Hong
Kong Med J 2018 Aug;24(4):400–7 | Epub 27 Jul 2018
DOI: 10.12809/hkmj177141
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
REVIEW ARTICLE
Mixed methods study on elimination of tuberculosis in
Hong Kong
Greta Tam, MB, BS, MS; H Yang, MPH; Tammy Meyers,
MB, BS, PhD
Jockey Club School of Public Health and Primary
Care, The Chinese University of Hong Kong, Shatin, Hong Kong
Corresponding author: Prof Greta Tam (gretatam@cuhk.edu.hk)
Abstract
Introduction: Tuberculosis
(TB) commonly affects developing countries. Several developed regions in
Asian still have a stagnant intermediate TB burden. Information to
adequately inform TB strategies is lacking. We conducted a mixed methods
study to fill this information gap in Hong Kong.
Methods: Data from the Hong Kong
government were used to analyse trends of TB notification rates compared
with World Health Organization (WHO) targets. A review of policy
documents and literature was conducted to evaluate TB control and
elimination in Hong Kong.
Results: Extrapolated trends
showed that Hong Kong will be unable to meet the WHO target of a 90%
drop in incidence rate by 2030. The policy review showed that the Hong
Kong government has not set a clear strategy and timeline for specific
goals in TB control and elimination. The literature review found that
older adults are largely responsible for the stagnant TB prevalence
because of reactivation of latent TB infection, while mortality
of hospitalised patients with TB is still high because of delayed
diagnosis and treatment.
Conclusion: Tuberculosis
incidence is currently under control in Hong Kong, but further actions
are needed if the elimination targets are to be achieved. Improved
diagnostic tools are required, and policies targeting latent TB infection in older
adults should be implemented to achieve the WHO target by 2030.
Introduction
Tuberculosis (TB) is a major global health burden
that ranks with human immunodeficiency virus (HIV)/acquired immune
deficiency syndrome (AIDS) as a leading cause of death worldwide. The
World Health Organization (WHO) estimated that 9.6 million people were
sickened by TB and 1.5 million died as a result in 2014, with 58% of
global TB cases occurring in the South-East Asia and Western Pacific
regions.1 2 As a part of the global response to TB, the sixth
Millennium Development Goal (MDG) set out to halve TB prevalence and
mortality rates by 2015 compared with the 1990 baseline.3 Following significant declines in TB mortality and
prevalence rates, in 2015, the third Sustainable Development Goals
contained targets to end the epidemics of AIDS, TB, malaria, and neglected
tropical disease by 2030.4 The TB
target for 2030 is to reduce the number of TB deaths by 90% compared with
2015 numbers. The WHO established the End TB Strategy in 2014, aiming to
reduce the TB burden by 2030 and eliminate TB entirely by 2050.5 6 Advanced
economies such as the US and Australia7
typically have low TB incidence, and TB is commonly known as a disease of
poverty that more heavily affects developing countries.8 The Global Fund is conducting country case studies on
HIV/AIDS, TB, and malaria in several developing countries, including
Haiti, Pakistan, and the Philippines.9
No country case studies have yet been conducted in developed Asian
countries/regions such as Hong Kong, Japan, Singapore, Taiwan, or South
Korea, which have good health infrastructure and stable economic growth,
but where intermediate levels of TB incidence persist.10 11
Reaching the WHO targets in Asia will require
strategies specific to TB epidemiology in this setting. However,
information to adequately inform strategies is lacking. The last report of
comparative data between Asian countries was published 10 years ago by the
WHO.5 The reasons for the gap
between the TB burden in Asian countries and that in their equally
developed counterparts in other regions need to be understood. The TB
burden in low-incidence countries is attributable mostly to immigrants.12 In contrast, the stagnant
intermediate incidence in developed Asian countries is ascribed mainly to
latent TB infection in ageing populations.13
Compared with that of Singapore, Japan, or Western
countries with similar gross domestic products, the notification rate of
TB in Hong Kong is relatively high (60 per 100 000 population in 2016).11 14
Presently, TB is the second most common notifiable disease in Hong Kong,
following chickenpox.15 The TB
notification rate in Hong Kong has declined slowly since 1995, although
the notification rate only dropped below 100 per 100 000 population in 2002,
and it took until 2011 for the notification rate to decline below 70 per
100 000 population.16
The present case study of the TB situation in Hong
Kong highlights successful policies intended to achieve WHO goals and
identifies areas for further research or intervention in gaps that could
prevent attainment of these targets. This could facilitate useful
comparisons with the situation in other developed Asian countries.
Methods
Secondary data analysis of publicly available data
A document review including both policy and
literature was conducted. Statistics on TB notification in Hong Kong were
obtained from the official website of the Tuberculosis and Chest Service,
Department of Health of Hong Kong SAR Government.14
The TB notification rates were analysed in terms of immigrant status,
age-group, and gender and presented in line graphs. The notification trend
was extrapolated to 2030 by using Microsoft Excel’s FORECAST function on
the trend in the past 10 years (2005-2015).
Policy review
Existing documents from the Tuberculosis and Chest
Service, Department of Health of Hong Kong SAR Government, such as the TB
manual (2006),17 TB annual reports
(2007-2013),18 19 20 21 22 23 24
information and guidelines (2006-2015),25
26 27
28 29
30 31
and other recommendations were obtained. Reports and strategies regarding
TB control and elimination from the WHO were also reviewed to analyse how
the strategy had been operationalised, how this may affect implementation
of local programmes, and to identify the policy gap between the Hong Kong
government’s and WHO’s strategies.
Literature review
Two electronic databases, PubMed and Google
Scholar, were searched to identify articles related to TB control and
elimination in Hong Kong. The key words ‘tuberculosis’ or ‘TB’ in
combination with the terms ‘Hong Kong’, ‘epidemiology’, ‘risk factors’,
‘prevention’, ‘treatment’, ‘Latent TB’, ‘MDR-TB’, or ‘XDR-TB’ were used to
search for relevant articles.
Selected publications included studies (a) carried
out in Hong Kong; (b) published in the past 10 years; (c) related to TB
prevalence, at-risk populations, and TB control measures/interventions in
Hong Kong; (d) with full-text articles in English; (e) with no overlapping
data; and (f) qualitative studies with sufficient sample size, significant
results (P<0.05), and specified outcomes/outputs.
Results
Tuberculosis notification in Hong Kong
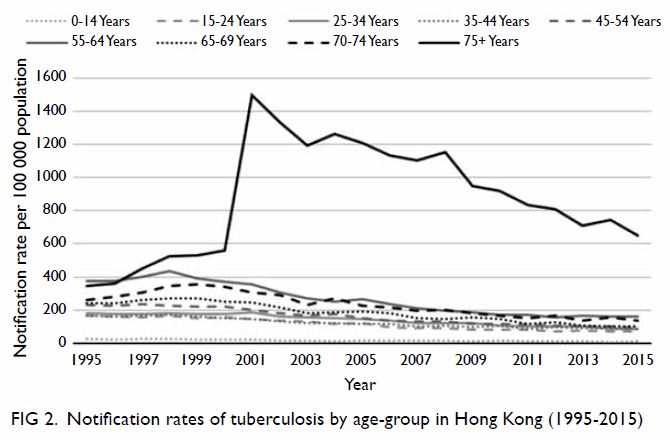
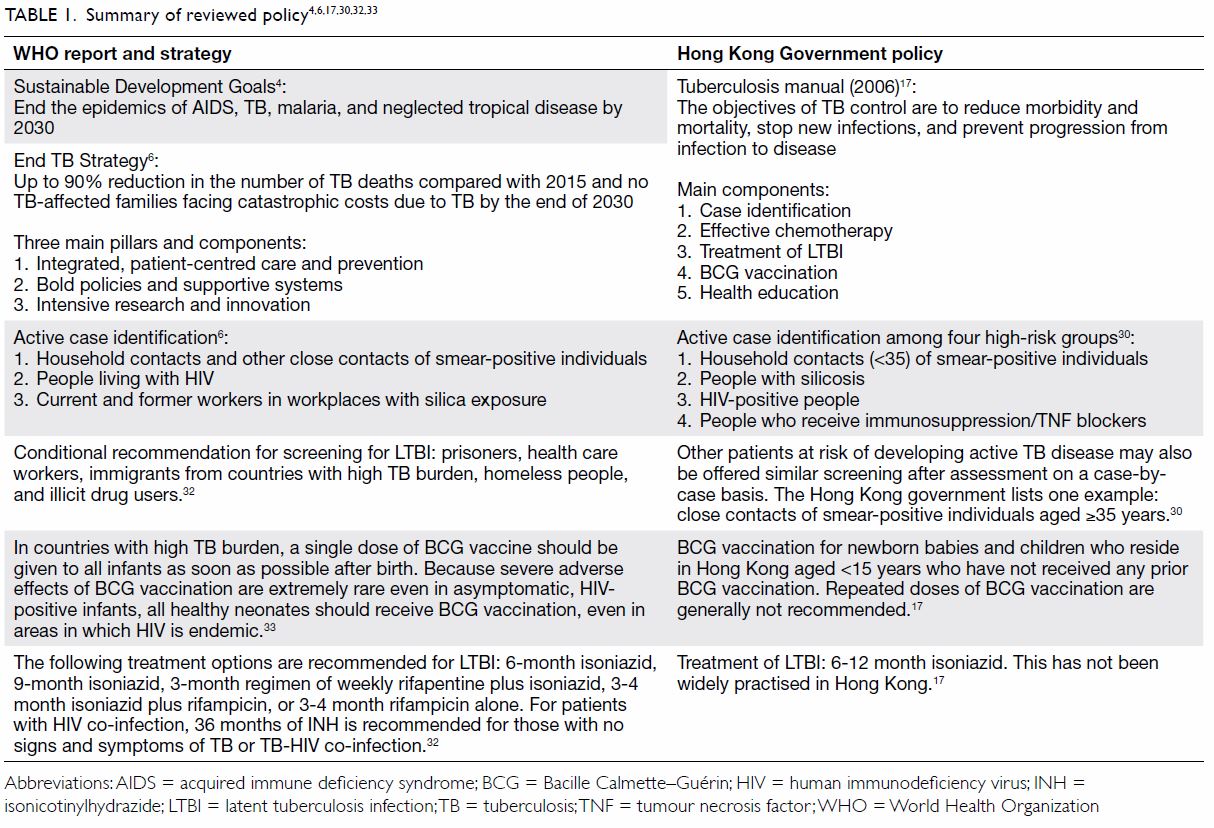
Since 1947, a downward trend in total TB
notification in Hong Kong has been observed. From 1970 to 1977, TB
notification rapidly declined but remained stagnant thereafter (Fig
1). The oldest age-group (≥75 years) had much higher TB notification
rates (Fig 2). Between 1995 and 2015, reductions in
notification rates occurred in younger age-groups but increased sharply at
the turn of the millennium in the oldest group, whose notification rate
had only gradually decreased by 2015. Notification rates in both genders
showed downward trends, although men had a higher notification rate than
women (data not shown).
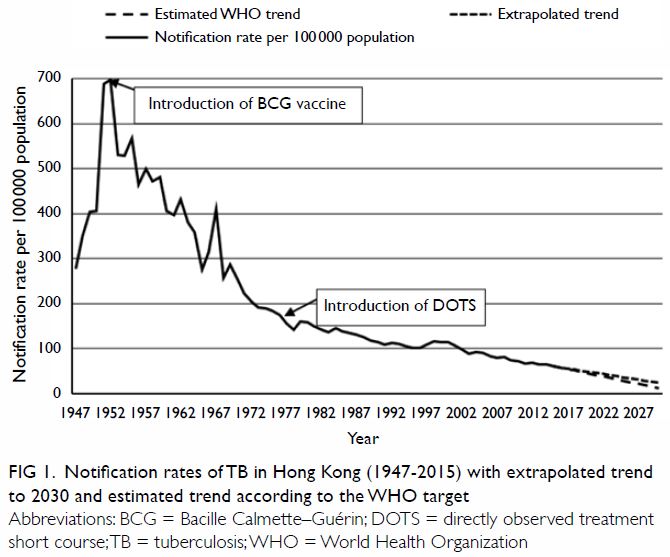
Figure 1. Notification rates of TB in Hong Kong (1947-2015) with extrapolated trend to 2030 and estimated trend according to the WHO target
Tuberculosis notification rates dropped rapidly
after the Bacille Calmette–Guérin (BCG) vaccine was introduced in 1952,
with a further decline after the introduction of directly observed
treatment short course (DOTS) [Fig 1]. The incidence in 2015 had almost halved
compared with that in 1990. Extrapolated trends showed that at the current
rate, Hong Kong would be unable to meet the WHO target of a 90% drop in
incidence rate by 2030. By then, Hong Kong’s TB notification rate is
predicted to drop by only 60.2%, compared with that in 2015. The analysis
shows that Hong Kong could become a low-incidence country (10 cases per
100 000 population) by 2036.
Comparison of reviewed policy between the World Health
Organization and Hong Kong
A comparison between the WHO’s and Hong Kong’s TB
policies is shown in Table 1.4 6 17
30 32
33 In 2015, the Sustainable
Development Goal 3 included a target to end the TB epidemic by 2030,4 and the End TB Strategy aims to achieve a 90% drop in
TB incidence rate and up to 95% reduction in number of TB-related deaths
by 2035 compared with those in 2015.6
Yet, the Hong Kong government has not set a clear strategy and timeline
for specific goals in TB control and elimination.
The WHO guidelines for management of latent TB
infection (LTBI) strongly recommended that high-income and upper-middle
income countries with TB incidence less than 100 per 100 000 population
per year perform systematic testing and treatment of LTBI in specific
groups, and Hong Kong was listed among these.32
Hong Kong follows the WHO recommendations for LTBI screening in high-risk
groups. However, conditional recommendations for a number of target
populations to be included in active case finding are not included in the
local Hong Kong policy documents. According to the Hong Kong TB Manual,
active case finding in high-risk groups was not very effective, as only 1%
of active TB was found in household contacts in 2004.17
Summary of reviewed literature
We reviewed the TB literature about studies
conducted in Hong Kong published in the past 10 years (Table
2).34 35 36 37 38 39 40 41 42 43 44 45 46 Thirteen
published studies were included: two on older adults in old age homes, one
on migrant populations, two on drug-resistant TB, two on HIV-related TB,
two on primary school children, three on TB treatment outcomes, and one on
TB prevalence in Hong Kong.
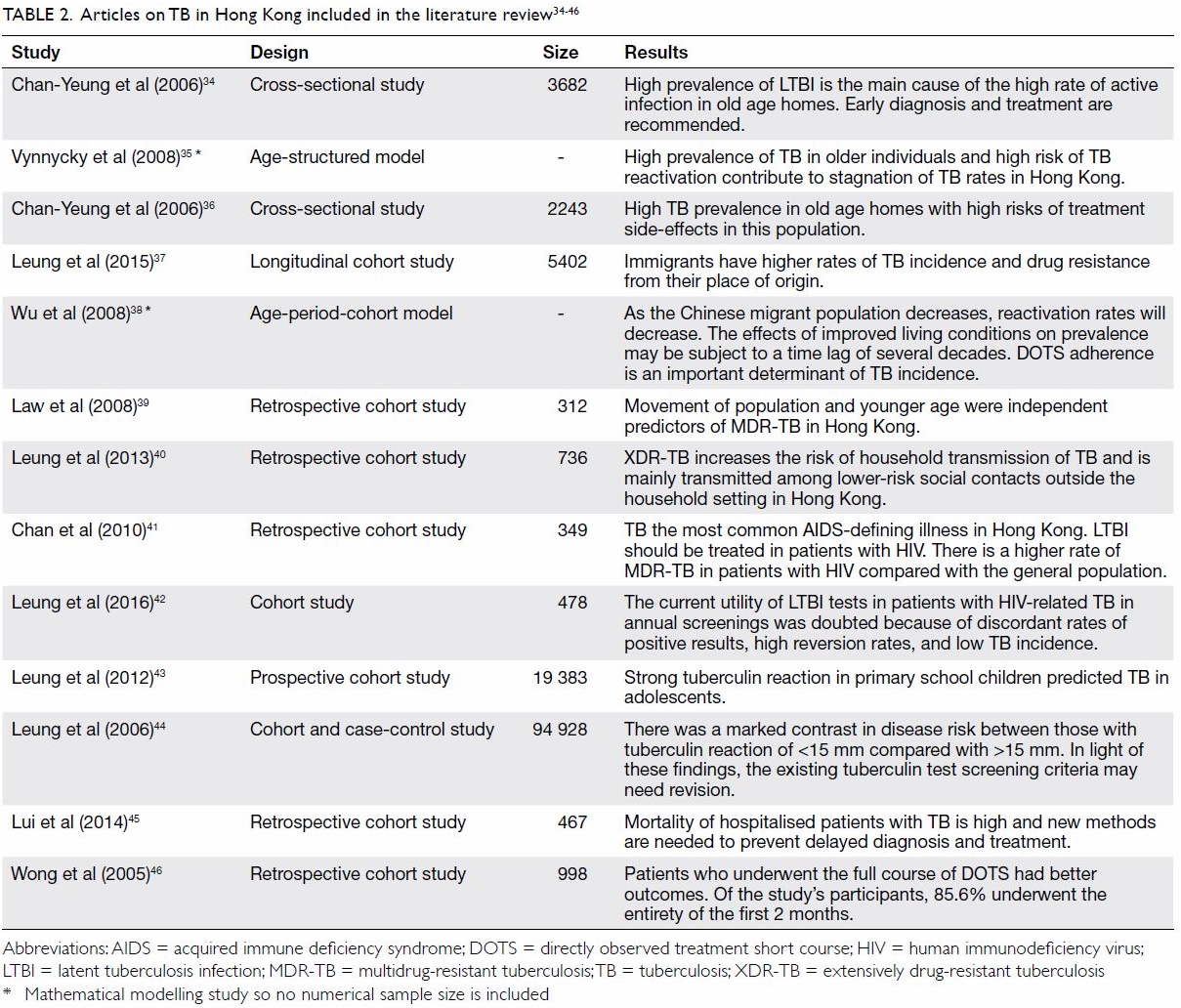
Table 2. Articles on TB in Hong Kong included in the literature review34 35 36 37 38 39 40 41 42 43 44 45 46
Among the included studies, three indicated that
Hong Kong’s TB prevalence rate is stagnating because of high TB prevalence
in older adults and a high risk of TB reactivation34 35 caused by
high prevalence of latent infection among older adults in old age homes.36 Some immigrants come from
countries with higher TB incidence and drug resistance rates, particularly
mainland China. These migrants may also be at increased risk of TB
reactivation.37 However, TB in the
migrant population is likely to decrease as migration from China is
reduced and living conditions for those entering the city improve.38
Multidrug-resistant TB (MDR-TB) is a threat that is
more likely in patients diagnosed with TB at younger ages.39 Extensively drug-resistant TB (XDR-TB) significantly
increases household TB transmission, demonstrating a need for prolonged
household surveillance.40
Treatment of LTBI is recommended to control TB, especially among people
with HIV. Two studies reported outcomes of treating LTBI in patients with
HIV in Hong Kong, one confirming the usefulness of LTBI treatment,41 while the other doubted the utility of LTBI tests in
annual screening of patients with HIV because of discordant results
between different tests.42
Identification of children with LTBI is also useful: in a study that
described the use of tuberculin tests to screen primary school children,
strong tuberculin reactions (>15 mm) predicted TB in adolescence.43 44 Diagnosis
of TB is still problematic, and new methods are needed to prevent delayed
diagnosis and treatment,35 as
mortality of hospitalised TB patients is still high.45 However, one Hong Kong study demonstrated that
although early diagnosis and treatment are recommended, TB therapy carried
a high risk of side-effects in the study population.36 Directly observed treatment short course has
significantly decreased TB incidence,38
46 although not all patients in
Hong Kong completed the first 2 months of treatment, with failure to
complete treatment predicting poorer outcomes than undergoing the full
course.46
Discussion
In Hong Kong’s older adult population, TB accounts
for the majority of the city’s high burden from the disease. In Hong Kong,
those aged >75 years showed an especially high TB incidence rate.
Migrants and people with HIV also have higher TB prevalence but contribute
significantly less to the burden than do older adults. Children with a
strong purified protein derivative reaction indicating infection were more
prone to develop TB in adolescence. Also, MDR-TB and XDR-TB pose a
relatively rare but important threat in Hong Kong. Late or underdiagnosis
results in high TB-related mortality in those who present symptoms late
and require hospitalisation.
High rates of LTBI in Hong Kong have been
documented in other Asian countries with low and intermediate TB burden.47 The BCG vaccine was introduced
to Hong Kong in April 195217;
therefore, by 1995, 2005 and 2015, those aged >43, >53 and >63
years, respectively, would not have been vaccinated in infancy. The higher
prevalence of LTBI and active TB in old age homes compared with that in
older adults living in the community is a trend shared with other
countries, including low-burden countries such as the US.48 49 50 Despite the higher prevalence of LTBI in
institutionalised older adults in Hong Kong (68.6%)36 compared with their American counterparts (5.5%),51 52 53 54 55 56 Hong Kong
has not followed the US policy of LTBI testing in this population.57 Further research is needed to explore the feasibility
and cost-effectiveness of screening and providing prophylaxis to older
adults and other populations.
In contrast to countries with low TB burden, where
infections in migrants primarily contribute to the burden,58 the infection rate in Hong Kong’s migrant population
is declining.16 However, MDR-TB
rates are higher in migrants and younger age-groups in Hong Kong and
countries with low TB burden.59 60 A systematic review also
concurred with a Hong Kong study’s findings that patients with HIV had a
higher risk of MDR-TB.41 61 Meanwhile, the findings on transmission of XDR-TB in
Hong Kong differ from those in Peru, where household contacts reported a
very high prevalence of XDR-TB.62
It has been postulated that in Hong Kong, XDR-TB is mainly transmitted
outside the household setting because of the high population density.40 The Peru study’s different findings may support this
idea, as the population density of Hong Kong is more than double that of
Lima.63 64
The WHO has called for improved tests to diagnose
LTBI, as the current ones lack accuracy.65
This was echoed by findings in the study of patients with HIV by Leung et
al.42 The finding that a strong
tuberculin reaction in 6-to-10-year-old schoolchildren in Hong Kong
predicted TB in adolescence was reinforced by a similar study in
Singapore, which is also a developed city with an intermediate TB burden.43 66
67 However, Hong Kong
schoolchildren are not routinely screened for LTBI.30 It may be advisable to extend LTBI testing to cover
schoolchildren.
The high mortality of hospitalised patients with TB
in Hong Kong is also seen in many other countries,45 68
emphasising the need for early detection and treatment. The DOTS strategy
is an important cornerstone of TB treatment; however, there is room for
improvement in compliance with DOTS in Hong Kong.46
Other developed Asian countries have similar DOTS treatment success rates
to Hong Kong.69 Without
improvement in medication adherence, treatment success rates are unlikely
to rise.
Policy recommendations
Hong Kong reached the MDG target of reducing TB
incidence, with a declining notification rate. However, according to the
extrapolated trend, if improvements are not instituted, there will likely
be only a 60% reduction in TB notification by 2030 compared with the 2015
baseline. To achieve the goal of 80% reduction in TB incidence proposed by
the End TB Strategy,70 an improved
supportive protocol targeting older adults with a clear timeline is
needed. In addition, the Hong Kong government should consider screening
high-risk groups included in the WHO’s conditional recommendations. More
research needs to be done to explore whether screening these groups would
be beneficial.
Limitations
This study has several limitations. First, some key
literature and important policies or strategies may have been missed, as
no systematic review was conducted. This may have imposed error on the
screening and article selection. Second, some patients that did not seek
health care may have been missed by the system. Despite these limitations,
this research has provided helpful suggestions and valuable insights for
future research and implementation of TB-related policy.
Conclusion
The TB incidence rate is currently under control in
Hong Kong, but further actions are warranted if the elimination targets
are to be achieved. More accurate diagnostic tools are required, and
policies targeting LTBI in older adults and children should be implemented
to achieve the WHO goal by 2030.
Author contributions
Concept or design: G Tam.
Acquisition of data: H Yang.
Analysis or interpretation of data: H Yang.
Drafting of the article: All authors.
Critical revision for important intellectual content: G Tam, T Meyers.
Acquisition of data: H Yang.
Analysis or interpretation of data: H Yang.
Drafting of the article: All authors.
Critical revision for important intellectual content: G Tam, T Meyers.
Funding/support
This research received no specific grant from any
funding agency in the public, commercial, or not-for-profit sectors.
Declaration
All authors have disclosed no conflicts of
interest. All authors had full access to the data, contributed to the
study, approved the final version for publication, and take responsibility
for its accuracy and integrity. Abstract of this article was presented at
Infection 2016 (13th Annual Scientific Meeting), 22 June 2016, The Chinese
University of Hong Kong, Hong Kong.
References
1. World Health Organization. Tuberculosis,
Fact sheet N104. Available from:
http://www.who.int/mediacentre/factsheets/fs104/en/. Accessed 11 Jul 2018.
2. World Health Organization. Global
tuberculosis report 2015. Available from:
http://www.who.int/tb/publications/global_report/gtbr15_main_text.pdf.
Accessed 11 Jul 2018.
3. World Health Organization. Global
tuberculosis report 2014. Available from:
http://www.who.int/tb/publications/global_report/gtbr14_main_text.pdf.
Accessed 11 Jul 2018.
4. World Health Organization. Health in
2015: from MDGs to SDGs. WHO report 2015. Available from:
http://www.who.int/gho/publications/mdgs-sdgs/en/. Accessed 11 Jul 2018.
5. World Health Organization. Framework
towards TB elimination in low-incidence countries. 2014. Available from:
http://www.who.int/tb/publications/Towards_TB_Eliminationfactsheet.pdf.
Accessed 11 Jul 2018.
6. World Health Organization. The End TB
strategy; global strategy and targets for tuberculosis prevention, care
and control after 2015. 2016. Available from:
http://www.who.int/tb/post2015_TBstrategy.pdf. Accessed 11 Jul 2018.
7. International Monetary Fund. World
economic outlook: adjusting to lower commodity prices. 2015. Available
from: http://www.imf.org/external/pubs/ft/weo/2015/02/pdf/text.pdf.
Accessed 11 Jul 2018.
8. World Health Organization. Addressing
poverty in TB control. Options for national TB control programmes.
Available from:
http://www.who.int/tb/areas-of-work/population-groups/poverty/en/ Accessed
11 Jul 2018.
9. The Global Fund. Where we invest, The
Global Fund. Available from: http://www.theglobalfund.org/en/overview/.
Accessed 11 Jul 2018.
10. The World Bank. Incidence of
tuberculosis (per 100,000 people). Available from:
http://data.worldbank.org/indicator/SH.TBS.INCD. Accessed 11 Jul 2018.
11. World Health Organization.
Tuberculosis (TB), tuberculosis country profiles. Available from:
http://www.who.int/tb/country/data/profiles/en/. Accessed 11 Jul 2018.
12. Pareek M, Abubakar I, White PJ,
Garnett GP, Lalvani A. Tuberculosis screening of migrants to low-burden
nations: insights from evaluation of UK practice. Eur Respir J
2011;37:1175-82. Crossref
13. World Health Organization.
Tuberculosis control in the South-East Asia and Western Pacific regions
2005: a biregional report. Available from:
http://iris.wpro.who.int/bitstream/handle/10665.1/5519/9290611960_eng.pdf.Accessed
11 Jul 2018.
14. Tuberculosis and Chest Service,
Department of Health, Hong Kong SAR Government. Statistics on
tuberculosis, 2015. Available from:
http://www.info.gov.hk/tb_chest/index_2.htm. Accessed 11 Jul 2018.
15. Centre for Health Protection,
Department of Health, Hong Kong SAR Government. Number of notifiable
infectious disease by month in 2015, notifiable infectious disease,
Statistics on communicable diseases. Available from:
http://www.chp.gov.hk/en/data/1/10/26/43/3829.html. Accessed 11 Jul 2018.
16. Centre for Health Protection,
Department of Health, Hong Kong SAR Government. Notification and death
rate of tuberculosis (all forms), 1947-2015. Available from:
http://www.chp.gov.hk/en/data/4/10/26/43/88.html. Accessed 11 Jul 2018.
17. Tuberculosis and Chest Service,
Department of Health, Hong Kong SAR Government. Tuberculosis manual 2006.
2006. Available from:
http://www.info.gov.hk/tb_chest/doc/Tuberculosis_Manual2006.pdf. Accessed
11 Jul 2018.
18. Tuberculosis and Chest Service,
Department of Health, Hong Kong SAR Government. Annual report 2007. 2007.
Available from: http://www.info.gov.hk/tb_chest/doc/Annual Report
2007.pdf. Accessed 11 Jul 2018.
19. Tuberculosis and Chest Service,
Department of Health, Hong Kong SAR Government. Annual report 2008. 2008.
Available from:
http://www.info.gov.hk/tb_chest/doc/Annual_Report_2008.pdf. Accessed 11
Jul 2018.
20. Tuberculosis and Chest Service,
Department of Health, Hong Kong SAR Government. Annual report 2009. 2009.
Available from: http://www.info.gov.hk/tb_chest/doc/AnnualReport2009.pdf.
Accessed 11 Jul 2018.
21. Tuberculosis and Chest Service,
Department of Health, Hong Kong SAR Government. Annual report 2010. 2010.
Available from: http://www.info.gov.hk/tb_chest/doc/AnnualReport2010.pdf.
Accessed 11 Jul 2018.
22. Tuberculosis and Chest Service,
Department of Health, Hong Kong SAR Government. Annual report 2011. 2011.
Available from: http://www.info.gov.hk/tb_chest/doc/AnnualReport2011.pdf.
Accessed 11 Jul 2018.
23. Tuberculosis and Chest Service,
Department of Health, Hong Kong SAR Government. Annual report 2012. 2012.
Available from: http://www.info.gov.hk/tb_chest/doc/AnnualReport2012.pdf.
Accessed 11 Jul 2018.
24. Tuberculosis and Chest Service,
Department of Health, Hong Kong SAR Government. Annual report 2013. 2013.
Available from: http://www.info.gov.hk/tb_chest/doc/AnnualReport2013.pdf.
Accessed 11 Jul 2018.
25. Tuberculosis and Chest Service,
Department of Health, Hong Kong SAR Government. Recommendations on the
management of human immunodeficiency virus and tuberculosis coinfection.
2008. Available from:
http://www.chp.gov.hk/files/pdf/recommendations_on_management_of_human_immunodeficiency_virus_and_tuberculosis_coinfection_r.pdf.
Accessed 11 Jul 2018.
26. Tuberculosis and Chest Service,
Department of Health, Hong Kong SAR Government. Guidelines on the
management of multidrug-resistant and extensively drugresistant
tuberculosis in Hong Kong. 2008. Available from:
http://www.info.gov.hk/tb_chest/doc/MDRTBguideline_0812.pdf. Accessed 11
Jul 2018.
27. Centre for Health Protection,
Department of Health, Hong Kong SAR Government. The use of BCG vaccine in
HIV infected patients. 2009. Available from:
http://www.chp.gov.hk/files/pdf/the_use_of_bcg_vaccine_in_hiv_infected_patients_r.pdf.
Accessed 11 Jul 2018
28. Tuberculosis and Chest Service,
Department of Health, Hong Kong SAR Government. Ambulatory treatment and
public health measures for a patient with uncomplicated pulmonary
tuberculosis—an information paper. 2013. Available from:
http://www.info.gov.hk/tb_chest/doc/Information_paper_ambulatory_tb_2013.pdf.
Accessed 11 Jul 2018.
29. Tuberculosis and Chest Service,
Department of Health, Hong Kong SAR Government. Guidance on logistical
arrangement for targeted screening and treatment of latent tuberculosis
infection among immunocompetent household contacts of smear-positive
pulmonary tuberculosis patients in TB and Chest Service. 2013. Available
from:
http://www.info.gov.hk/tb_chest/doc/Guidance_Notes_Contact_TBCS_upated 1
NOV 2013.pdf. Accessed 11 Jul 2018.
30. Tuberculosis and Chest Service,
Department of Health, Hong Kong SAR Government. Guidelines on targeted
tuberculin testing and treatment of latent tuberculosis infection. 2015.
Available from:
http://www.info.gov.hk/tb_chest/doc/LTBI_guide_TBCS_2012_update 1
Nov2013_ADD_31March2015.pdf. Accessed 11 Jul 2018.
31. Tuberculosis and Chest Service,
Department of Health, Hong Kong SAR Government. Scheme for investigation
of close contacts (household) in the Tuberculosis & Chest Service,
Department of Health. 2015. Available from:
http://www.info.gov.hk/tb_chest/doc/TST_contacts of smear-negative
sources.pdf. Accessed 11 Jul 2018.
32. Getahun H, Matteelli A, Abubakar I, et
al. Management of latent mycobacterium tuberculosis infection: WHO
guidelines for low tuberculosis burden countries. Eur Respir J
2015;46:1563-76. Crossref
33. World Health Organization. Weekly
epidemiological record. 2004. Available from:
http://www.who.int/wer/2004/en/wer7904.pdf?ua=1. Accessed 11 Jul 2018.
34. Chan-Yeung M, Cheung AH, Dai DL, et
al. Prevalence and determinants of positive tuberculin reactions of
residents in old age homes in Hong Kong. Int J Tuberc Lung Dis
2006;10:892-8.
35. Vynnycky E, Borgdorff MW, Leung CC,
Tam CM, Fine PE. Limited impact of tuberculosis control in Hong Kong:
attributable to high risks of reactivation disease. Epidemiol Infect
2008;136:943-52. Crossref
36. Chan-Yeung M, Chan FH, Cheung AH, et
al. Prevalence of tuberculous infection and active tuberculosis in old age
homes in Hong Kong. J Am Geriatr Soc 2006;54:1334-40. Crossref
37. Leung CC, Chan CK, Chang KC, et al.
Immigrants and tuberculosis in Hong Kong. Hong Kong Med J 2015;21:318-26.
Crossref
38. Wu P, Cowling BJ, Schooling CM, et al.
Age-period-cohort analysis of tuberculosis notifications in Hong Kong from
1961 to 2005. Thorax 2008;63:312-6. Crossref
39. Law WS, Yew WW, Chiu Leung C, et al.
Risk factors for multidrug-resistant tuberculosis in Hong Kong. Int J
Tuberc Lung Dis 2008;12:1065-70.
40. Leung EC, Leung CC, Kam KM, et al.
Transmission of multidrug-resistant and extensively drug-resistant
tuberculosis in a metropolitan city. Eur Respir J 2013;41:901-8. Crossref
41. Chan CK, Alvarez Bognar F, Wong KH, et
al. The epidemiology and clinical manifestations of human immunodeficiency
virus–associated tuberculosis in Hong Kong. Hong Kong Med J 2010;16:192-8.
42. Leung CC, Chan K, Yam WC, et al. Poor
agreement between diagnostic tests for latent tuberculosis infection among
HIV-infected persons in Hong Kong. Respirology 2016;21:1322-9. Crossref
43. Leung CC, Yew WW, Au KF, et al. A
strong tuberculin reaction in primary school children predicts
tuberculosis in adolescence. Pediatr Infect Dis J 2012;31:150-3. Crossref
44. Leung CC, Yew WW, Chang KC, et al.
Risk of active tuberculosis among schoolchildren in Hong Kong. Arch
Pediatr Adolesc Med 2006;160:247-51. Crossref
45. Lui G, Wong RY, Li F, et al. High
mortality in adults hospitalized for active tuberculosis in a low HIV
prevalence setting. PLoS One 2014;9:e92077. Crossref
46. Wong MY, Leung CC, Tam CM, Lee SN.
Directly observed treatment of tuberculosis in Hong Kong. Int J Tuberc
Lung Dis 2005;9:443-9.
47. Mori T, Leung CC. Tuberculosis in the
global aging population. Infect Dis Clin North Am 2010;24:751-68. Crossref
48. Stead WW, Dutt AK. Tuberculosis in
elderly persons. Annu Rev Med 1991;42:267-76. Crossref
49. Stead WW, Lofgren JP, Warren E, Thomas
C. Tuberculosis as an endemic and nosocomial infection among the elderly
in nursing homes. N Engl J Med 1985;312:1483-7.Crossref
50. Macarthur C, Enarson DA, Fanning EA,
Hessel PA, Newman S. Tuberculosis among institutionalized elderly in
Alberta, Canada. Int J Epidemiol 1992;21:1175-9. Crossref
51. Shea KM, Kammerer JS, Winston CA,
Navin TR, Horsburgh CR Jr. Estimated rate of reactivation of latent
tuberculosis infection in the United States, overall and by population
subgroup. Am J Epidemiol 2014;179:216-25. Crossref
52. Welty C, Burstin S, Muspratt S, Tager
IB. Epidemiology of tuberculous infection in a chronic care population. Am
Rev Respir Dis 1985;132:133-6.
53. Dorken E, Grzybowski S, Allen EA.
Significance of the tuberculin test in the elderly. Chest 1987;92:237-40.
Crossref
54. Stead WW, To T. The significance of
the tuberculin skin test in elderly persons. Ann Intern Med
1987;107:837-42. Crossref
55. Nisar M, Williams CS, Ashby D, Davies
PD. Tuberculin testing in residential homes for the elderly. Thorax
1993;48:1257-60. Crossref
56. Creditor MC, Smith EC, Gallai JB,
Baumann M, Nelson KE. Tuberculosis, tuberculin reactivity, and delayed
cutaneous hypersensitivity in nursing home residents. J Gerontol
1988;43:M97-100. Crossref
57. Centers for Disease Control and
Prevention. Latent tuberculosis infection: a guide for primary health care
providers. 2013. Available from:
http://www.cdc.gov/tb/publications/ltbi/targetedtesting.htm. Accessed 11
Jul 2018.
58. Pareek M, Greenaway C, Noori T, Munoz
J, Zenner D. The impact of migration on tuberculosis epidemiology and
control in high-income countries: a review. BMC Med 2016;14:48. Crossref
59. Hargreaves S, Lönnroth K, Nellums LB,
et al. Multidrugresistant tuberculosis and migration to Europe. Clin
Microbiol Infect 2017;23:141-6. Crossref
60. Faustini A, Hall AJ, Perucci CA. Risk
factors for multidrug resistant tuberculosis in Europe: a systematic
review. Thorax 2006;61:158-63.Crossref
61. Mesfin YM, Hailemariam D, Biadgilign
S, Kibret KT. Association between HIV/AIDS and multi-drug resistance
tuberculosis: a systematic review and meta-analysis. PLoS One
2014;9:e82235. Crossref
62. Becerra MC, Appleton SC, Franke MF, et
al. Tuberculosis burden in households of patients with multidrug-resistant
and extensively drug-resistant tuberculosis: a retrospective cohort study.
Lancet 2011;377:147-52. Crossref
63. World population review. Lima
population 2017. 2018. Available from:
http://worldpopulationreview.com/worldcities/lima-population/. Accessed 11
Jul 2018.
64. World population review. Hong Kong
population 2017. 2018. Available from:
http://worldpopulationreview.com/countries/hong-kong-population/#.
Accessed 11 Jul 2018.
65. World Health Organization. WHO
guidelines on the management of latent tuberculosis infection launched
today. Available from: http://www.who.int/tb/features_archive/LTBI/en/.
Accessed 11 Jul 2018.
66. Chee CB, Soh CH, Boudville IC, Chor
SS, Wang YT. Interpretation of the tuberculin skin test in Mycobacterium
bovis BCG-vaccinated Singaporean schoolchildren. Am J Respir Crit Care Med
2001;164:958-61. Crossref
67. World Health Organization.
Tuberculosis. 2007. Available from:
http://www.wpro.who.int/mediacentre/factsheets/fs_20060829/en/. Accessed
11 Jul 2018.
68. Waitt CJ, Squire SB. A systematic
review of risk factors for death in adults during and after tuberculosis
treatment. Int J Tuberc Lung Dis 2011;15:871-85. Crossref
69. Tam CM. The DOTS strategy in Hong
Kong. Med Bull 2006;11:3-4.
70. World Health Organization. The End TB
Strategy. Available from: http://www.who.int/tb/End_TB_brochure.pdf?ua=1.
Accessed 11 Jul 2018.