showing generalised erythematous maculopapular rash on the trunk and extremities. The rash started on the face and spread cephalocaudally to the trunk and extremities
Congenital rubella syndrome
Congenital rubella syndrome may result from
maternal rubella infection during embryogenesis.14
Cataracts, congenital heart defects, and sensorineural deafness are the
classic triad of congenital rubella syndrome and they typically occur if
the fetal infection occurs in the first 11 weeks of gestation.7 25 26
Ophthalmic abnormalities including cataracts (Fig
3), pigmentary retinopathy, infantile glaucoma, cloudy cornea,
chorioretinitis, iris hypoplasia, lacrimal drainage anomalies, and
microphthalmia occur in approximately 40% of cases.4 5 7 25 26 27 28 Cataracts occur in approximately 25% of children with
congenital rubella syndrome and they are bilateral in approximately 50% of
cases.4 25
Congenital rubella syndrome is the most common cause of congenital
cataracts.13 Pigmentary
retinopathy is traditionally characterised by a salt and pepper appearance
or a mottled, blotchy, irregular pigmentation in the fundus.11 27
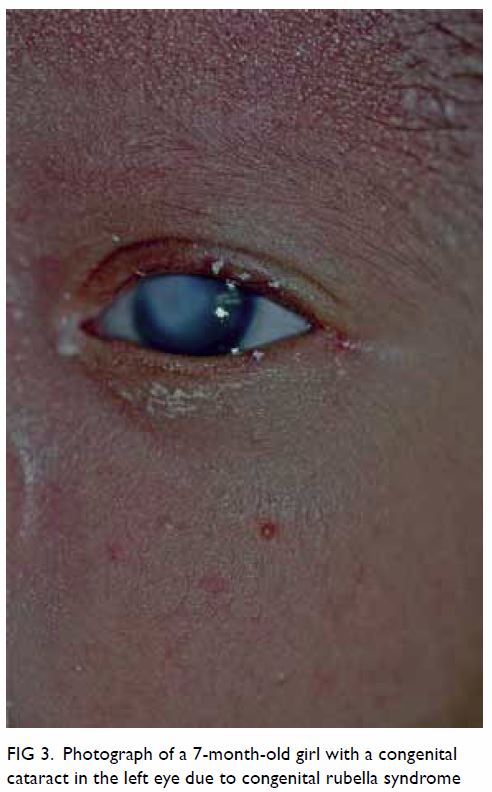
Figure 3. Photograph of a 7-month-old girl with a congenital cataract in the left eye due to congenital rubella syndrome
Patent ductus arteriosus and peripheral pulmonary
artery stenosis occur in approximately 20% and 12% of patients with
congenital rubella syndrome, respectively.25
Other cardiovascular defects such as pulmonary artery hypoplasia,
pulmonary valvular stenosis, aortic valve stenosis, coarctation of the
aorta, atrial septal defect, ventricular septal defect, and tetralogy of
Fallot have also been reported.5 14 25
Hearing impairment occurs in approximately 60% of
patients and is usually sensorineural and bilateral.7 25 At times,
hearing impairment may be the sole manifestation of congenital rubella
syndrome.29 The hearing impairment
ranges from mild to severe, may not be apparent until the second year of
life and beyond, and may progress over time.25
During the neonatal period, congenital rubella may
produce a myriad of clinical features and conditions. These include
prematurity, intrauterine growth retardation, microcephaly, haemolytic
anaemia, thrombocytopenia, purpuric rash, jaundice, hepatitis,
hepatomegaly, splenomegaly, “blueberry muffin” spots (sites of dermal
erythropoiesis, Figs 4 and 5), hypotonia, bulging anterior fontanelle,
constricted maxillary arch, high palate, interstitial pneumonia,
myocarditis, myositis, nephritis, meningoencephalitis, and striated
radiolucencies in the long bone (“celery stalk” lesions).4 7 25 30 31 32 33 34 35 Many of these features are transient and may resolve
spontaneously over days or weeks.25
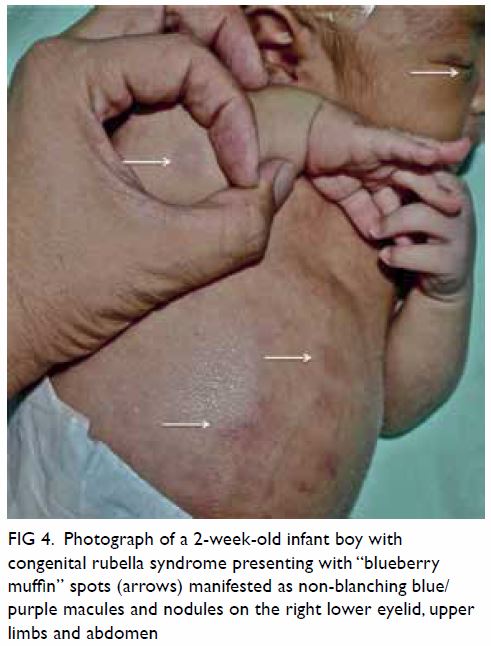
Figure 4. Photograph of a 2-week-old infant boy with congenital rubella syndrome presenting with “blueberry muffin” spots (arrows) manifested as non-blanching blue/purple macules and nodules on the right lower eyelid, upper limbs and abdomen
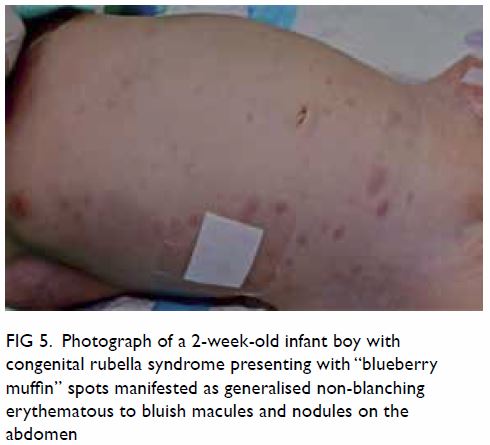
Figure 5. Photograph of a 2-week-old infant boy with congenital rubella syndrome presenting with “blueberry muffin” spots manifested as generalised non-blanching erythematous to bluish macules and nodules on the abdomen
Delayed manifestations, in addition to
sensorineural hearing impairment, include mental retardation, psychomotor
retardation, speech delay, attention deficit hyperactivity syndrome,
autism, behavioural disorders, progressive encephalopathy,
insulin-dependent diabetes mellitus, thyroid dysfunction (hypothyroidism,
hyperthyroidism, thyroiditis), Addison disease, growth hormone deficiency,
and immunological defects.4 5 25 36 37 38
Complications
The most common complication of postnatal rubella
is arthralgia/arthritis, which occurs in 60% to 70% of teenagers and adult
women about 1 week after the rash.8
23 24
The arthralgia/arthritis usually lasts 3 to 4 days but may persist for 1
month.7 Typically, the wrists,
fingers, knees, and ankles are affected symmetrically.8 24 Morning
stiffness may also occur.10
Arthralgia/arthritis is uncommon in children and adult men.4 8 Other rare
complications include carpal tunnel syndrome, tenosynovitis,
thrombocytopenia, purpura, haemolytic anaemia, haemolytic uraemia
syndrome, myocarditis, pericarditis, hepatitis, orchitis, retinopathy,
uveitis, Guillain-Barré syndrome, and post-infectious encephalopathy.7 23 24 39 40 41 42
In addition to congenital rubella syndrome,
maternal rubella, especially during early pregnancy, may lead to
miscarriage, intrauterine fetal death, premature labour, and intrauterine
growth retardation.14 25 Individuals with congenital rubella syndrome are at
risk for deafness, blindness, hypertension, cardiac failure, academic
failure, reduced life expectancy and, in female patients, early menopause
and osteoporosis.37 The
disabilities and financial burden associated with congenital rubella
syndrome have an adverse effect on quality of life.
Diagnosis and laboratory investigations
Rubella should be suspected in a patient with
fever, erythematous maculopapular (non-vesicular) rash spreading
cephalocaudally from the face downwards, and
retroauricular/suboccipital/posterior cervical lymphadenopathy, especially
in the presence of arthralgia/arthritis. This is especially so if there is
a history of exposure to rubella, travel to an endemic area, or during an
outbreak of rubella in an individual without immunity to rubella.
Generally, clinical diagnosis of rubella is
unreliable because the clinical manifestations can be mild and
non-specific especially in young children. In addition, there are many
other viral infections having similar clinical features. Laboratory
confirmation of rubella virus infection is therefore essential. The
diagnosis of a recent postnatal rubella infection can be based on a
positive serological test for rubella-specific immunoglobulin M (IgM)
antibody in a single sample or a four-fold or greater increase in
rubella-specific immunoglobulin (IgG) titres between acute and
convalescent sera drawn 2 to 3 weeks apart.5
6 8
24 Among all the serologic tests
available, enzyme linked immunoassays (ELISA) are most commonly used to
measure rubella-specific IgG and IgM because they are very sensitive,
highly specific, technically easy to perform, rapid, and relatively
inexpensive.8 10 Rubella-specific IgM antibody is present in
approximately 50% of patients on the day of appearance of the rash but in
almost all the cases 5 days after the onset of rash; the IgM antibody
tends to persist ≥8 weeks.5 8 As such, rubella-specific IgM antibody might be falsely
negative if the test is conducted early. In contrast, false positive
results may rarely occur in patients with heterophile antibodies,
rheumatoid factors, parvovirus B19 infection, and cytomegalovirus
infection.1 8 The use of IgM-capture ELISA rather than indirect IgM
ELISA may reduce the occurrence of false positive results.1 8 When the
first serum sample was collected months after clinical symptoms, avidity
(strength of antigen-antibody binding) test of rubella-specific IgG
antibody, if available, can be used to differentiate a recent primary
infection from a past infection or reinfection.3
5 8
Low avidity anti-rubella IgG suggests recent primary rubella infection
while high avidity is consistent with previous rubella vaccination, past
rubella infection, or reinfection.3
5 7
8
Although rubella virus can be isolated most
consistently from nasopharyngeal and throat specimens, viral culture is
generally not necessary because viral culture is expensive,
time-consuming, and not readily available. Rubella virus culture is done
mainly for academic and epidemiological purposes to facilitate
surveillance during outbreaks.10
Rubella virus RNA testing by real-time reverse transcriptase-polymerase
chain reaction (RT-PCR), if available, may be performed for diagnosis and
genotype identification.1 10
The diagnosis of congenital rubella syndrome can be
confirmed by the detection of rubella-specific IgM antibody in the cord
blood or in the neonatal serum collected within the first 6 months of
life.1 25
In infants older than 3 months, a negative IgM does not exclude a
congenital rubella infection although a positive test does support the
diagnosis.23 25 Congenital rubella infection can also be confirmed by
demonstrating persistent or increasing serum concentrations of
rubella-specific IgG over the first 7 to 11 months of life.1 Detection of
rubella virus RNA by RT-PCR in nasopharyngeal swab or urine provides
laboratory evidence of congenital rubella syndrome.4 6 8 25
Differential diagnosis
The differential diagnosis includes measles,
scarlet fever, roseola infantum (exanthem subitum), erythema infectiosum
(fifth disease), infectious mononucleosis, mycoplasma infection,
rash-associated enteroviral infection, Kawasaki disease, drug eruption,
contact dermatitis, dengue, toxoplasmosis, cytomegalovirus infection, Zika
virus infection, West Nile fever, Ross River fever, and Chikungunya fever.8 14
21 23
43 44
Management
Treatment of postnatally acquired rubella in a
non-gravid individual is mainly symptomatic and consists of the use of
non-steroidal anti-inflammatory drugs for severe arthralgia/arthritis.10 In a gravid individual with rubella infection,
management depends on the gestation age at the time of infection.7 If the infection occurs before 20 weeks’ gestation, the
fetus is at risk for malformation.10
24 25
Termination of pregnancy should be discussed as an option based on local
legislation. Immune globulin administered intramuscularly or intravenously
should be considered for susceptible women with known rubella exposure in
early pregnancy for whom termination of pregnancy is not an option.4 6 24
Treatment of children with congenital rubella
syndrome should be symptomatic and organ-specific and directed to improve
the patient outcome and quality of life. Children with congenital rubella
syndrome often present with a broad range of problems and therefore will
benefit from a multidisciplinary approach. Consultations with, among
others, a paediatrician, ophthalmologist, cardiologist,
otorhinolaryngologist, and speech pathologist should be considered.
Because children with congenital rubella syndrome are at risk for delayed
manifestations, long-term audiologic, ophthalmic, and neurodevelopmental
follow-up is indicated for early identification of these disorders. Early
intervention is important to educate the family, organise the most
appropriate educational placement, and plan specialist referral and
follow-up.
Prevention
Immunisation
Universal childhood immunisation and vaccination of
all susceptible patients with rubella vaccine to decrease circulation of
the virus are the cornerstones to prevention of rubella and, more
importantly, congenital rubella syndrome. The current strategy is to
immunise all children aged 12 to 15 months and again at age 4 to 6 years
with rubella vaccine, according to recommendations for routine measles,
mumps, rubella, and varicella vaccination.1
One dose of rubella vaccine given at or after age 1 year is 95% effective
in protecting against rubella infection whereas two doses given at
appropriate intervals is close to 100% effective.4
5 8
14 Women of childbearing age
without documentation of rubella immunity should get vaccinated before
they become pregnant.1 14 Women receiving rubella vaccine should be advised to
avoid pregnancy for 1 month after rubella vaccination.4 10 Routine
prenatal screening for immunity to rubella should be performed.1 Rubella susceptible women should receive
measles-mumps-rubella (MMR) vaccine in the immediate postpartum period as
a significant number of these individuals are also susceptible to measles
and/or mumps.10
Globally, the most commonly used rubella vaccines
contain a live attenuated RA 27/3 strain grown in human diploid cell
cultures.1 8 24 China and
Japan use BRD-2 and TO-336 strains, respectively.7
The vaccines, once administered, would replicate within the host to induce
both humoral and cellular immunity.1
8 24
Rubella vaccines can be given subcutaneously as a single component (eg, in
Russia and some African countries), but more often, as combination
vaccines such as measles-mumps-rubella-varicella (MMRV) vaccine and MMR
vaccine.8 10 The MMRV vaccine has similar safety profile and
immunogenicity as the MMR vaccine except that MMRV vaccine has a two-fold
increase in relative risk of febrile seizures.45
Rubella vaccines are generally safe, immunogenic,
highly cost-effective, and well tolerated.5
Adverse effects usually occur 5 to 12 days post-vaccination and consist
mainly of fever (15%), rash (5%), transient arthralgia/arthritis, and mild
lymphadenopathy.1 7 10 24 Rare adverse effects include febrile seizures,
parotiditis, thrombocytopenic purpura, anterior uveitis, cataract,
anaphylaxis, and encephalitis.7 46
Rubella vaccine given to a nursing mother does not
affect the safety of breastfeeding both for the mother and infant.1 As such, breastfeeding is not a contra-indication to
rubella immunisation.1
Contra-indications for rubella vaccination include febrile illness,
moderate/severe illness, immunodeficiency, hypersensitivity to any
component of the vaccine including gelatine and neomycin, confirmed
history of an anaphylactic reaction to a previous rubella-containing
vaccine, and pregnancy.4 10 However, inadvertent administration of a
rubella-containing vaccine to pregnant mothers is not known to cause fetal
and/or maternal complications.4 10 24
Rubella vaccination should be deferred for at least 4 weeks in those
individuals with recent use of high-dose corticosteroids (>2 mg/kg or
20 mg/day) for ≥14 days or recent administration of immunoglobulin or
blood products.1 The rubella
vaccine can be given at the same time as other live vaccines, but should
be deferred for 3 weeks after another live vaccine has been given.4
Infection control
Confirmed cases of rubella should be excluded from
day care or school for at least 7 days after onset of the rash.1 Proper
hand washing technique and droplet precautions should be emphasised.14
Children with congenital rubella syndrome can
transmit the disease as long as they are shedding the virus. Approximately
20% of children with congenital rubella syndrome may still be shedding the
virus from the pharynx at aged 1 year and therefore are contagious.3 These individuals should be isolated to avoid the
spread of the infection until two throat swab or urine cultures obtained
at least 1 month apart are negative for the rubella virus.1 Only healthcare providers with immunity to rubella
should be involved in the care of these patients.
Prognosis
Postnatally acquired rubella is generally a mild,
self-limited, and relatively benign infection without consequences in most
cases.35 However, infection in
early pregnancy may lead to miscarriage, intrauterine fetal death,
premature labour, and congenital rubella syndrome. The prognosis of
children with congenital rubella syndrome varies, depending on the
severity and number of organs affected. Infants with thrombocytopenia,
hepatosplenomegaly, interstitial pneumonia, and pulmonary hypertension
have a high risk of mortality.34 47 Of those who develop
thrombocytopenia and hepatosplenomegaly in the neonatal period,
approximately 15% die within the first year of life.3
Conclusions
Apart from congenital infection, rubella is
generally a mild and self-limited disease in children. Rubella when
acquired by a pregnant mother in an early stage of the pregnancy can have
catastrophic effects on the developing fetus and may result in
miscarriage, intrauterine fetal death, premature labour, intrauterine
growth retardation, and congenital rubella syndrome. To eliminate rubella
from a population, universal childhood immunisation and vaccination of all
susceptible individuals with rubella vaccine is required. Although rubella
has been eliminated from most developed countries, physicians should
remain vigilant in recognising both postnatal rubella and congenital
rubella syndrome because rubella cases can be “imported” from those
countries where rubella is endemic.
Author contributions
All authors have made substantial contributions to
the concept or design of the study, acquisition of data, analysis or
interpretation of data, drafting of the manuscript, and critical revision
for important intellectual content. All authors had full access to the
data, contributed to the study, approved the final version for
publication, and take responsibility for its accuracy and integrity.
Conflicts of interest
All authors have disclosed no conflict of interest.
Funding/support
This research received no specific grant from any
funding agency in the public, commercial, or not-for-profit sectors.
Ethics approval
All patients were treated in accordance with the
Declaration of Helsinki. The parents of all patients provided written
informed consent for photographs to be taken and published.
References
1. Kimberlin DW, Brady MT, Jackson MA, Long
SS, editors. Red Book: 2018 Report of the Committee on Infectious
Diseases. 31st ed. Itasca: American Academy of Pediatrics; 2018: 705-11.
2. Veale H. History of an epidemic of
Rötheln with observations on its pathology. Edinb Med J 1866;12:404-14.
3. Drutz JE. Rubella. Pediatr Rev
2010;31:129-30. Crossref
4. Best JM. Rubella. Semin Fetal Neonatal
Med 2007;12:182-92. Crossref
5. Lambert N, Strebel P, Orenstein W,
Icenogle J, Poland GA. Rubella. Lancet 2015;385:2297-307. Crossref
6. Tyor W, Harrison T. Mumps and rubella.
Handb Clin Neurol 2014;123:591-600. Crossref
7. Bouthry E, Picone O, Hamdi G,
Grangeot-Keros L, Ayoubi JM, Vauloup-Fellous C. Rubella and pregnancy:
diagnosis, management and outcomes. Prenat Diagn 2014;34:1246-53. Crossref
8. Edwards MS. Rubella. Available from:
https://www.uptodate.com/contents/rubella. Accessed 5 Dec 2018.
9. De Santis M, Cavaliere AF, Straface G,
Caruso A. Rubella infection in pregnancy. Reprod Toxicol 2006;21:390-8. Crossref
10. Riley LE. Rubella in pregnancy.
Available from:
https://www.uptodate.com/contents/rubella-in-pregnancy. Accessed 10 Dec
2018.
11. Duszak RS. Congenital rubella
syndrome—major review. Optometry 2009;80:36-43.
12. Kirby T. Rubella is eliminated from
the Americas. Lancet Infect Dis 2015;15:768-9. Crossref
13. Fang J, Agrawal A, Gowtham S, et al.
Case report: congenital rubella syndrome: a rare but persistent concern in
the United States. J Perinatol 2013;33:899-902. Crossref
14. Shukla S, Maraqa NF. Congenital
rubella. StatPearls. Available from:
https://www.ncbi.nlm.nih.gov/books/NBK507879/. Accessed 10 Jan 2019.
15. Rubella vaccines: WHO position paper.
Wkly Epidemiol Rec 2011;86:301-16.
16. Martínez-Quintana E,
Castillo-Solórzano C, Torner N, Rodríguez-González F. Congenital rubella
syndrome: a matter of concern. Rev Panam Salud Publica 2015;37:179-86.
17. Grant GB, Reef SE, Patel M, Knapp JK,
Dabbagh A. Progress in rubella and congenital rubella syndrome control and
elimination—Worldwide, 2000-2016. MMWR Morb Mortal Wkly Rep
2017;66:1256-60. Crossref
18. Chang C, Ma H, Liang W, et al. Rubella
outbreak and outbreak management in a school setting, China, 2014. Hum
Vaccin Immunother 2017;13:772-5. Crossref
19. Hackett DW. Japan’s rubella outbreak
reaches 2,186 cases. 29 Nov 2018. Available from:
https://www.precisionvaccinations.com/travel-alert-level-2-remains-active-regarding-japan%E2%80%99s-rubella-outbreak.
Accessed 14 Mar 2019.
20. Hong Kong SAR Government. Press
release. Public and travellers urged to guard against infectious diseases
during Lunar New Year holiday. Available from:
https://www.info.gov.hk/gia/general/201901/25/P2019012500443.htm. Accessed
10 Nov 2019.
21. Chan T, MacFadden DR, Leis JA. Rubella
in a returned traveller. CMAJ 2016;188:363-6. Crossref
22. Sadlier C, Carr A, Bergin C. High
levels of susceptibility to measles, mumps and rubella (MMR) in
HIV-infected individuals in Ireland. J Infect 2016;73:84-6. Crossref
23. Banatvala JE, Brown DW. Rubella.
Lancet 2004;363:1127-37. Crossref
24. Dontigny L, Arsenault MY, Martel MJ.
No. 203—Rubella in pregnancy. J Obstet Gynaecol Can 2018;40:e615-21. Crossref
25. Dobson SR. Congenital rubella
syndrome: clinical features and diagnosis. Available from:
https://www.uptodate.com/contents/congenital-rubella-syndrome-clinical-features-and-diagnosis/print.
Accessed 15 Dec 2018.
26. Cordier AG, Vauloup-Fellous C,
Grangeot-Keros L, et al. Pitfalls in the diagnosis of congenital rubella
syndrome in the first trimester of pregnancy. Prenat Diagn 2012;32:496-7.
Crossref
27. Bypareddy R, Chawla R, Azad SV,
Khokhar S. Rubella cataract and retinopathy. BMJ Case Rep 2016;2016. pii:
bcr2016216112.
28. Gupta S, Ali MJ, Naik MN. Lacrimal
drainage anomalies in congenital rubella syndrome. Clin Ophthalmol
2017;11:1975-7. Crossref
29. Nagasawa K, Ishiwada N, Ogura A, et
al. Congenital rubella syndrome: a case report on changes in viral load
and rubella antibody titers. Pediatrics 2016;137. pii: e20153333. Crossref
30. Ahuja R, Shigli AL, Thakur G, Jain U.
Dental manifestations of congenital rubella syndrome. BMJ Case Rep
2015;2015. pii: bcr2015209382.
31. Ajij M, Nangia S, Dubey BS. Congenital
rubella syndrome with blueberry muffin lesions and extensive metaphysitis.
J Clin Diagn Res 2014;8:PD03-4. Crossref
32. Gandhi N, Mendiratta V, Shukla S,
Rawat R, Rana S, Chander R. Violaceous maculopapular rash in a newborn:
Congenital rubella syndrome. Indian J Dermatol 2015;60:521. Crossref
33. Kumar D, Jajoo M. Congenital rubella
syndrome: an unusual cause of neonatal fulminant hepatic failure. Trop
Doct 2018;48:66-8. Crossref
34. Mizuno Y, Yokoi K, Suzuki S.
Congenital rubella syndrome with death from interstitial pneumonia.
Pediatr Int 2016;58:490-3. Crossref
35. Yazigi A, De Pecoulas AE,
Vauloup-Fellous C, Grangeot-Keros L, Ayoubi JM, Picone O. Fetal and
neonatal abnormalities due to congenital rubella syndrome: a review of
literature. J Matern Fetal Neonatal Med 2017;30:274-8. Crossref
36. Chauhan N, Sen MS, Jhanda S, Grover S.
Psychiatric manifestations of congenital rubella syndrome: a case report
and review of literature. J Pediatr Neurosci 2016;11:137-9. Crossref
37. Dammeyer J. Congenital rubella
syndrome and delayed manifestations. Int J Pediatr Otorhinolaryngol
2010;74:1067-70. Crossref
38. Hutton J. Does rubella cause autism: a
2015 reappraisal? Front Hum Neurosci 2016;10:25. Crossref
39. Bharadwaj SD, Sahay RR, Yadav PD, et
al. Acute encephalitis with atypical presentation of rubella in family
cluster, India. Emerg Infect Dis 2018;24:1923-5. Crossref
40. Chaari A, Bahloul M, Berrajah L, et
al. Childhood rubella encephalitis: diagnosis, management, and outcome. J
Child Neurol 2014;29:49-53. Crossref
41. Kamiya K, Nishio E, Horio A, Tokura Y.
Unusual clinical manifestations of rubella in the elderly. Int J Dermatol
2016;55:e371-2. Crossref
42. Robson WL, Leung AK, Kaplan BS.
Hemolytic-uremic syndrome. Curr Probl Pediatr 1993;23:16-33. Crossref
43. Leung AK, Hon KL, Leong KF, Sergi CM.
Measles: a disease often forgotten but not gone. Hong Kong Med J
2018;24:512-20. Crossref
44. Vaidya SR, Raut CG, Jadhav SM.
Laboratory confirmation of rubella infection in suspected measles cases. J
Med Virol 2016;88:1685-9. Crossref
45. Leung AK, Hon KL, Leung TN. Febrile
seizures: an overview. Drugs Context 2018;7:212536. Crossref
46. Ferrini W, Aubert V, Balmer A, Munier
FL, Abouzeid H. Anterior uveitis and cataract after rubella vaccination: a
case report of a 12-month-old girl. Pediatrics 2013;132:e1035-8. Crossref
47. Toizumi M, Motomura H, Vo HM, et al.
Mortality associated with pulmonary hypertension in congenital rubella
syndrome. Pediatrics 2014;134:e519-26. Crossref

