Hong
Kong Med J 2018 Aug;24(4):335–9 | Epub 30 Jul 2018
DOI: 10.12809/hkmj177025
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE
Ambulance use affects timely emergency treatment of
acute ischaemic stroke
KK Lau, FRACP, FHKAM (Medicine)1; Ellen
LM Yu, BSc (Stat & Fin), MSc (Epi & Biostat)2; MF Lee,
BS (Nursing), MSc1; SH Ho, BS (Nursing)1; PM Ng, BS
(Nursing), MSc1; CS Leung, FHKCEM, FHKAM (Emergency Medicine)3
1 Department of Medicine and Geriatrics,
Princess Margaret Hospital, Laichikok, Hong Kong
2 Clinical Research Centre, Princess
Margaret Hospital, Laichikok, Hong Kong
3 Accident and Emergency Department,
Princess Margaret Hospital, Laichikok, Hong Kong
Corresponding author: Dr KK Lau (laukk2@ha.org.hk)
Abstract
Introduction: For acute
ischaemic stroke patients, treatment with intravenous tissue plasminogen
activator within a 4.5-hour therapeutic window is essential. We aimed to
assess the time delays experienced by stroke patients arriving at the
emergency department and to compare ambulance users and non-ambulance
users.
Methods: We performed a
prospective cohort study in a tertiary hospital in Hong Kong. All acute
stroke patients attending the emergency department from January to June
2017 were recruited. Patients who were in hospital at the time of stroke
onset and those who transferred from other hospitals were excluded.
Three phases were compared between ambulance users and non-ambulance
users: phase I, between stroke onset and calling for help; phase II,
between calling for help and arriving at the emergency department; and
phase III, between arriving and receiving medical assessment.
Results: Of 102 consecutive
patients recruited, 48 (47%) patients arrived at the emergency
department by ambulance. The percentage of stroke patients attending
emergency department within the therapeutic window was significantly
higher for ambulance users than for non-ambulance users (64.6% vs 29.6%;
P<0.001). For phases I, II and III, the median times were
significantly shorter for ambulance users (77.5, 32 and 8 min,
respectively) than for non-ambulance users (720, 44.5 and 15 min,
respectively; all P<0.001).
Conclusion: Transport of
patients to the emergency department by ambulance is important for
timely and effective stroke treatment.
New knowledge added by this study
- Significantly more ambulance users received medical consultation at the emergency department within the therapeutic window than non-ambulance users.
- Time intervals between stroke onset, help seeking, arrival at the emergency department and medical consultation were significantly shorter for ambulance users than for non-ambulance users.
- Non-ambulance users who had visited a general practitioner arrived at the emergency department significantly later than ambulance users after seeking help; those who did not visit a general practitioner were not significantly different from ambulance users.
- The public should be educated to promptly call the emergency services after stroke onset.
Introduction
Treatment for acute ischaemic stroke by intravenous
tissue plasminogen activator (TPA) was introduced in 1995.1 Early attendance is essential, as the effectiveness of
TPA has been shown to decrease over time.2
3 Stroke patients are recommended
to receive TPA within 4.5 hours after stroke onset.1 2 In Hong Kong,
TPA has been available since early 2010. It typically takes 1 hour to
complete the necessary examination, blood tests, brain computed
tomographic scan, and preparation of TPA for administration. Therefore,
stroke patients should receive a medical consultation at an emergency
department (ED) within the therapeutic window of 3.5 hours after onset. In
1999, a study in Hong Kong investigated how patients attended EDs after
stroke.4 At that time, stroke was
classified as category II, and patients were not treated as urgent.
Therefore, such stroke patients were often seen several hours after
arrival. The study suggested that stroke should be treated as category I,
and that immediate treatment should be given.4
Public education on recognising the signs and symptoms of stroke was also
recommended.4 A collective effort
at the social and administrative levels, aimed at shortening the duration
between onset and arrival has been proposed.5
The aim of the present study was to investigate stroke patients’ means of
transportation to the ED after stroke. The percentage of stroke patients
receiving medical consultation at the ED within the therapeutic window was
compared between ambulance users and non-ambulance users.
Methods
This was a prospective cohort study conducted by
the Accident and Emergency Department and the Department of Medicine and
Geriatrics, Princess Margaret Hospital, Hong Kong. All stroke patients
admitted to the acute stroke unit via the ED from 1 January 2017 to 30
June 2017 were included. Patients who were in hospital at the time of
stroke onset, or who transferred from other hospitals were excluded.
Patients were invited to join this study after receiving stroke treatment,
including TPA when applicable. Stroke patients were divided into two
groups: ambulance users who called the emergency services and were brought
to hospital by emergency ambulance; and non-ambulance users who sought
alternate help and attended by other means of transportation.
Non-ambulance users were further divided into those who visited a general
practitioner (GP) before attending the ED, and those who did not. The
onset time, arrival time, and time of medical consultation in the ED were
collected from patient interviews and electronic admission records. The
collected data were cross-checked by relatives or a GP. Three time
intervals were studied: phase I was between stroke onset and calling for
help (calling the emergency services for ambulance users or other calls
for help for non-ambulance users); phase II was between calling for help
and arriving at the ED; and phase III was between arriving at the ED and
receiving medical consultation. The percentage of stroke patients
receiving a medical consultation within the therapeutic window (210
minutes from stroke onset) was compared between ambulance users and
non-ambulance users using Pearson’s Chi squared test. The time intervals of the three
phases were reported as median (interquartile range) and were compared
between the two groups using the Mann-Whitney U test.
Results
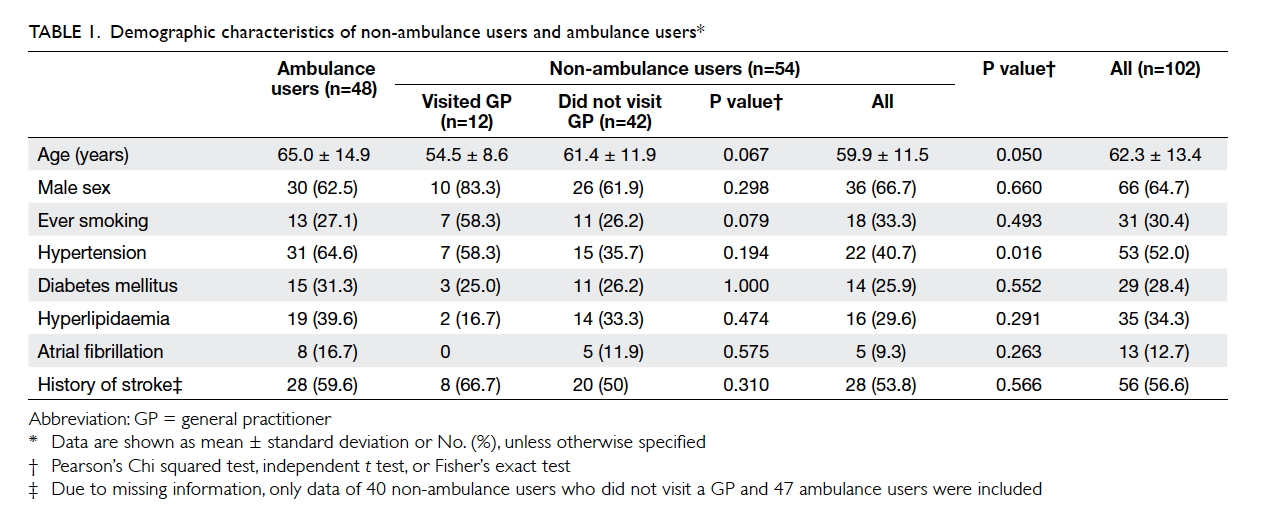
A total of 102 patients were eligible and were
consecutively recruited. Of these patients, 48 (47.1%) were brought to the
ED by ambulance. Patient demographic data, including age, sex, and
co-morbidities are presented and compared between ambulance users and
non-ambulance users in Table 1. No statistical difference was found between
the two groups except hypertension (P=0.016).
The proportion of stroke patients arriving within
the therapeutic window was significantly higher in ambulance users (64.6%;
31/48) than that in non-ambulance users (29.6%; 16/54) [P<0.001]. Of
the 12 non-ambulance users who visited a GP before going to the ED, only
one (8.3%) arrived within the therapeutic window, compared with 15 out of
42 (35.7%) patients from the non-ambulance user group.
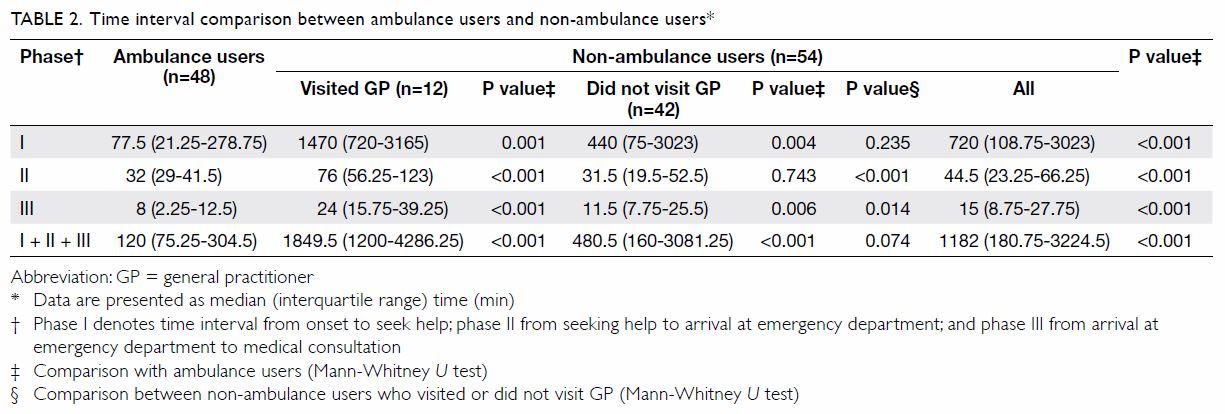
Table 2 shows the comparison of the different time
intervals between ambulance users and non-ambulance users. There were
significant differences between the two groups for all phases
(P<0.001). The median time for phase I for ambulance users was 77.5
minutes, whereas for non-ambulance users it was 720 minutes. The
non-ambulance user group, whether the patient visited a GP or not, had a
longer phase I interval than the ambulance user group (1470 [720-3165] min;
P=0.001 for those who visited a GP and 440 [75-3023] min; P=0.004 for those who did
not visit a GP). For phase II, the median travel time for ambulance users (32 min)
was significantly shorter than that for non-ambulance users (44.5 min)
[P<0.001]. Compared with ambulance users, non-ambulance users who had
visited a GP had a significantly longer travel time (76 [56.25-123] min;
P<0.001), whereas the travel time for those who did not visit a GP was
not significantly different (31.5 [19.5-52.5] min; P=0.743). After arrival
at the ED, the time to medical consultation for ambulance users was 8
minutes and that for non-ambulance users was 15 minutes (P<0.001). The
time from onset of stroke to medical consultation in the ED for ambulance
users was 120 minutes, whereas that for non-ambulance users was 1182
minutes (P<0.001).
Of the 102 patients, 34 patients were treated with
TPA. The reasons for not giving TPA were: uncertain onset time (n=8),
therapeutic window exceeded (n=13), low National Institutes of Health
Stroke Scale (NIHSS) score of <5 (n=52), high NIHSS score of >25
(n=16), intracerebral haemorrhage (n=16), convulsions (n=2), patient
refused TPA (n=2), and poor pre-morbidity (n=6). There may be more than
one reason per patient for not giving TPA. At 3 months after
administration of TPA, five patients had excellent results (ie, reduction
of ≥8 points in NIHSS score), 11 had good results (ie, reduction of ≥4
points in NIHSS score), 14 were static (ie, change of <4 points in
NIHSS score), and four deteriorated (ie, increase of ≥4 points in NIHSS
score).
Discussion
In Hong Kong, calls to the emergency services are
answered by the Police Force and the Fire Services Department, which
provides ambulance and fire-fighting services. Our study found that
overall time intervals were shorter in ambulance users than in
non-ambulance users. Significantly more ambulance users had a medical
consultation within the therapeutic window than did non-ambulance users.
For phase I, ambulance users might have more awareness and called for help
earlier than the non-ambulance users. Compared with ambulance users, phase
II was significantly longer for non-ambulance users who visited a GP, but
not for patients who did not visit a GP. This might be because
non-ambulance users who did not visit a GP went directly to the ED after
calling for help. Ambulance users had a shorter phase III than did
non-ambulance users. Non-ambulance users who did not visit a GP had
shorter phase II, phase III, and overall time from onset to medical
consultation than did those who visited a GP.
A study in Australia showed that fewer than 50% of
stroke patients who called for an ambulance could correctly identify
stroke from the symptoms.6 A study
in Germany on calling for emergency assistance showed similar findings.7 An important finding in these
papers was the importance of advice and assistance immediately after
stroke onset6 7; one third of these patients were unable to make
decision themselves.6 How stroke
patients interpreted their symptoms, developed coping mechanisms, and
engaged others prior to an emergency call for help was unclear.6 The process of seeking “lay referral” to call for an
ambulance was not studied.6
In North America, a study to compare hospital
arrivals showed no major differences between the situation in 2002 and
that in 2009.8 The Get With The
Guidelines–Stroke Program included over 413 147 ischaemic stroke patients
from 287 hospitals; of these, 26.8% of patients arrived at the ED in ≤3.5
hours. The percentage of stroke patients who arrived within the
therapeutic window did not change during the studied period. The authors
suggested that further effort would be necessary to increase the
proportion of patients arriving within the therapeutic window.8
Our findings are important for clinical
applications. In our literature search, we could not find study from Hong
Kong on how to shorten the time prior to hospital arrival. We believe that
appropriate education can change the mindset of the public. If patients
can recognise the signs and symptoms of stroke, they are more likely to
call an ambulance in a timely manner, and thus will have a higher chance
of receiving TPA treatment within the therapeutic window.
There are several limitations to the present study.
The study was conducted in a single centre within a 6-month period.
Although the sample size was limited by the study period, significant
results were found. The study involved asking patients to recall the time
of stroke onset, time of calling for help, and time of arrival at the ED.
To mitigate any potential recall bias, the recalled information was
cross-checked by relatives or a GP, and the time interval was short.
In recent years, the Hong Kong Stroke Fund has
provided much public education, promoting recognition of acute stroke
using the mnemonic “FAST” (談笑用兵). Here, “F” (face, 笑) refers to facial
asymmetry, “A” (arms, 用) refers to weakness or numbness of the limbs, “S”
(speech, 談) refers to slurring of speech, and “T” (time, 兵) refers to
calling for immediate assistance.9
A study in Japan compared the effectiveness of
different media on how to improve public knowledge of stroke. The authors
found that television was more effective than printed newspapers.10 A combination of different media was found to be most
effective.10 Structured
community-based public education can improve public knowledge on stroke.10
Some patients voluntarily mentioned their reasons
for not calling the emergency services for an ambulance. Some years ago,
there was a publicity campaign to reduce ambulance misuse.11 Although the original message was not to misuse the
ambulance service, the effect was long-lasting. Some patients still
believe that there is always someone who is in greater need of an
ambulance. Thus, these patients believe that they can travel to the ED
themselves and are unaware of the urgency. Because these patients are
unaware of the therapeutic window, they do not hurry to the ED. Public
education, especially to encourage proper use of ambulance services is
required.12 Public education on
recognition of the symptoms and signs of stroke and on how to better
utilise the emergency services is of the utmost importance.
Conclusion
The present study shows that the means of transport
to the ED is an important aspect in effective stroke treatment. Stroke
patients who call the emergency services are more likely to be treated
effectively with TPA within the therapeutic window. Increasing public
awareness of the signs and symptoms of acute stroke, and of the need to
call the emergency services in case of stroke is critical.
Acknowledgement
Thanks to all patients and their relatives, without
their support this study could not be completed.
Author contributions
All authors have made substantial contributions in
designing the study, collecting data, analysis and interpretation of data,
drafting, and critical revision of the article.
Funding/support
This research has received no specific grant from
any funding agency in the public, commercial, or not-for-profit sectors.
Declaration
All authors have disclosed no conflict of interest.
All authors had full access to the data, contributed to the study,
approved the final version for publication, and take responsibility for
its accuracy and integrity.
Ethical approval
This study was approved by the Ethics Committee,
Kowloon West Cluster (REC no. KW/EX-16-183(105-10)). Written informed
consent was provided by all patients.
References
1. National Institute of Neurological
Disorders and Stroke rt-PA Stroke Study Group. Tissue plasminogen
activator for acute ischemic stroke. N Engl J Med 1995;333:1581-7. Crossref
2. Hacke W, Donnan G, Fieschi C, et al.
Association of outcome with early stroke treatment: pooled analysis of
ATLANTIS, ECASS, and NINDS rt-PA stroke trials. Lancet 2004;363:768-74. Crossref
3. Strbian D, Ringleb P, Michel P, et al.
Ultra-early intravenous stroke thrombolysis: do all patients benefit
similarly? Stroke 2013;44:2913-6. Crossref
4. Lau KK, Yeung KM, Chiu LH, et al. Delays
in the presentation of stroke patients to hospital and possible ways of
improvement. Hong Kong J Emerg Med 2003;10:76-80. Crossref
5. Hachinski V, Donnan GA, Gorelick PB, et
al. Stroke: working toward a prioritized world agenda. Cerebrovasc Dis
2010;30:127-47. Crossref
6. Mosley I, Nicol M, Donnan G, Patrick I,
Dewey H. Stroke symptoms and the decision to call for an ambulance. Stroke
2007;38:361-6. Crossref
7. Handschu R, Poppe R, Rauss J, Neundörfer
B, Erbguth F. Emergency calls in acute stroke. Stroke 2003;34:1005-9. Crossref
8. Tong D, Reeves MJ, Hernandez AF, et al.
Times from symptom onset to hospital arrival in the Get With the
Guidelines–Stroke Program 2002 to 2009: temporal trends and implications.
Stroke 2012;43:1912-7. Crossref
9. Hong Kong Stroke Fund. Acute Stroke
Management— FAST. 2017. Available from:
http://www.strokefund.org/eng/prevention_part1.php. Accessed 22 Sep 2017.
10. Miyamatsu N, Okamura T, Nakayama H, et
al. Public awareness of early symptoms of stroke and information sources
about stroke among the general Japanese population: the acquisition of
stroke knowledge study. Cerebrovasc Dis 2013;35:241-9. Crossref
11. Hong Kong’s Information Services
Department.「切勿濫用救護車」標語創作比賽. 2009. Available from:
http://www.info.gov.hk/gia/general/200906/16/P200906160205.htm. Accessed
22 Sep 2017.
12. Becker K, Fruin M, Gooding T,
Tirschwell D, Love P, Mankowski T. Community-based education improves
stroke knowledge. Cerebrovasc Dis 2001;11:34-43. Crossref