Hong Kong Med J 2018 Jun;24(3):238–44 | Epub 21 May 2018
DOI: 10.12809/hkmj177039
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE
Hypospadias surgery in children: improved service model
of enhanced recovery pathway and dedicated surgical team
YS Wong, FHKAM (Surgery); Kristine KY Pang, FHKAM
(Surgery); YH Tam, FHKAM (Surgery)
Division of Paediatric Surgery and Paediatric
Urology, Department of Surgery, Prince of Wales Hospital, The Chinese
University of Hong Kong, Shatin, Hong Kong
Corresponding author: Dr YH Tam (pyhtam@surgery.cuhk.edu.hk)
Abstract
Introduction: Children in Hong
Kong are generally hospitalised for 1 to 2 weeks after hypospadias
repairs. In July 2013, we introduced a new service model that featured
an enhanced recovery pathway and a dedicated surgical team responsible
for all perioperative services. In this study, we investigated the
outcomes of hypospadias repair after the introduction of the new service
model.
Methods: We conducted a
retrospective study on consecutive children who underwent primary
hypospadias repair from January 2006 to August 2016, comparing patients
under the old service with those under the new service. Outcome measures
included early morbidity, operative success, and completion of enhanced
recovery pathway.
Results: The old service and new
service cohorts comprised 176 and 126 cases, respectively. There was no
difference between the two cohorts in types of hypospadias and surgical
procedures performed. The median hospital stay was 2 days in the new
service cohort compared with 10 days in the old service cohort
(P<0.001). Patients experienced less early morbidity (5.6% vs 15.9%;
P=0.006) and had a lower operative failure rate (20.2% vs 44.2%;
P<0.001) under the new service than the old service. Multivariable
analysis revealed that the new service significantly reduced the odds of
early morbidity (odds ratio=0.35, 95% confidence interval=0.15-0.85;
P=0.02) and operative failure (odds ratio=0.32, 95% confidence
interval=0.17-0.59; P<0.001) in comparison with the old service. Of
the new service cohort, 111(88.1%) patients successfully completed the
enhanced recovery pathway.
Conclusions: The enhanced
recovery pathway can be implemented safely and effectively to primary
hypospadias repair. A dedicated surgical team may play an important role
in successful implementation of the enhanced recovery pathway and
optimisation of surgical outcomes.
New knowledge added by this study
- Children can be discharged early from hospital after primary hypospadias repairs, regardless of the severity of the hypospadias and the surgical techniques used.
- Improved operative success of hypospadias repair may be achieved by dedicated hypospadias surgeons.
- Primary hypospadias repair in children can be considered as short-stay surgery.
- Tertiary centres for hypospadias may consider concentration of hypospadias repairs among a few dedicated surgeons.
Introduction
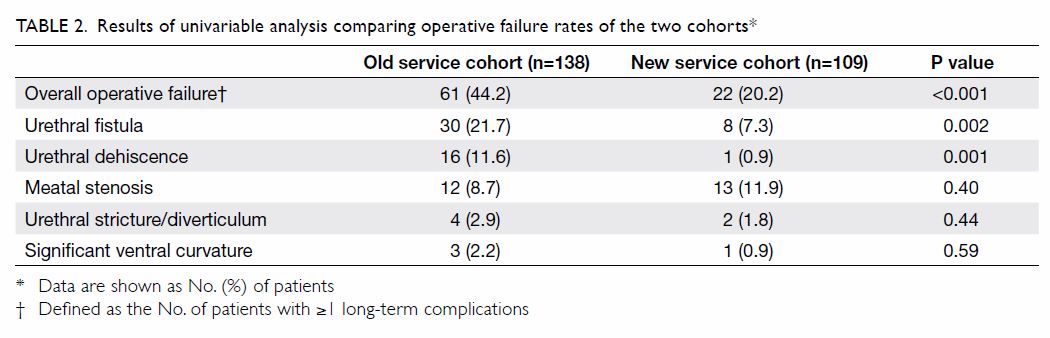
Hypospadias is a congenital abnormality of the
external genitalia in boys, and is defined as an arrest in the
embryological development of the urethra, foreskin, and ventral aspect of
the penis.1 Hypospadias is
characterised by abnormal foreskin with a dorsal hood and an ectopic
urethral meatus, which can be located anywhere from the ventral aspect of
the glans penis, along the penile shaft, within the scrotum, to the
perineum (Fig 1). Hypospadias can be classified broadly into
distal, mid-shaft, or proximal types, with the proximal type being the
most severe form. In general, more severe forms of hypospadias are
associated with a higher incidence and severity of penile ventral
curvature (chordee).1
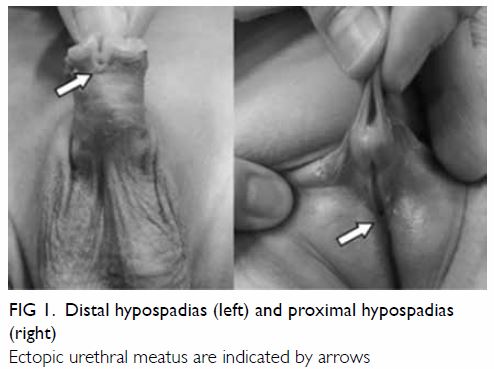
Figure 1. Distal hypospadias (left) and proximal hypospadias (right)
Ectopic urethral meatus are indicated by arrows
Hypospadias repair is generally recommended in
early childhood for improved function and cosmesis.2 Although advances in surgical techniques have resulted
in favourable outcomes with high success rates for distal hypospadias
repair,3 proximal hypospadias
repair remains challenging, and complication rates have been
reported to be as high as over 50%.4
Postoperatively, the urethral catheter is usually left in place for free
drainage for 5 to 7 days in distal repair5
and from 10 to 14 days in proximal repair.6
In many parts of the world, including North America, patients generally
have a very short stay in hospital and are discharged home with urethral
catheters in situ.7 In contrast,
conventional practice in Hong Kong has been to provide in-patient care
after hypospadias surgery until removal of the urethral catheter.
The Division of Paediatric Surgery and Paediatric
Urology at the Prince of Wales Hospital has been a tertiary referral
centre for hypospadias surgery for over two decades. We introduced a new
service (NS) model in July 2013, which featured the establishment of a
dedicated surgical team and the implementation of an enhanced recovery
pathway (ERP). The present study aimed to compare the outcomes of the NS
model with those of the old service (OS) model. We hypothesised that ERP
implementation by a dedicated surgical team would reduce the risk of early
morbidity and increase the operative success of hypospadias repair.
Methods
Patients
A historical cohort study was conducted on
consecutive patients younger than 18 years who underwent primary repair of
hypospadias in our centre from January 2006 to August 2016. The patients
were identified using both the ICD-10 (International Classification of
Diseases, 10th revision) code related to hypospadias surgery and the
registry of operative procedures entry in operating theatres. We used
ICD-10 code 752.61, which covered the diagnosis of various types of
hypospadias, as well as codes 58.45 and 58.46, which covered various
techniques of hypospadias repairs. The patients underwent either one-stage
tubularised incised plate (TIP) repair5
8 (Fig 2), or two-stage preputial flap repair9 (Fig 3), as these two techniques had been our
standard practice for primary repair of hypospadias from distal to
proximal types during the study period. We excluded reoperative
hypospadias repairs and repairs with buccal mucosal graft (BMG).
Reoperative hypospadias surgery is highly variable in complexity, involves
multiple surgical techniques, and is usually investigated separately from
primary hypospadias surgery in literature. Children who undergo BMG
harvest are generally not considered suitable for early hospital
discharge. Moreover, BMG is used rarely in hypospadias surgery, and only
under special circumstances. We also excluded minor hypospadias repairs by
meatal advancement with glansplasty or meatoplasty alone, as such
procedures did not require prolonged urethral catheterisation.
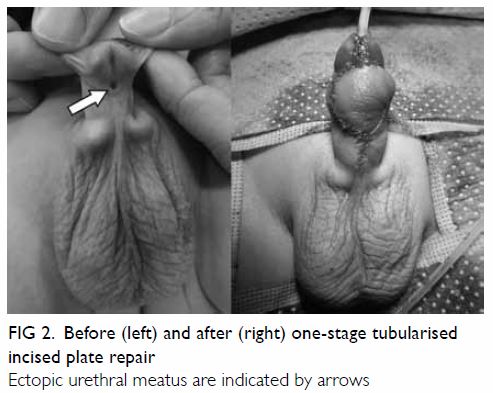
Figure 2. Before (left) and after (right) one-stage tubularised incised plate repair
Ectopic urethral meatus are indicated by arrows
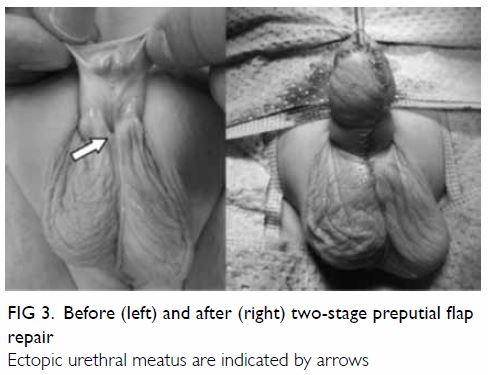
Figure 3. Before (left) and after (right) two-stage preputial flap repair
Ectopic urethral meatus are indicated by arrows
New service model versus old service model
In this study, we assigned patients to two cohorts.
The OS cohort was the control cohort comprising patients on whom we
operated from January 2006 to June 2013. All the patients in this cohort
remained as in-patients until removal of the urethral catheter and
received intravenous antibiotics and regular wound care by medical staff
in the postoperative period. Six specialist paediatric surgeons were
involved in performing the repairs in the OS cohort. The NS cohort
comprised patients who underwent surgery in July 2013 or thereafter.
Patients in the NS cohort were routinely discharged on postoperative day 2
or, rarely, on postoperative day 3, with their urethral catheters in situ.
The dedicated surgical team comprising three (initially only two)
specialist paediatric surgeons who subspecialised in paediatric urology
provided all perioperative services, including handling of the consent
process, surgical repairs, postoperative demonstration of wound care, and
explanation of the discharge plan. Parents or main caregivers were
instructed to perform saline irrigation to the penile wound at home 3 to 4
times per day. Patients received oral antibiotics and were scheduled to
return in a day visit for removal of urethral catheters by a member of the
dedicated team. Parents were instructed to call the ward to arrange an
unplanned consultation visit if necessary. After urethral catheter
removal, patients were followed up at 2 to 4 weeks, 3 months, 6 to 9
months, and then yearly thereafter.
Outcome measures
Medical records were retrospectively reviewed and
data were collected by the authors, who were not blinded to the type of
service model. Data collected were age at time of surgery, type of
hypospadias, type of surgical repair, early morbidity, length of hospital
stay (LOS), unplanned hospital visits, and follow-up evaluation for
long-term complications. Data on the types of hypospadias and surgical
techniques were based on the operative findings and surgical procedures
documented in the operative records. The presence of any early morbidity
was based on investigation results (including urine/wound swab culture)
and/or documentations of urethral catheter dislodgement, wound bleeding,
or wound gaping in the early postoperative period when the urethral
catheter was in situ. The presence of any long-term complications was
based on the findings in the latest follow-up visit, or any
reintervention/reoperation records subsequent to the primary surgery. When
collecting data, we tried to minimise potential bias regarding long-term
complications by defining such complications as meatal stenosis,
neourethra dehiscence, urethral fistula, urethral stricture or
diverticulum, and significant recurrent chordee. All of these long-term
complications required re-intervention/reoperation and were documented if
present.
Primary outcomes of interest were early morbidity
and operative failure. Early morbidity was defined by the presence of one
or more of the following conditions when the urethral catheter was still
in situ: urinary tract infection, catheter dislodgement, and wound-related
events (bleeding/infection/gaping). In the OS cohort, early morbidity was
detected during the hospitalisation period after hypospadias repair. In
the NS cohort, early morbidity was detected at the time of urethral
catheter removal or during unplanned hospital visits before the scheduled
date of urethral catheter removal.
Successful or failed repair was determined during
follow-up in those who had undergone TIP repair or had completed both
stages of the two-stage repair. Operative failure was defined as the
development of one or more of the long-term complications that required
reoperation or reintervention. The secondary outcome measure was the
successful completion rate of ERP. Failure of ERP was defined as any
unplanned hospital visit earlier than the scheduled date for urethral
catheter removal. Failure was further subdivided into day visit or
overnight stay.
Statistical analysis
Discrete variables were expressed as percentage
frequency, whereas continuous variables were reported as mean with
standard deviation or median with interquartile range (IQR). The two
cohorts were compared using Chi squared, Fisher’s exact, Student’s t,
and Mann-Whitney U tests, as appropriate. Using the outcomes of
early morbidity and operative failure, multivariable analysis was
performed using a logistic regression model by the enter method, which
estimated the odds ratios (ORs) and 95% confidence intervals (95% CIs) of
potential associated factors, including age at the time of surgery, type
of hypospadias, type of surgical repair, and the service model.
Statistical analysis was performed with SPSS (Windows version 23; IBM
Corp, Armonk [NY], United States). A two-tailed P value of <0.05 was
considered to be statistically significant. Based on type I error of 0.05
and power of 0.8, 82 to 152 cases in each cohort would be required to show
any two-tailed significant difference in the operative failure rates with
a difference of 15% to 20% between the two cohorts.
Results
There were 302 major primary hypospadias repairs
(OS cohort=176; NS cohort=126) eligible for inclusion in the study. We
identified 107 cases of reoperative hypospadias repairs and one case of
BMG during the study period; these were excluded from this study. No
patients were lost to the first follow-up examination after urethral
catheter removal. The median follow-up durations of the OS and NS cohorts
were 32 (IQR, 20-58) and 20 (IQR, 14-30) months, respectively
(P<0.001).
Of the NS cohort, 111 (88.1%) patients successfully
completed the ERP. Of the 15 patients who failed to complete ERP, 11 (8.7%
of total) returned earlier in an unplanned day visit for wound assessment;
these patients only required reassurance without any intervention. Four
patients (3.2% of total) required additional overnight hospital stay.
Reasons for additional overnight stay were minor wound bleeding (n=1),
dislodgement of urethral catheter (n=2), and social reasons (n=1). The
patient who failed ERP for social reasons was an orphan, and staff at the
orphanage found it difficult to perform wound care at their institution.
Table 1 summarises the findings comparing patient
characteristics and early morbidity between the two cohorts. The median
age at the time of surgery was older in the OS than the NS cohort
(P<0.001). There was no difference between the two groups in type of
hypospadias, type of surgical procedures, and time interval between
surgery and urethral catheter removal. The median LOS was 2 days in the NS
cohort versus 10 days in the OS cohort (P<0.001). Patients in the NS
cohort experienced less early morbidity than those in the OS cohort (5.6%
vs 15.9%; P=0.006).
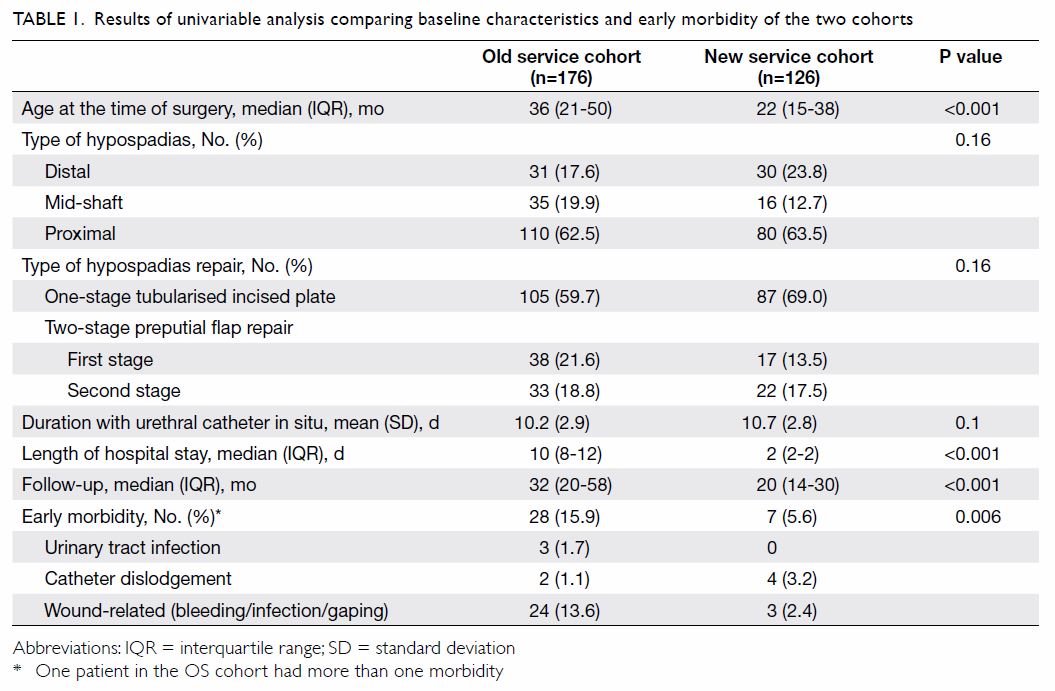
Table 1. Results of univariable analysis comparing baseline characteristics and early morbidity of the two cohorts
Excluding patients who had received only the first
stage of a two-stage repair, 138 and 109 patients of the OS and NS cohort
were eligible for assessment of operative success, respectively. Patients
in the NS cohort had a lower operative failure rate than those in the OS
cohort (20.2% vs 44.2%; P<0.001). Specifically, patients in the NS
cohort had a lower incidence of urethral fistula and dehiscence than
patients in the OS cohort (P=0.002 and 0.001); there were no differences
in the other complications (Table 2).
In the multivariable analysis, the NS model was the
only factor that was independently associated with reduced odds of early
morbidity (OR=0.35, 95% CI=0.15-0.85; P=0.02). The NS model was also
associated with reduced odds of operative failure (OR=0.32, 95%
CI=0.17-0.59; P<0.001) compared with the OS model. Compared with
proximal hypospadias, distal hypospadias had reduced odds for operative
failure (OR=0.14, 95% CI, 0.06-0.37; P<0.001). Age at the time of
surgery and surgical techniques were not associated with any difference in
operative success (Table 3).
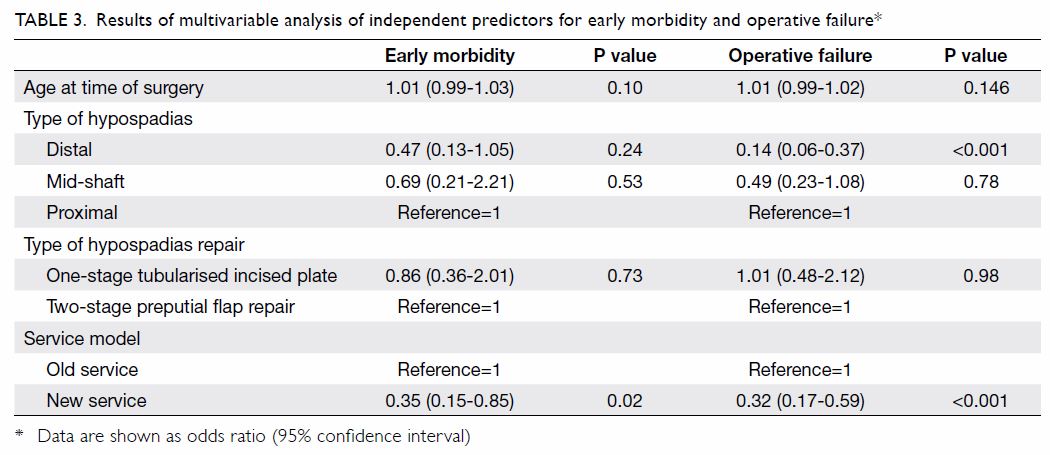
Table 3. Results of multivariable analysis of independent predictors for early morbidity and operative failure
Discussion
The conventional practice of keeping patients in
hospital until urethral catheter removal after hypospadias surgery is well
reflected from the first annual Surgical Outcome Monitoring and
Improvement Programme Report in 2008/09 to the fifth report in 2012/13
issued by the Hong Kong Hospital Authority.10
11 12
13 14
The median LOS after hypospadias surgery performed in Hospital Authority
hospitals ranged from 9 to 11 days from 2008 to 2013.10 11 12 13 14 It was a traditionally held belief that Hong Kong
parents would not be sufficiently competent to provide proper wound care
at home, and that surgical outcomes would be adversely affected if
patients were discharged from hospital with the urethral catheter in situ.
There was also concern that Hong Kong parents would not welcome the offer
of early hospital discharge, given the reality that the actual costs
billed to parents for in-patient service in Hospital Authority hospitals
are relatively insignificant, compared with other parts of the world where
medical insurance covers only very short in-patient care after hypospadias
surgery. The present study was the first in Hong Kong to investigate the
outcomes of hypospadias surgery after the introduction of an ERP. It is
important to note that our findings do not reflect purely the effect of
ERP but the effect of an NS model that features ERP implementation by a
dedicated surgical team.
Our findings demonstrate that ERP can be applied
effectively and safely to all children who undergo primary hypospadias
repair, regardless of the severity and type of hypospadias. Since its
introduction, we have offered ERP to 126 consecutive patients and none of
the parents or caregivers have declined the offer. Only one patient
discontinued ERP for social reasons, as that child was an
institutionalised orphan. Penile wound care does not require special
skills and involves only wound irrigation with normal saline or clean
water a few times daily. Patients can also be bathed with the urethral
catheters in situ. Adequate preoperative counselling and postoperative
wound care demonstration by the same surgeons who performed the surgery is
the key to promoting the acceptance of ERP among parents.
Almost 90% of our patients completed ERP
successfully. Among those who failed to complete ERP, none had major
adverse events that required surgical intervention and, overall, only 3.2%
of patients required additional overnight stay. The median hospital stay
of 2 days under the NS model was significantly shorter than the median of
10 days in our OS control cohort. In-patient services are precious
resources in our health care system. A much shorter LOS after hypospadias
surgery allows for better allocation of health care resources to other
service areas in which in-patient care is more indicated.
More importantly, our findings suggest that ERP
does not increase early morbidity after primary hypospadias repair. On the
contrary, the NS model was the only factor that was found to independently
predict a reduced risk of early morbidity. Our finding of an early
morbidity rate of 5.6% in the NS model is in agreement with the 4.9%
reported by a previous study in the United States.15 Our finding that most of the early morbidity in the
OS model was wound-related and our observation that, in some of these
patients, the wound swab grew Pseudomonas and extended spectrum
beta-lactamase Escherichia coli raised the concern of possible
hospital-acquired infection. While more evidence is needed to attribute
the high early morbidity rate under the OS model solely to the prolonged
hospital stay, it follows logically that avoiding unnecessary hospital
stay is an effective way to prevent hospital-acquired infection if
in-patient care does not give any additional benefits.
We found a better outcome after primary hypospadias
repair under the NS versus OS model in both univariable and multivariable
analyses. This study not only provides evidence that the implementation of
ERP did not reduce operative success, but also demonstrates how our centre
has responded to the international trend of concentrating hypospadias
repairs among dedicated hypospadias surgeons.2
16 17
In recent years, there has been an international call to stop the practice
of hypospadias repair by occasional surgeons. Proponents of this view hold
that surgeons who perform hypospadias repair should be proficient in using
various techniques to correct the full spectrum of hypospadias defects,
from distal hypospadias to the most complex proximal type.17 18 The
preoperative impression of the ectopic meatal position is not a reliable
reflection of the severity of hypospadias, and many cases are found to be
more complicated intra-operatively.19
Under the NS model, we abandoned our policy of allowing all paediatric
surgical specialists to perform hypospadias surgery; instead, all
hypospadias repairs were concentrated among the three specialists who
subspecialised in paediatric urology.
We believe the improved operative success under the
NS model is attributable to the establishment of the dedicated team, which
has also introduced some technical modifications in the existing
techniques.20 Our overall failure
rate of 20.2% of patients requiring reoperation or re-intervention in the
NS cohort is in agreement with the 18.1% reported by a national
population-based study in the United Kingdom21
and the 24.1% reported by a regional tertiary centre in Europe.22 Both studies included primary repairs of all types of
hypospadias performed by multiple techniques, such as those used in the
present study.21 22 Previous studies have shown that centres that operate
on more than 20 cases per year have a better operative success than those
that operate less frequently,21
and surgeons who perform 20 primary repairs annually have reduced odds of
failure compared with those who perform 10 per year.23 Although the minimum number of hypospadias repairs
per year a surgeon must perform to be considered competent remains
debatable, it is recommended that hypospadias repairs be performed by
surgeons who perform a high volume of repairs and are intellectually
interested in this subject, with continuous review of their own results.17 The current three-member team in
our institution strikes a balance between surgical outcomes and other
practical issues, such as stable staffing, expertise, training, and
succession.
Proximal hypospadias has been known to be
associated with a higher failure rate in primary repair and a higher
reoperation rate than distal hypospadias.24
25 The most recent studies from
major centres have unanimously suggested that the failure rate of primary
repair of proximal hypospadias has actually been underreported in the
literature.6 26 27 Our
finding of increased odds of failure in primary repair of proximal
hypospadias when compared with the distal type is in agreement with the
current evidence. We did not find age at the time of surgery and surgical
techniques to be independent predictors of repair failure, and our finding
is in agreement with other studies.22
We acknowledge the limitations of the retrospective
nature of our study and the lack of randomisation. Data are lacking on
anatomical variations such as quality of urethral plate and glans size,
which may have affected the surgical outcomes. Patients were not
randomised by the type of recovery programme and the study participants
were assigned to the two cohorts according to the service model at the
time. Our results could have been confounded by the effect of accumulating
experience in hypospadias surgery throughout the study period. Data were
collected by investigators who were not blinded to the types of service
models; therefore, there was potential bias in the data collection
process, but inter-rater reliability was not examined. As the ERP was
implemented at the same time as the establishment of the dedicated team,
these two factors could not be analysed separately. Being the more recent
cohort, the patients under the NS model had shorter follow-up duration
than those under the OS model. However, our median follow-up duration of
20 months in the NS cohort compares favourably to that of many published
studies.25
Despite these limitations, our findings demonstrate
the safety and effectiveness of implementing ERP to primary hypospadias
repair for the full spectrum of hypospadias severity. A dedicated surgical
team may play an important role in the successful implementation of ERP
and optimisation of surgical outcomes.
Author contributions
All authors have made substantial contributions to
the concept of this study; acquisition of data; analysis or interpretation
of data; drafting of the article; and critical revision for important
intellectual content.
Funding/support
This research received no specific grant from any
funding agency in the public, commercial, or not-for-profit sectors.
Declaration
All authors have no conflicts of interest to
disclose. All authors had full access to the data, contributed to the
study, approved the final version for publication, and take responsibility
for its accuracy and integrity.
Ethical approval
The study protocol was approved by the Joint
Chinese University of Hong Kong–New Territories East Cluster Clinical
Research Ethics Committee. The requirement for patient consent was waived
by the ethics board.
References
1. Baskin LS, Ebbers MB. Hypospadias:
anatomy, etiology, and technique. J Pediatr Surg 2006;41:463-72. Crossref
2. Steven L, Cherian A, Yankovic F, Mathur
A, Kulkarni M, Cuckow P. Current practice in paediatric hypospadias
surgery; a specialist survey. J Pediatr Urol 2013;9(6 Pt B):1126-30. Crossref
3. Wilkinson DJ, Farrelly P, Kenny SE.
Outcomes in distal hypospadias: a systematic review of the Mathieu and
tubularized incised plate repairs. J Pediatr Urol 2012;8:307-12. Crossref
4. Long CJ, Canning DA. Hypospadias: are we
as good as we think when we correct proximal hypospadias. J Pediatr Urol
2016;12:196.e1-5. Crossref
5. Snodgrass WT, Bush N, Cost N.
Tubularized incised plate hypospadias repair for distal hypospadias. J
Pediatr Urol 2010;6:408-13. Crossref
6. Pippi Salle JL, Sayed S, Salle A, et al.
Proximal hypospadias: a persistent challenge. Single institution outcome
analysis of three surgical techniques over a 10-year period. J Pediatr
Urol 2016;12:28.e1-7. Crossref
7. Pohl HG, Joyce GF, Wise M, Cilento BJ
Jr. Cryptorchidism and hypospadias. J Urol 2007;177:1646-51. Crossref
8. Snodgrass W, Bush N. Tubularized incised
plate proximal hypospadias repair: continued evolution and extended
applications. J Pediatr Urol 2011;7:2-9. Crossref
9. McNamara ER, Schaeffer AJ, Logvinenko T,
et al. Management of proximal hypospadias with 2-stage repair: 20-year
experience. J Urol 2015;194:1080-5. Crossref
10. Surgical Outcomes Monitoring &
Improvement Program (SOMIP) report. Volume One: July 2008-June 2009.
Hospital Authority, Hong Kong SAR Government; 2010.
11. Surgical Outcomes Monitoring &
Improvement Program (SOMIP) report. Volume Two: July 2009-June 2010.
Hospital Authority, Hong Kong SAR Government; 2011.
12. Surgical Outcomes Monitoring &
Improvement Program (SOMIP) report. Volume Three: July 2010-June 2011.
Hospital Authority, Hong Kong SAR Government; 2012.
13. Surgical Outcomes Monitoring &
Improvement Program (SOMIP) report. Volume Four: July 2011-June 2012.
Hospital Authority, Hong Kong SAR Government; 2013.
14. Surgical Outcomes Monitoring &
Improvement Program (SOMIP) report. Volume Five: July 2012-June 2013.
Hospital Authority, Hong Kong SAR Government; 2014.
15. Meyer C, Sukumar S, Sood A, et al.
Inpatient hypospadias care: trends and outcomes from the American
nationwide inpatient sample. Korean J Urol 2015;56:594-600. Crossref
16. Springer A, Krois W, Horcher E. Trends
in hypospadias surgery: results of a worldwide survey. Eur Urol
2011;60:1184-9. Crossref
17. Snodgrass W, Macedo A, Hoebeke P,
Mouriquand PD. Hypospadias dilemmas: a round table. J Pediatr Urol
2011;7:145-57. Crossref
18. Malone P. Commentary to “A
standardized classification of hypospadias”. J Pediatr Urol 2012;8:415. Crossref
19. Orkiszewski M. A standardized
classification of hypospadias. J Pediatr Urol 2012;8:410-4. Crossref
20. Tam YH, Pang KK, Wong YS, et al.
Improved outcomes after technical modifications in tubularized incised
plate urethroplasty for mid-shaft and proximal hypospadias. Pediatr Surg
Int 2016;32:1087-92. Crossref
21. Wilkinson DJ, Green PA, Beglinger S,
et al. Hypospadias surgery in England: higher volume centres have lower
complication rates. J Pediatr Urol 2017;13:481.e1-6. Crossref
22. Spinoit AF, Poelaert F, Van Praet C,
Groen LA, Van Laecke E, Hoebeke P. Grade of hypospadias is the only factor
predicting for re-intervention after primary hypospadias repair: a
multivariate analysis from a cohort of 474 patients. J Pediatr Urol
2015;11:70.e1-6. Crossref
23. Lee OT, Durbin-Johnson B, Kurzrock EA.
Predictors of secondary surgery after hypospadias repair: a population
based analysis of 5,000 patients. J Urol 2013;190:251-5. Crossref
24. Castagnetti M, El-Ghoneimi A. Surgical
management of primary severe hypospadias in children: systematic 20-year
review. J Urol 2010;184:1469-74. Crossref
25. Pfistermuller KL, McArdle AJ, Cuckow
PM. Meta-analysis of complication rates of the tubularized incised plate
(TIP) repair. J Pediatr Urol 2015;11:54-9. Crossref
26. Stanasel I, Le HK, Bilgutay A, et al.
Complications following staged hypospadias repair using transposed
preputial skin flaps. J Urol 2015;194:512-6. Crossref
27. Long CJ, Chu DI, Tenney RW, et al.
Intermediate-term followup of proximal hypospadias repair reveals high
complication rate. J Urol 2017;197(3 Pt 2):852-8. Crossref