Hong
Kong Med J 2018 Apr;24(2):206.e1–2
DOI: 10.12809/hkmj164980
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
PICTORIAL MEDICINE
Pancreatic pseudocyst rupture into the portal vein
diagnosed by magnetic resonance imaging
HC Lee, FRCR, FHKCR1; KH Tse, FRCR,
FHKCR2
1 Department of Radiology, United
Christian Hospital, Kwun Tong, Hong Kong
2 Department of Radiology, Princess
Margaret Hospital, Laichikok, Hong Kong
Corresponding author: Dr HC Lee (lhc874@ha.org.hk)
A 38-year-old man presented to the United Christian
Hospital, Hong Kong, with acute epigastric pain in October 2014. He was a chronic drinker
and had experienced intermittent abdominal pain for 6 months. His serum
amylase level was elevated (454 IU/L), and a diagnosis of acute-on-chronic
pancreatitis was made. The patient was treated conservatively.
Magnetic resonance cholangiopancreatography
performed 3 months after hospital discharge showed a 5.8-cm-diameter
unilocular cystic mass over the pancreatic head (Fig 1). The main and right portal veins showed a
signal intensity identical to that of the cystic pancreatic lesion on all
phases, without any contrast enhancement (Fig 2). There was communication between the main
portal vein and the cystic mass (Fig 3). The presence of multiple collateral veins in
the hepatic hilum was consistent with cavernous transformation (Fig
2c). Features were suggestive of a pancreatic head pseudocyst that
had ruptured into the main portal vein.
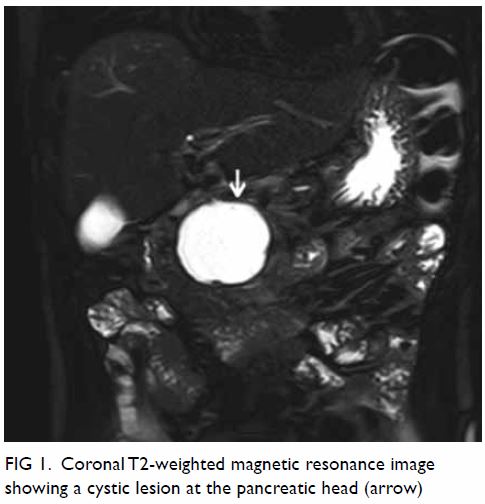
Figure 1. Coronal T2-weighted magnetic resonance image showing a cystic lesion at the pancreatic head (arrow)
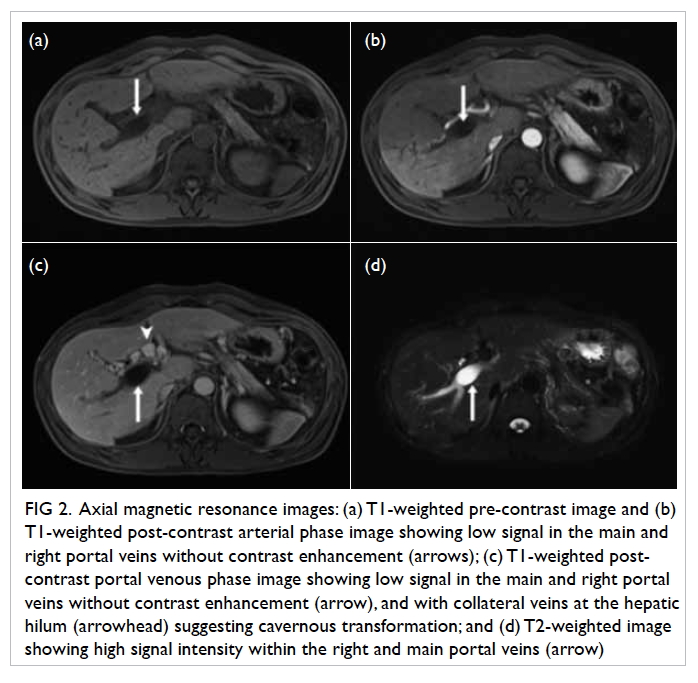
Figure 2. Axial magnetic resonance images: (a) T1-weighted pre-contrast image and (b) T1-weighted post-contrast arterial phase image showing low signal in the main and right portal veins without contrast enhancement (arrows); (c) T1-weighted post-contrast portal venous phase image showing low signal in the main and right portal veins without contrast enhancement (arrow), and with collateral veins at the hepatic hilum (arrowhead) suggesting cavernous transformation; and (d) T2-weighted image showing high signal intensity within the right and main portal veins (arrow)
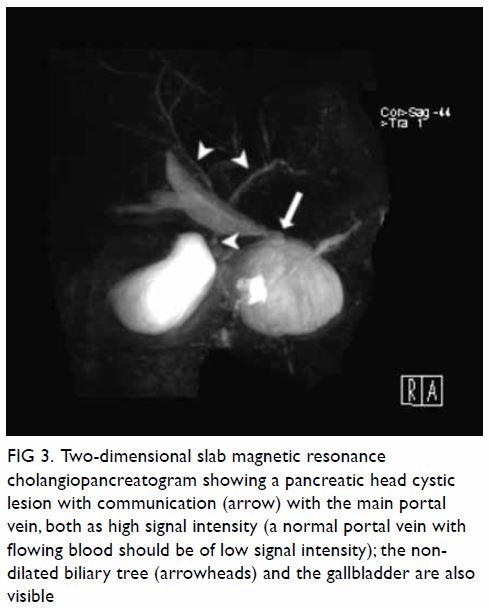
Figure 3. Two-dimensional slab magnetic resonance cholangiopancreatogram showing a pancreatic head cystic lesion with communication (arrow) with the main portal vein, both as high signal intensity (a normal portal vein with flowing blood should be of low signal intensity); the non-dilated biliary tree (arrowheads) and the gallbladder are also visible
The patient presented again 1 month later with
recurrent pancreatitis. Contrast computed tomography (CT) showed that the
pancreatic pseudocyst had enlarged, to 7.6 cm in diameter (Fig
4). Pancreatic cystojejunostomy and cholecystectomy were performed.
Intra-operatively, a 10-cm cystic lesion at the pancreatic head was found,
and 200 mL of clear fluid was aspirated. Intra-operative ultrasonography
showed the lack of flow in the main portal vein.
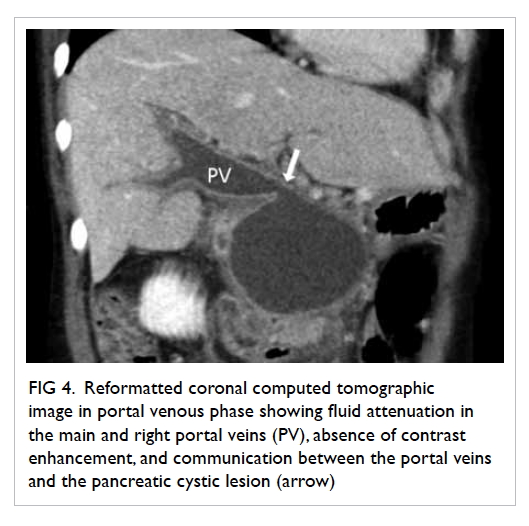
Figure 4. Reformatted coronal computed tomographic image in portal venous phase showing fluid attenuation in the main and right portal veins (PV), absence of contrast enhancement, and communication between the portal veins and the pancreatic cystic lesion (arrow)
The patient had a few more episodes of recurrent
pancreatitis thereafter. The last CT examination, performed 2 years after
surgery, showed a reduction in the size of the pseudocyst, to 2 cm. The
patient remains on regular follow-up.
Discussion
Rupture of a pancreatic pseudocyst into the portal
vein is an uncommon complication; only a handful of cases have been
reported in the literature.1 It has
been postulated that portal vein thrombosis occurs first, followed by
erosion of the portal vein by pancreatic enzymes present in the
pseudocyst, and subsequent lysis of the thrombus and filling of the portal
vein with fluid.1 2 It has also been reported that rupture of the
pseudocyst into the portal vein may be the initial event, followed by the
development of portal vein thrombosis.3
4
Previously reported cases have used various
diagnostic techniques. Invasive methods include endoscopic retrograde
cholangiopancreatography and portography with surgery. Non-invasive
methods include ultrasonography, CT, and magnetic resonance imaging (MRI).
In all reported cases in which MRI was performed, the signal intensity of
fluid in the portal vein matched that of the pancreatic pseudocyst.1 2 3 Direct communication between the portal vein and the
pancreatic pseudocyst was clearly seen in most cases. The presence of
residual thrombus or concomitant existence of complete thrombosis of the
portal vein has also been reported.1
There is no well-established treatment protocol.
Options include conservative management, endoscopic or percutaneous
procedures, or surgery. The patient’s clinical condition and symptoms,
patency of the portal vein, communication between the pseudocyst and
pancreatic duct, size of pseudocyst, and any other complicating factors
should be considered in treatment planning.3
In summary, rupture of a pancreatic pseudocyst into
the portal vein is an uncommon complication. On MRI, demonstration of
fluid signal in the portal vein that matches the signal intensity of a
pancreatic pseudocyst allows the diagnosis to be confidently made,
obviating the need for more invasive investigations.
Declaration
The authors have no conflicts of interest to
disclose.
References
1. Dayal M, Sharma R, Madhusudhan KS, et
al. MRI diagnosis of rupture of pancreatic pseudocyst into portal vein:
case report and review of literature. Ann Gastroenterol 2014;27:173-6.
2. Riddell A, Jhaveri K, Haider M.
Pseudocyst rupture into the portal vein diagnosed with MRI. Br J Radiol
2005;78:265-8. Crossref
3. Ng TS, Rochefort H, Czaplicki C, et al.
Massive pancreatic pseudocyst with portal vein fistula: case report and
proposed treatment algorithm. Pancreatology 2015;15:88-93. Crossref
4. Dawson BC, Kasa D, Mazer MA. Pancreatic
pseudocyst rupture into the portal Vein. South Med J 2009;102:728-32. Crossref

