Hong
Kong Med J 2018 Aug;24(4):378–83 | Epub 27 Jul 2018
DOI: 10.12809/hkmj187217
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE
Telepsychiatry for stable Chinese psychiatric
out-patients in custody in Hong Kong: a case-control pilot study
KM Cheng, MB, BS, FHKAM (Psychiatry)1;
Bonnie WM Siu, MB, ChB, FHKAM (Psychiatry)2; Cherie CY Au
Yeung, BSc, MStat2; TP Chiang, MB, BS, FHKAM (Psychiatry)1;
MH So, BSc3; Mick CW Yeung, FHKAN, BSc3
1 Department of General Adult
Psychiatry, Castle Peak Hospital, Tuen Mun, Hong Kong
2 Department of Forensic Psychiatry,
Castle Peak Hospital, Tuen Mun, Hong Kong
3 Correctional Services Department,
Wanchai, Hong Kong
Corresponding author: Dr Bonnie WM Siu (swm810@ha.org.hk)
Abstract
Introduction: In Hong
Kong, persons in custody receive primary medical care within the
institutions of the Correctional Services Department (CSD). However, for
psychiatric care, persons in custody must attend specialist out-patient
clinics (SOPCs), which may cause embarrassment and stigmatisation. The
aim of this interventional pilot study was to compare teleconsultations
with face-to-face consultations for a group of stable Chinese
psychiatric out-patients in custody.
Methods: A total of 86 stable
Chinese male out-patients in custody were recruited for psychiatric
teleconsultations. They were compared with 249 age-matched Chinese male
out-patients in custody attending standard face-to-face psychiatric
consultations at other SOPCs. The two groups had comparable baseline
characteristics including age, education level, and 12-item Chinese
General Health Questionnaire (C-GHQ-12) score. A satisfaction survey of
patients towards the teleconsultation was also carried out.
Results: Compared with the
face-to-face consultation group, the teleconsultation group showed a
significantly better result in the difference in C-GHQ-12 scores before
and after consultations (P=0.023). The correlation between the first and
second teleconsultations also showed a moderate positive relationship (r=0.309).
The satisfaction survey showed a favourable response to
teleconsultations. No significant adverse events were identified for the
teleconsultation group.
Conclusions: The results suggest
that teleconsultations are a sustainable and safe alternative to
face-to-face consultations for stable Chinese psychiatric out-patients
in custody.
New knowledge added by this study
- Psychiatric teleconsultations are a sustainable and safe alternative to face-to-face consultations for stable Chinese psychiatric out-patients in custody.
- The intrinsic problems of embarrassment and stigmatisation caused to persons in custody, their risk of abscondence, and the issue of general public safety can all be addressed with this promising alternative mode of psychiatric care for stable Chinese psychiatric out-patients in custody.
Introduction
Telepsychiatry is the practice of delivering mental
health consultations at a distance. New developments in information and
communication technologies have allowed telepsychiatry to become a viable
method of providing services to patients in rural or remote locations with
limited access to medical services.1
2 3
Telepsychiatry has been used in prison settings for more than 20 years.4 A demonstration of telepsychiatry
in prison in the US in 1996 concluded that this practice was
cost-effective.5 Prison
administrators even claimed that there were fewer assault incidents after
its use.5 In Hong Kong, the use of
telepsychiatry can be dated back to 1998.6
Currently, persons in custody (PICs) in Hong Kong
receive primary medical care within the institutions of the Correctional
Services Department (CSD). However, for specialist psychiatric service for
their mental problems, PICs must attend psychiatric specialist out-patient
clinics (SOPCs) of the Hospital Authority. In addition, most psychiatric
drugs are available only in SOPCs.
For security reasons, PICs must be escorted by at
least two CSD staff and be handcuffed on every occasion they need to
attend follow-up at a SOPC. Such an exposing arrangement inevitably causes
much embarrassment and stigmatisation for PICs. There is also a potential
risk to the public in the event of abscondence from custody. The PIC may
also experience travel sickness during the journey between the
correctional facilities and the SOPC; most correctional facilities in Hong
Kong are situated in relatively remote areas, so the journey times can be
long. Furthermore, other patients in the SOPC may feel uncomfortable
witnessing a PIC being handcuffed. Some SOPCs manage this problem by
placing the PIC in a special corner or room, depending on availability.
Face-to-face consultation is the gold standard for
medical practice. However, telepsychiatry is suitable for PICs and might
confer additional benefits for this group of patients. Direct physical
examinations are typically unnecessary for stable psychiatric patients
during follow-up. Additionally, the nurse at the CSD site can help measure
vital signs such as blood pressure, pulse, and temperature. Therefore,
offering PICs psychiatric teleconsultations cannot only maintain their
usual psychiatric care but also reduce embarrassment, stigmatisation, and
the risk of abscondence. Furthermore, it can also reduce the need for
special arrangements in SOPCs.
To the best of our knowledge, there have been no
previous studies exploring the effect of psychiatric teleconsultations for
Chinese psychiatric out-patients under the legal custody of the CSD in
Hong Kong. The main aim of the present study was to explore the use of
psychiatric teleconsultations for stable Chinese psychiatric out-patients
under the legal custody of the CSD in Hong Kong. The desired outcome was
to maintain the clinical interests of PICs and to provide them with
appropriate psychiatric services using telecommunications in a safe,
humane, and cost-effective manner. This was an interventional pilot study
evaluating the effect of psychiatric teleconsultations on the general
health of an intervention group of clinically stable Chinese male
psychiatric out-patients who were under the custody of the CSD as compared
with a matched control group of Chinese male psychiatric out-patients
under the usual type of care (ie, face-to-face consultation with a
psychiatrist at a SOPC). In addition, the satisfaction of patients towards
psychiatric teleconsultations was assessed.
The null hypotheses of this study were as follows:
1. After the consultation, the psychological health of the intervention group is worse than that of the control group;
2. The effect of psychiatric teleconsultations is unsustainable;
3. Patients in the intervention group are unsatisfied with the psychiatric teleconsultations;
4. Adverse events occur during psychiatric teleconsultations.
1. After the consultation, the psychological health of the intervention group is worse than that of the control group;
2. The effect of psychiatric teleconsultations is unsustainable;
3. Patients in the intervention group are unsatisfied with the psychiatric teleconsultations;
4. Adverse events occur during psychiatric teleconsultations.
Methods
This was an interventional pilot study conducted by
the Hospital Authority in collaboration with the Hong Kong CSD.
Participants
The study period was from June 2014 to May 2016.
Participants were aged 21 to 64 years. The intervention group comprised
Chinese patients in custody attending follow-up at the SOPC of Castle Peak
Hospital (CPH), Hong Kong. The control group included Chinese patients in
custody attending follow-up at other SOPCs in Hong Kong. In this study,
only male PICs were included because of logistic and feasibility reasons.
Exclusion criteria applied when selecting intervention and control
participants for this study included: (a) patients with mental instability
or with prominent and recent change/deterioration in mental condition,
such as those who were suicidal or homicidal, or who had delirium or acute
psychosis; (b) patients who required regular blood tests, such as those
taking clozapine; (c) patients requiring other tests/investigations only
available in SOPC or Hospital Authority hospitals; (d) patients requiring
drug administration in SOPC, such as depot antipsychotics; (e) patients
attending SOPC for the first time; or (f) patients with visual or auditory
deficits that might impair the ability to interact via video-conferencing. Eligible patients meeting the inclusion criteria were invited to participate in the study. Written informed consent was
obtained from the intervention and control participants.
Sample size
A sample size of at least 80 participants for the
intervention group with an intervention-to-control ratio of approximately
1:3 was adopted in this study. This was an affordable and representative
sample size with reference to the number of stable psychiatric
out-patients in custody attending follow-up appointment at the SOPC of CPH
during the study period.
Assessment tools
Socio-demographic and clinical data including age,
education level, and principal psychiatric diagnosis according to the 10th
revision of the International Classification of Diseases were obtained.7 The intervention and control participants were
requested to complete the Chinese version of the 12-item General Health
Questionnaire (C-GHQ-12).8 The GHQ
is a self-administered test used for evaluating the psychological
components of ill health and is helpful in screening for general emotional
distress.9 10 The GHQ possesses adequate content validity and
construct validity, and good internal consistency has been demonstrated
with Cronbach’s alphas ranging from 0.82 to 0.93.9
10 The Chinese and English
versions of the GHQ have been adopted for Chinese and non-Chinese
subjects, respectively.8 9 10 The
C-GHQ-12 consists of 12 items, with each item assessing the severity of a
mental problem using a 4-point Likert scale.8
The six positive items were rated from 1 (more than usual) to 4 (much less
than usual) and the six negative items from 1 (never) to 4 (much more than
usual); thus, a higher score indicates a more severe mental health
condition. In this study, the pre-consultation and post-consultation
C-GHQ-12 scores for each patient were obtained. The difference between the
two scores (ie, the pre-post difference) was used as a proxy measurement
of the quality of consultation.
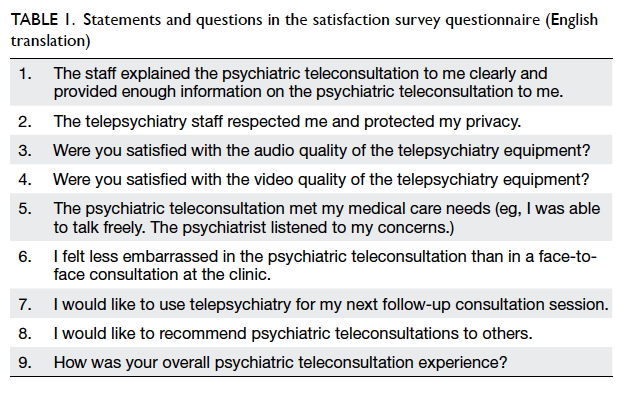
The intervention participants were also requested
to complete a questionnaire in Chinese designed to measure the patient
satisfaction regarding the psychiatric teleconsultation. The questionnaire
consisted of nine statements/questions rated according to a 5-point Likert
scale, from 1 (strongly agree) to 5 (strongly disagree) or from 1 (very
satisfied) to 5 (very dissatisfied). The questionnaire was designed by the
authors as there were no available validated Chinese questionnaires
suitable for assessing patient satisfaction of telepsychiatry at the time
of the study (English translations of the statements/questions in the
questionnaire are listed in Table 1).
Procedure
The intervention participants were transferred from
various CSD institutions to the Lai Chi Kok Reception Centre, Hong Kong,
for the psychiatric teleconsultation. On the scheduled day of
consultation, the CSD staff brought two portable video-conferencing
devices to CPH. Registration was performed only after the device had been
checked as functional. All persons in the consultation rooms at the CSD
site and at the CPH site were identified to each other prior to the
consultation session. Consultation rooms provided at both sites were
appropriately set up with particular attention to audio and visual
privacy, lighting, backdrop, and gaze angle. A qualified CSD nurse was
present in the consultation room at the CSD site together with the
patient. There was also a CSD medical doctor at the reception centre
during the psychiatric teleconsultation, in case emergency medical
treatment was needed. After the consultation, the CSD staff collected the
medicine for the patient according to the usual procedures. For the
intervention participants, the maximum number of consecutive psychiatric
teleconsultations was set as four, after which a face-to-face follow-up
consultation must follow. The control participants attended only
face-to-face consultations at other SOPCs. Both groups of participants filled in the C-GHQ-12
within 7 days before the consultation and again within 7 days after the
consultation. In addition, the intervention participants filled in the
satisfaction survey questionnaire after the psychiatric teleconsultation.
Any major adverse events, such as medical or psychiatric emergencies, were
recorded.
Statistical analysis
Descriptive statistics were used to analyse the
baseline profile of the participants’ socio-demographic and clinical
characteristics as well as pre- and post-consultation C-GHQ-12 scores and
satisfaction survey questionnaire responses. Chi squared test and
two-samples t test were performed to assess if there were
differences in the baseline characteristics between the intervention and
control participants. A non-parametric Mann-Whitney U test was
performed to test if there were differences in the pre-post difference in
C-GHQ-12 score between intervention and control participants attending
their first consultation. Spearman’s correlation was used to compute the
correlation between the pre-post difference in C-GHQ-12 score of the first
and second teleconsultations among the intervention participants. All
statistical analyses were conducted using SPSS for Windows, version 12.0
(SPSS Inc, Chicago [IL], US), with P<0.05 considered as statistically
significant in this study.
Results
During the study period, there were 377 PIC
scheduled attendances at CPH. Of these, 221 PIC scheduled attendances were
suitable for psychiatric teleconsultation; however, for 49 of the suitable
PIC scheduled attendances, the PICs refused to give consent for this
study. Finally, 172 PIC psychiatric teleconsultation attendances were
included. Each participant could have more than one psychiatric
teleconsultation attendance during the study period. Therefore, 86
participants aged 21 to 64 years who were stable Chinese male psychiatric
out-patients and who fulfilled the inclusion and exclusion criteria for
psychiatric teleconsultations in CPH were included. For the control group,
249 male patients within the same age range (21-64 years) were recruited.
Table 2 compares patient characteristics between the
intervention and control groups. There were no significant differences in
the age and education profile between the two groups. The mean age of both
groups was approximately 40 years. Approximately three quarters of the
participants in each group had attained education at the secondary level
or above. There was a significant difference in the principal psychiatric
diagnosis (P=0.029). Slightly over 50% of each group were diagnosed as
substance abuse. A larger proportion of intervention participants had
schizophrenia (28%) than did the control participants (16%). There were no
significant differences in the mean pre-consultation C-GHQ-12 score
between the two groups.
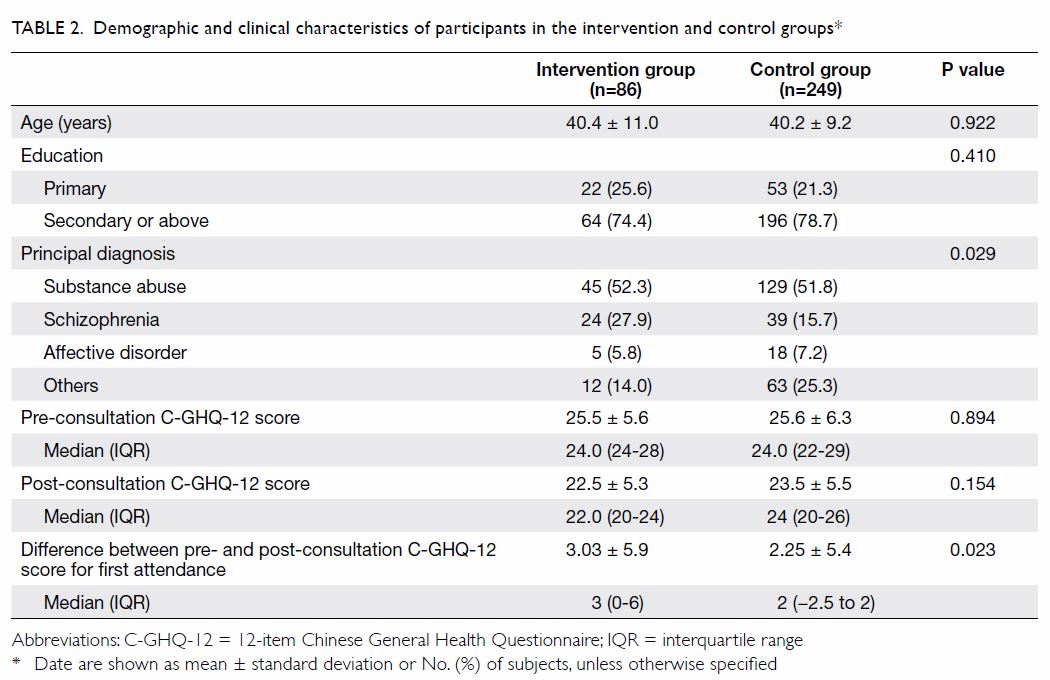
Table 2. Demographic and clinical characteristics of participants in the intervention and control groups*
The mean (standard deviation) on-air time duration
of the psychiatric teleconsultations was 6.33 (3.58) minutes. There were
no significant adverse events associated with teleconsultations reported
during the study. The pre-post difference in C-GHQ-12 score of the
intervention participants was significantly higher than that of the
control participants (P=0.023; Table 2). Furthermore, among 29 intervention
participants who had at least two teleconsultations, the association
between pre-post difference in C-GHQ-12 score of the first and second
teleconsultations was moderately strong (r=0.309, P=0.103) but did
not reach the level of significance set for this study. The possible scores on the satisfaction survey
questionnaire ranged from 9 (the most satisfied) to 45 (the least
satisfied). The mean (standard deviation) satisfaction score of the
intervention group was 16.48 (4.35). No major adverse events were reported
throughout the study.
Discussion
Telepsychiatry is not a new development in Hong
Kong. Since 2001, the use of telepsychiatry has been shown to increase
access to care.11 Studies have
shown that telepsychiatry is an effective means to provide psychogeriatric
services to residents of care homes,11
and cognitive intervention for community-dwelling elderly patients with
memory problems.12 This was the first intervention pilot study in Hong Kong exploring the effect of psychiatric teleconsultation for Chinese
psychiatric out-patients under the legal custody of the CSD. Our study
compared the effectiveness of psychiatric teleconsultations with that of
face-to-face consultations among PIC receiving out-patient psychiatric
treatment. The two groups of stable Chinese male out-patient participants
had the same baseline characteristics in age, education level, and
pre-consultation C-GHQ-12 score. The results showed that the standard of
care of teleconsultations was comparable to that of face-to-face
consultations. The pre-post difference in C-GHQ-12 score for
teleconsultations had a marginally larger positive increase than did
face-to-face consultations. The intervention participants also showed high
satisfaction with the psychiatric teleconsultation service, with a mean
satisfaction score above the 80th percentile. This results is similar to
that of a previous study in the US that compared the effectiveness of
telepsychiatry and in-person psychiatry sessions among 71 parolees over a
6-month follow-up period, revealing high satisfaction with telepsychiatry
treatment.13 In the present study,
the pre-post difference between C-GHQ-12 score of the first and second
psychiatric teleconsultations showed a moderate positive relationship,
suggesting a consistent and sustainable clinical effect of telepsychiatry
between sessions. Importantly, there were no reports of significant
adverse events. Therefore, telepsychiatry can be considered sustainable
and safe for Chinese PIC in Hong Kong.
Studies on the effects of telepsychiatry for
incarcerated populations are relatively scarce; however, the results of
our study are also consistent with studies of telepsychiatry in
populations that were not involved with the correctional system. In a
randomised controlled study in Canada, 495 patients were assigned at
random to be examined face-to-face or by telepsychiatry.14 Psychiatric consultations and follow-ups delivered by
telepsychiatry produced clinical outcomes equivalent to those achieved
when the service was provided face-to-face.14
This result suggests that psychiatric consultation and short-term
follow-up can be as effective when delivered by telepsychiatry as when
provided face-to-face. Another study evaluating the effectiveness of
telepsychiatry in relation to cognitive changes in patients with dementia
revealed that changes in the Mini-Mental State Examination score were not
significantly different between patients receiving teleconsultations and
those receiving clinic-based face-to-face consultations.15 This finding suggest that telepsychiatry may be a
useful alternative to face-to-face clinical visits for treatment of a wide
range of patient groups, including patients with dementia. Research has
shown that there is an association between dementia and criminal offences
and that the use of telepsychiatry might be extended to PIC with dementia
in Hong Kong.16
Our study has several limitations. First, the
sample size of the intervention group was small. Most enrolled patients
served short sentences but had long follow-up intervals, because we
recruited stable patients. Although the study duration was 2 years, only
29 out of 86 intervention participants had at least two psychiatric
teleconsultations for comparison within the intervention group. Second,
recruitment of potential telepsychiatry participants was limited to stable
Chinese male psychiatric out-patients. Therefore, the sample may be
affected by self-selection bias, because PICs volunteered to participate
in telepsychiatry. This restricted sample also limits the generalisability
of the results. Third, the mean time between the consultation and
completion of the C-GHQ-12 was not recorded for intervention or control
groups. Differences in this time interval may affect the pre-post
difference in C-GHQ-12 score for the groups. We also did not collect data
on the follow-up interval between the first and second psychiatric
teleconsultations for the intervention group. This follow-up interval may
affect the C-GHQ-12 score and the satisfaction on psychiatric
teleconsultation. Fourth, the mean on-air time duration of psychiatric
teleconsultations was 6.33 minutes; however, we did not measure the
duration of face-to-face consultations for comparison between the two
groups. The duration of consultation may have an effect on the outcome
scores and patient satisfaction. Last, the study lacked robust clinical
outcome measures and the satisfactory questionnaire adopted in this study
had not been validated. Despite the limitations of this study, the results
suggest that psychiatric teleconsultations are a sustainable and safe
alternative to face-to-face consultations for stable Chinese male
psychiatric out-patients in custody. The use of psychiatric
teleconsultations has potential in other populations of PICs, such as
female PICs or elderly PICs, but further research is required to
investigate psychiatric teleconsultations for these populations.
Further research is required to examine the full
potential of telepsychiatry among PICs in Hong Kong. In future studies,
female patients should be recruited, to assess any sex-based differences.
In addition, the scale of future studies using telepsychiatry can be
increased by setting up more stations at CSD institutions and at other
SOPCs in the Hospital Authority. Clinical outcomes such as symptom
severity and psychological functioning of the patients could be assessed.
Given the increasing number of older PICs in Hong Kong, recruitment of
older patients could be considered for further study. It would be
worthwhile to perform a future study with a larger sample size and with
participants receiving a greater number of psychiatric teleconsultations,
in order to further support the sustainability of psychiatric
teleconsultations.
A cost analysis for psychiatric teleconsultation
was beyond the scope of the present study. However, a systematic review of
137 telemedicine services in hospital facilities revealed that one of the
key reasons for introducing telemedicine was cost reduction.17 Similar cost-saving conclusions have been reported in
two studies in Hong Kong related to dementia and community geriatric
services.11 12 In future studies, cost analysis of psychiatric
teleconsultation including direct, indirect, and hidden costs could be
calculated for further exploring the effectiveness of psychiatric
teleconsultation.
Conclusions
Telepsychiatry appears to be an acceptable approach
for providing out-patient psychiatric care for stable Chinese male PICs in
Hong Kong. Telepsychiatry can be considered a sustainable and safe
alternative to face-to-face consultations, with a comparable standard of
care. Moreover, the intrinsic problems of embarrassment and stigmatisation
caused to PICs, the risk that PICs might abscond, and the safety of the
general public are all addressed by this promising alternative mode of
psychiatric care for stable Chinese male PICs. Telepsychiatry is likely to
show similar benefits for Chinese female PICs and PICs in other age-groups, such as older adults, but further research is required to confirm
this.
Author contributions
All authors have made substantial contributions to
the concept and design, acquisition of data, analysis and interpretation
of data, drafting and critical revision for important intellectual content
of the article.
Acknowledgement
We would like to acknowledge Dr CK Tung, Dr CF
Tsui, Mr KW Chung, Mr Kenny Wong, Dr NM Kwong, and all the mental health
professionals and CSD staff who have assisted in the design and
implementation of this study. We would also like to acknowledge the study
participants who had kindly participated in the present study.
Funding/support
This research received no specific grant from any
funding agency in the public, commercial, or not-for-profit sectors.
Declaration
All authors have disclosed no conflicts of
interest. All authors had full access to the data, contributed to the
study, approved the final version for publication, and take responsibility
for its accuracy and integrity. The research was presented in part in the
Hospital Authority Convention 2017, 16 May 2017, Hong Kong.
Ethical approval
Approval for conducting the study was granted by
the Research and Ethics Committee of the New Territories West Cluster of
the Hospital Authority and the Research and Ethics Committee of the
Correctional Services Department. The principles outlined in the
Declaration of Helsinki were followed in the conduction of this study.
References
1. Gray LC, Edirippulige S, Smith AC, et
al. Telehealth for nursing homes: the utilization of specialist services
for residential care. J Telemed Telecare 2012;18:142-6. Crossref
2. Grady B, Myers KM, Nelson EL, et al.
Evidence-based practice for telemental health. Telemed e-Health
2011;17:131-48. Crossref
3. WHO Global Observatory for eHealth.
2010. Telemedicine: opportunities and developments in Member States:
report on the second global survey on eHealth. Geneva: World Health
Organization. Available from: http://www.who.int/iris/handle/10665/44497.
Accessed 1 Jan 2018.
4. McLaren P. Telemedicine and telecare:
what can it offer mental health services? Adv Psychiatr Treat
2003;9:54-61. Crossref
5. Telemedicine can Reduce Correctional
Health Care Costs: An Evaluation of a Prison Telemedicine Network. US
Department of Justice; 1999.
6. Hjelm NM. Telemedicine: academic and
professional aspects. Hong Kong Med J 1998;4:289-92.
7. International Statistical Classification
of Diseases and Related Health Problems, 10th revision. Geneva, World
Health Organization; 1992.
8. Chan DW. The Chinese version of the
General Health Questionnaire: does language make a difference? Psychol Med
1985;15:147-55. Crossref
9. Goldberg DP. The Detection of
Psychiatric Illness by Questionnaire. London: Oxford University Press;
1972.
10. Goldberg D, Williams P. A User’s Guide
to the General Health Questionnaire. London: NFER; 1988.
11. Tang WK, Chiu H, Woo J, Hjelm M, Hui
E. Telepsychiatry in psychogeriatric service: a pilot study. Int J Geriatr
Psychiatry 2001;16:88-93. Crossref
12. Poon P, Hui E, Dai D, Kwok T, Woo J.
Cognitive intervention for community-dwelling older persons with memory
problems: telemedicine versus face-to-face treatment. Int J Geriatr
Psychiatry 2005;20:285-6. Crossref
13. Farabee D, Calhoun S, Veliz R. An
experimental comparison of telepsychiatry and conventional psychiatry for
parolees. Psychiatr Serv 2016;67:562-5. Crossref
14. O’Reilly R, Bishop J, Maddox K,
Hutchinson L, Fisman M, Takhar J. Is telepsychiatry equivalent to
face-to-face psychiatry? Results from a randomized controlled equivalence
trial. Psychiatr Serv 2007;58:836-43. Crossref
15. Kim H, Jhoo JH, Jang JW. The effect of
telemedicine on cognitive decline in patients with dementia. J Telemed
Telecare 2017;23:149-54. Crossref
16. Liljegren M, Naasan G, Temlett J, et
al. Criminal behavior in frontotemporal dementia and Alzheimer disease.
JAMA Neurol 2015;72:295-300. Crossref
17. AlDossary S, Martin-Khan MG, Bradford
NK, Smith AC. A systematic review of the methodologies used to evaluate
telemedicine service initiatives in hospital facilities. Int J Med Inform
2017;97:171-94. Crossref