DOI: 10.12809/hkmj176945
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
MEDICAL PRACTICE CME
Complexity of syncope in elderly people: a
comprehensive geriatric approach
CW Wong, FHKAM (Medicine), FHKCP
Department of Medicine and Geriatrics, Caritas
Medical Centre, Shamshuipo, Kowloon, Hong Kong
Corresponding author: Dr CW Wong (chitwaiwong@hotmail.com)
Abstract
Syncope is a prevalent health problem among
elderly people. It may be neurally mediated or caused by conditions such
as orthostatic hypotension, postprandial hypotension, and cardiac
disorders. A combination of different aetiologies is not uncommon in the
elderly people. Many pathophysiological processes, including age-related
physiological changes, co-morbidities, concomitant medication use, and
prolonged bedrest, coexist and predispose elderly people to syncope;
advanced age and cardiac syncope are associated with increased
mortality. Recurrent syncope and its co-morbidities, such as
fall-related physical injury, negative psychological impact, and
functional decline, may increase the dependency of elderly patients.
Furthermore, the overlap between falls and syncope, and the interaction
between syncope and frailty complicate management. Available clinical
guidelines for the management of syncope that focus on diagnosis,
investigation, and treatment are therefore insufficient to address
syncope in elderly patients. A comprehensive geriatric approach that
considers an individual’s functional and cognitive capacities, as well
as medical and psychosocial aspects, would be more appropriate.
Introduction
Syncope is a transient loss of consciousness (LOC)
and postural tone resulting from global cerebral hypoperfusion, followed
by spontaneous and complete recovery and no neurological sequelae.1 This pathophysiology distinguishes syncope from other
causes of transient LOC, including metabolic disorder, epileptic seizure,
and transient ischaemic attack.
Syncope is prevalent in elderly populations. After
a peak in younger populations (age, 10-30 years), the incidence of syncope
increases sharply from 5.4 events per 1000 person-years in people aged 60
to 69 years to 11.1 events per 1000 person-years in those aged 70 to 79
years, and reaching 19.5 events per 1000 person-years in those aged 80
years or older.2 The incidence is
similar for men and women but tends to increase in women of advanced age.
The prevalence of syncope is high for the institutionalised elderly, at
23%.3 Syncope in elderly patients
often presents atypically, such as with falls. Elderly patients may also
have difficulty in recalling events. Therefore, the true incidence and
prevalence of syncope are expected to be higher than those estimated in
some previous studies.
Syncope is typically an isolated disease in young
people. However, it is usually multifactorial and associated with many
predisposing factors in the elderly people; thus, its management is
challenging. In this article, the aetiology of syncope in the elderly
people, pathophysiological factors that impair haemodynamic homeostasis,
consequences of syncope, and relationships between syncope and falls and
between syncope and frailty are discussed. Finally, a comprehensive
approach for the management of syncope in elderly patients is recommended.
Causes of syncope in the elderly people
The causes of syncope are highly age-dependent.4 Reflex or neurally mediated syncope is the most common
cause, particularly in younger patients. With increasing age, orthostatic
hypotension (OH) and cardiac syncope occur more frequently.
Reflex or neurally mediated syncope
Reflex syncope is a heterogeneous group of
conditions, including vasovagal syncope, situational syncope, and carotid
sinus syndrome, and is the most frequent cause of syncope in the elderly
people (44% of cases).5 In reflex
syncope, the cardiovascular reflexes that normally help control the
circulation become intermittently inappropriate (eg, inappropriate
vasodilation or bradycardia) in response to a trigger (eg, emotion or
orthostatic stress).
Vasovagal syncope is the most common form of reflex
syncope and is mediated by the vasovagal reflex. The most common triggers
in elderly people are prolonged standing or sitting and use of vasodilator
drugs. The classic prodromal features (pallor, diaphoresis, nausea, and
warmth) are less prominent in elderly people.
Situational syncope occurs in conditions that
trigger the Valsalva manoeuvre, such as urination, defaecation, coughing,
and swallowing.
Syncope exacerbated by the carotid sinus reflex
response is referred to as carotid sinus syndrome (CSS). It is related to
underlying carotid sinus hypersensitivity, which is diagnosed when carotid
sinus massage (CSM) produces asystole longer than 3 seconds
(cardioinhibitory CSS) or a reduction in systolic blood pressure (SBP) by
more than 50 mm Hg (vasodepressor CSS). Carotid sinus syndrome typically
occurs in adults older than 50 years and is predominant in men. There is
usually no identifiable trigger, but CSS may be precipitated by sudden
head turning and wearing tight clothing around the neck.6 Carotid sinus syndrome is regarded as a significant
cause of syncope and unexplained falls in the elderly people; as many as
45% of elderly patients presenting with syncope or unexplained falls
demonstrate carotid sinus hypersensitivity.7
8
Orthostatic hypotension
Orthostatic hypotension (OH) is prevalent in
elderly people and in those who are frail, affecting up to 18% of people
aged 65 years or older9 and up to
52% of institutionalised elderly patients.10
It also accounts for 30% of cases of syncope in patients aged 75 years or
older.5 Orthostatic hypotension is
defined as a sustained reduction in systolic blood pressure of at least 20
mm Hg or in diastolic blood pressure of 10 mm Hg, within 3 minutes of
standing.11 Because elderly
patients may present beyond 3 minutes of standing and OH may not always be
reproducible in elderly people, repeated measurement—preferably in the
morning—may be required. Among factors that precipitate OH are age-related
changes in the blood pressure regulatory mechanism, disease-related
autonomic dysfunction, and numerous other factors that decrease cardiac
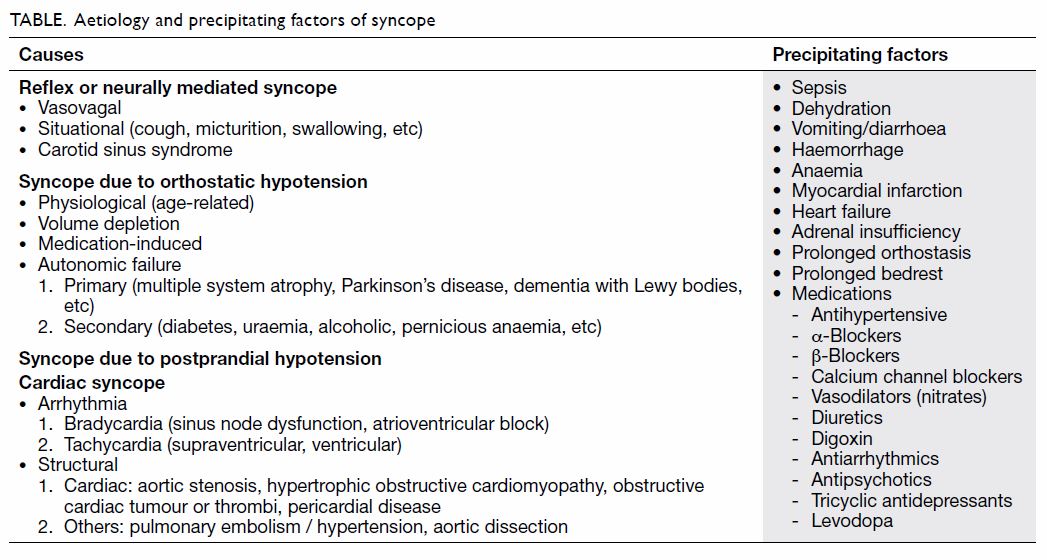
output or total peripheral vascular resistance (Table). Occurrence of OH is significantly related to
the number of co-morbidities and to potentially causative medications.12 13 However,
supine systolic hypertension is often also present in elderly people with
OH and further complicates management of OH.
Postprandial hypotension
Postprandial hypotension (PPH) is also common in
the elderly people, with a prevalence reaching 59% in older Chinese men,
especially in those older than 80 years.14
It is often under-recognised as a potential cause of syncope and is seldom
mentioned in published clinical guidelines on syncope. In one study, PPH
accounted for 8% of syncopal episodes.15
Postprandial hypotension is defined as a decline in systolic blood
pressure of 20 mm Hg or more, or to lower than 90 mm Hg, within 2 hours of
starting a meal.16 Similar to OH,
PPH is more likely to occur in the morning. Consuming a meal that is large
or rich in carbohydrates also increases the risk of PPH. The condition is
caused by the pooling of blood in the splanchnic vascular bed. Although
PPH occurs frequently with OH, the pathophysiological mechanisms of OH and
PPH may be different.17
Postprandial hypotension is more likely to occur if patients have diabetes
mellitus, hypertension, or Parkinson’s disease, or if they take multiple
concurrent medications, particularly diuretics.18
19
Cardiac syncope
Cardiac syncope accounts for up to 15% of cases of
syncope in the elderly people.5 20 It is caused by impaired cardiac
output due to arrhythmia or structural heart disease in which left
ventricular blood flow is obstructed. Arrhythmia—either bradyarrhythmia or
tachyarrhythmia—is the most common cause of cardiac syncope. Calcific
degenerative aortic stenosis is the most common valvular lesion in the
elderly people and also the most common structural cardiovascular cause of
syncope.21 In general, cardiac
syncope is associated with a high mortality rate.2
Unexplained syncope
The prevalence of unexplained syncope has decreased
as the use of diagnostic techniques, such as the tilt-table test and CSM,
has increased. These techniques can identify reflex syncope and CSS in the
elderly people. The reported proportion of elderly patients with
unexplained syncope decreased from 40% in 198622
to 10% in 2006.5 For elderly
patients with syncope in whom the aetiology remains undetermined after
extensive evaluation, it is important to look for a cardiac cause. In a
study using an implantable loop recorder, arrhythmia accounted for 59% of
all recurrences of syncope that would previously have been regarded as
unexplained.23
Multiple causes of syncope
There are commonly multiple potential causes of
syncope in elderly patients: in 23.5% of those aged 65 or older and in
13.4% of those younger than 65 years.24
Apart from older age, patients with atrial fibrillation or symptomatic
heart failure, or those receiving drug therapy for cardiac conditions are
more likely than others to have multiple causes of syncope. The presence
of multiple causes also correlates with poor survival.
Multiple risk factors in the elderly people
Maintaining blood pressure at a constant level
during a wide range of daily activities or conditions requires an intact
cardiovascular system, baroreflex function, autonomic nervous system, and
humoural regulatory mechanism. Age-related change in the blood pressure
regulatory mechanism increases the susceptibility to syncope in elderly
people. Baroreflex sensitivity is blunted by ageing, resulting in reduced
heart rate and reduced vasoconstriction response to hypotensive stimuli.25 Furthermore, elderly people are
prone to dehydration and reduced blood volume owing to reduced thirst
sensation, reduction in renin–aldosterone activity, and elevation of
atrial natriuretic peptide, which decreases the kidneys’ capacity to
conserve salt and water.26 27 The blunted baroreflex response and contracted blood
volume, together with age-related diastolic dysfunction, can lead to low
cardiac output and thus low cerebral blood flow. The latter predisposes
elderly people to syncope under conditions causing hypotensive stress.
Co-morbidities and concomitant medication use can
impair the adaptive response to hypotensive stress. Any conditions that
contribute to haemodynamic stress or impair the blood pressure regulation
mechanism, leading to decreased cardiac output or total peripheral
vascular resistance (vasodilation), predispose the elderly people to
reflex syncope and OH. Syncope can be induced by acute conditions, such as
sepsis, myocardial infarction, cardiac arrhythmia, heart failure,
haemorrhage, and dehydration. It can also be induced by chronic conditions
such as chronic adrenal suppression from steroid use (which can produce
hypovolaemia), as well as untreated or uncontrolled hypertension and
coronary heart disease. Untreated or uncontrolled hypertension can
increase the risk of OH by reducing baroreflex sensitivity and shifting
the threshold for cerebral autoregulation to a higher blood pressure,28 29 whereas
coronary heart disease is associated with carotid sinus hypersensitivity.30 In addition, patients presenting
with OH may have autonomic insufficiency, which can be secondary to
peripheral nervous system diseases, such as diabetes mellitus, alcoholism,
chronic kidney disease, vitamin B12 deficiency, and
paraneoplastic disease. Autonomic insufficiency may also be due to central
nervous system diseases, such as multiple system atrophy, dementia with
Lewy bodies, and Parkinson’s disease.
The Table lists the medications that may
precipitate syncope. Although antihypertensive drugs are commonly thought
to increase the risk of postural blood pressure drop and thus OH, clinical
trials have shown inconsistent results.31
On the contrary, the reduction or normalisation of blood pressure by
antihypertensive agents may even improve OH in elderly patients with
hypertension.32 However, excessive
blood pressure reduction and concurrent use of three or more
antihypertensive drugs is independently associated with OH.12 13
Diuretics, nitrates, antipsychotics, tricyclic antidepressants, and
levodopa can also induce OH. Drugs that can induce QT prolongation and
torsades de pointes include antiarrhythmics and antipsychotics.33 Drugs that can cause bradyarrhythmia include
amiodarone, beta-blockers, calcium channel blockers, and digoxin. Because
of age-related changes in pharmacokinetics and pharmacodynamics, the
adverse effects and interactions of these drugs are further exacerbated in
the elderly people.
Bedrest is common in patients with acute illness or
in those who are frail or chronically ill. After prolonged bedrest,
however, elderly patients can develop syncope when sitting up. Prolonged
bedrest can cause deconditioning in the musculoskeletal and cardiovascular
system, as well as pressure natriuresis, which in turn induces blood
volume contraction. These conditions can aggravate OH, syncope, and fall.34
All of the above pathophysiological processes can
act together to impair cardiovascular compensation for haemodynamic stress
in elderly people and thereby complicate the management of syncope.
Consequences of syncope
Whether syncope independently increases the risk of
overall or cardiac mortality remains controversial. Nonetheless, among
patients with syncope, mortality generally tends to increase with
advancing age and in those with cardiac syncope and OH.35 36 37 38 39 A 2-year study found that the overall mortality rate
was 0% in patients aged 65 to 69 years, increasing to 14%, 22%, and 43% in
patients aged 70 to 79 years, 80 to 89 years, and ≥90 years, respectively.37 Syncope of cardiac cause was
noted to have higher 5-year mortality (51%) than non-cardiac (30%) or
unknown-cause (24%) mortality.38
Orthostatic hypotension is associated with a significantly increased risk
of death for patients younger than 65 years (relative risk = 1.78; 95%
confidence interval = 1.25-2.52) but not for older patients.39 Overall prognosis is worse in patients with an
underlying cardiac disease such as myocardial infarction, arrhythmia,
structural cardiac defect, cardiomyopathy, or congestive heart failure,
regardless of the occurrence or aetiology of syncope.36 40 41 The presence of multiple potential causes of syncope
also predicts a lower survival rate as compared with a single cause of
syncope (73% vs 89% at 4 years).24
In contrast, patients with non-cardiac co-morbidities or no underlying
heart disease are at low risk.
Patients with a history of syncope have an
increased risk of recurrence. Patients with syncope have a 20% recurrence
rate at 1 year, compared with a 2% rate of syncope in patients without
prior syncope.40 The recurrence
rate is even higher in the institutionalised elderly, at 30%.3 Syncope recurs more frequently in older patients at 2
years, with a rate of 28% in patients aged 65 to 79 years, 37% in those
aged 80 to 89 years, and 43% in those older than 90 years.37 Other factors predicting recurrence include the
concurrent use of multiple medications with known adverse effects of OH or
syncope and cardiac co-morbidities, particularly atrial fibrillation,
atrioventricular or left bundle branch block, or aortic valve stenosis.42 Recurrence may not be related to
the aetiology of syncope, although a higher recurrence in patients
affected by reflex and unexplained syncope has been reported.36
Besides physical injuries and disabilities due to
syncope-related falls, depression and fear of falling after syncope may
reduce elderly patients’ functional capacity and mobility, and can result
in institutionalisation. Furthermore, syncope can negatively affect
quality of life,43 particularly in
patients who are older, have multiple co-morbidities, and experience
recurrent episodes of syncope.44
Syncope and falls
There is an overlap between syncope and falls in
the elderly people; syncope causes falls and some falls are due to
syncope. Although taking an accurate history of an event allows the
differentiation between syncope and fall, the history is often unreliable
in the elderly people because of poor recall and lack of witnesses. Many
elderly patients will only recall the fall but not realise they fainted;
amnesia is common (up to 42%) for witnessed syncope, even in cognitively
normal elderly patients.6 7 8 45 This is particularly the case for CSS: in one study,
21% of patients with CSS presented with falls alone and 27% failed to
recall the syncope event.6
Furthermore, frequently reported reasons for falls in the elderly people,
such as muscle weakness, arthritis, gait and balance problems, visual
impairment, functional decline, depression, cognitive impairment,
polypharmacy, and environmental factors,46
47 may distract clinicians from
searching for syncope.
Nonetheless, multiple co-morbidities and
polypharmacy associated with advancing age predispose elderly people to
both falls and syncope. Moderate haemodynamic changes that are
insufficient to cause syncope may cause falls in elderly patients with
gait balance instability or slow protective reflexes.48 Such falls may be indistinguishable from syncope in
elderly patients. Considering that syncope may be a component of fall in
elderly patients, especially in those with unwitnessed or recurrent
unexplained fall, assessment of cardiovascular status and postural blood
pressure, as well as further investigation for accurate diagnosis and
treatment, are recommended.47
Syncope and frailty
Frailty that leads to diminished functional reserve
and adverse health outcomes is defined as the presence of three of more of
the following criteria: unintentional weight loss (10 lbs [~4.5 kg] in the
past year), self-reported exhaustion, weakness (grip strength), slow
walking speed, and low physical activity.49
The relationship between frailty and syncope is not well described in the
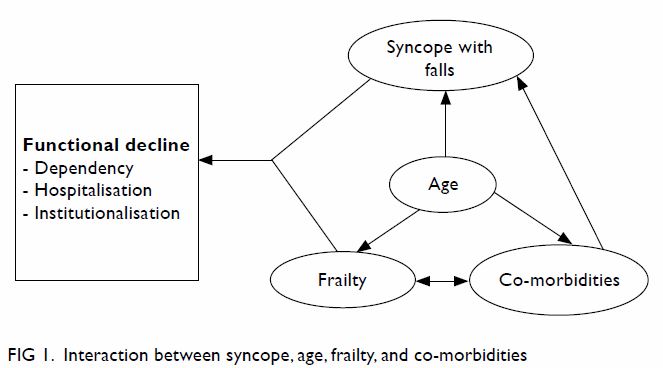
literature. However, there is an interaction between ageing,
co-morbidities, and the development of frailty (Fig 1). Co-morbidities are common among the elderly
people. As many as 82% of people aged 65 years or older have one or more
chronic conditions.50 Advancing
age and co-morbidities, in turn, increase the likelihood of being frail.
Conversely, frail people are likely to have more co-morbidities.51 Age-related physiological changes and co-morbidities
also increase the risk of syncope and falls. Thus, an episode of syncope
with a fall may act as an acute stressor in the elderly people. The
decreased physiological reserve in frail elderly patients inhibits their
response to acute stressors. This inhibited response leads to rapid
functional decline and results in hospitalisation, dependency, and
institutionalisation (Fig 1).
Comprehensive geriatric approach
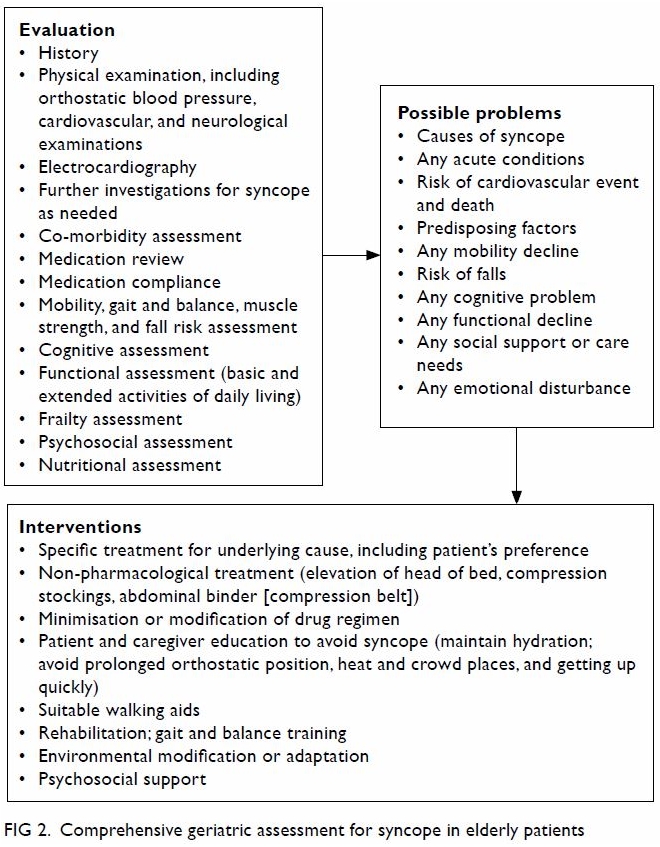
According to clinical guidelines,1 52 initial
evaluation for syncope starts with careful recording of the patient’s
history, physical examination (including orthostatic blood pressure
measurement), and electrocardiography (ECG). On the basis of these
findings, additional examinations such as Holter monitoring, CSM,
tilt-table test, echocardiography, and blood tests may be performed. The
purpose of the initial evaluation is to differentiate syncopal from
non-syncopal conditions, to determine the cause of syncope, and to
stratify the risk of major cardiovascular events or death. Predictors of
high cardiovascular risk are the presence of structural heart disease or
coronary artery disease (eg, heart failure, low left ventricular ejection
fraction, and previous myocardial infarction), palpitation before syncope,
syncope during exertion or in the supine position, and ECG features
suggesting arrhythmic disturbance. Initial evaluations can identify a
certain or highly likely cause of syncope in 63% of patients.53 If the cause remains uncertain, further investigation
is indicated. The subsequent tests are based on the findings of the
initial evaluation and suspected aetiology: tilt-table test for reflex
syncope or OH; CSM for elderly people with unexplained falls; Holter
monitoring or external/implantable loop recording to detect arrhythmia in
recurrent unpredictable syncope; echocardiography for structural heart
disease and cardiac function, especially in the presence of abnormal
findings of ECG or cardiovascular examination or suspicion from history;
or neurological evaluation for autonomic failure or neurological
conditions that are difficult to differentiate from syncope. Treatment
depends on the underlying causes and usually includes the following:
However, as outlined in this article, syncope in
elderly people has certain complexities—namely, (1) there is a marked
overlap between syncope, fall, and dizzy spell, and atypical presentations
make diagnosis difficult; (2) the syncope event is often multifactorial,
with many predisposing factors; and (3) management is often complicated by
underlying co-morbidities, concomitant medication use, cognitive and
functional decline, and declined psychosocial support. Therefore, the
above standard structural approach is insufficient to address syncope in
elderly patients. Comprehensive geriatric assessment, “a multidimensional
interdisciplinary diagnostic process focused on determining a frail
elderly person’s medical, psychological and functional capacity in order
to develop a coordinated and integrated plan for treatment and long term
follow up”, is recommended.54 This
comprehensive approach is both a diagnostic and a therapeutic process and
involves a multidisciplinary team (physician, nurse, physiotherapist,
occupational therapist, and social worker) with the collective goal of
improving care outcomes and quality of life for elderly people. When an
elderly patient is referred for syncope, an unexplained fall, or
dizziness, comprehensive geriatric assessment is applied to obtain a
thorough history and physical examination, together with assessments for
co-morbidities, frailty, cognitive and functional status, psychological
and social variables, and medication review (Fig 2). After extensive evaluation, a problem list
is generated with details of the identified syncope event and its cause or
predisposing factors, whether the patient is at high risk of
cardiovascular event or death, and any cognitive or functional impairments
or psychosocial problems. Then, multidisciplinary interventions are
integrated with the patient’s or caregiver’s preferences, so as to
conserve the patient’s health status, improve psychosocial support, and
maintain the patient’s independence and community living situation. The
following should be considered in the management of syncope:
An example of comprehensive geriatric assessment
for elderly people referred for syncope is presented in the following case
scenario. A 75-year-old woman was admitted to hospital after an episode of
transient LOC. She reported walking down the street then feeling dizzy,
passing out, and falling on the ground. There were no eyewitnesses. The
patient recovered spontaneously but could not recall the duration of LOC.
She denied any preceding events such as palpitation or chest discomfort,
except dizziness. The patient reported having experienced similar episodes
twice in the previous 2 years, once while standing and once while walking.
Her medical history included hypertension, type 2 diabetes mellitus,
ischaemic heart disease, and knee osteoarthritis, for which she was taking
ramipril, metformin, metoprolol, amlodipine, isosorbide mononitrate, and
amitriptyline. The patient lived alone, walked unaided, and went out
shopping daily. She expressed concerned about recurrent dizziness and
falls, which had restrained her social activities. Physical examination
revealed postural blood pressure drop from 110/60 to 90/50 mm Hg within 3
minutes of standing, normal heart sound, varus deformities in both knees
due to osteoarthritis, and lower-limb weakness with muscle power grade
4/5. Laboratory studies revealed a haemoglobin level of 100 g/L with a
mean corpuscular volume of 98 fL; serum vitamin B12, 120
pmol/L; random serum glucose, 6 mmol/L; and haemoglobin A1c,
5.8%. Results of renal and liver function tests and ECG were normal. A
nurse, a physiotherapist, and an occupational therapist also assessed the
patient.
Relevant problems included the following:
Interventions implemented in this case were as
follows:
Conclusions
In younger patients, vasovagal syncope is the
predominant aetiology of syncope. In contrast, CSS, OH, PPH, and cardiac
syncope become more prevalent with advancing age. Multiple aetiologies are
frequently observed in elderly patients. Interactions among age-related
physiological changes, co-morbidities, and concomitant medication use
impair haemodynamic homeostasis and predispose elderly people to syncope.
These factors, together with cognitive impairment, functional decline, and
frailty associated with advanced age, make the management of syncope in
elderly patients complex. Structured clinical guidelines are insufficient
to manage syncope in elderly patients. Use of a comprehensive geriatric
approach to integrate an individual’s co-morbidities, cognitive and
functional capacities, and medical and psychosocial aspects is more
appropriate and beneficial for elderly patients so as to maintain
functional state and quality of life.
Declaration
The author has no conflicts of interest to
disclose.
References
1. Task Force for the Diagnosis and
Management of Syncope; European Society of Cardiology (ESC); European
Heart Rhythm Association (EHRA); Heart Failure Association (HFA); Heart
Rhythm Society (HRS), Moya A, Sutton R, Ammirati F, et al. Guidelines for
the diagnosis and management of syncope (version 2009). Eur Heart J
2009;30:2631-71. Crossref
2. Soteriades ES, Evans JC, Larson MG, et
al. Incidence and prognosis of syncope. N Engl J Med 2002;347:878-85. Crossref
3. Lipsitz LA, Wei JY, Rowe JW. Syncope in
an elderly, institutionalised population: prevalence, incidence, and
associated risk. Q J Med 1985;55:45-54.
4. Strickberger SA, Benson DW, Blaggioni L,
et al. AHA/ACCF scientific statement on the evaluation of syncope: from
the American Heart Association Councils on Clinical Cardiology,
Cardiovascular Nursing, Cardiovascular Disease in the Young, and Stroke,
and the Quality of Care and Outcomes Research Interdisciplinary Working
Group; and the American College of Cardiology Foundation in Collaboration
with the Heart Rhythm Society. J Am Coll Cardiol 2006;47:473-84. Crossref
5. Ungar A, Mussi C, Del Rosso A, et al.
Diagnosis and characteristics of syncope in older patients referred to
geriatric departments. J Am Geriatr Soc 2006;54:1531-6. Crossref
6. Kenny RA, Traynor G. Carotid sinus
syndrome—clinical characteristics in elderly patients. Age Ageing
1991;20:449-54. Crossref
7. McIntosh SJ, Lawson J, Kenny RA.
Clinical characteristics of vasodepressor, cardioinhibitory, and mixed
carotid sinus syndrome in the elderly. Am J Med 1993;95:203-8. Crossref
8. Davies AJ, Steen N, Kenny RA. Carotid
sinus hypersensitivity is common in older patients presenting to an
accident and emergency department with unexplained fall. Age Ageing
2001;30:289-93. Crossref
9. Rutan GH, Hermanson B, Bild DE, Kittner
SJ, LaBaw F, Tell GS. Orthostatic hypotension in older adults. The
Cardiovascular Health Study. CHS Collaborative Research Group.
Hypertension 1992;19(6 Pt 1):508-19. Crossref
10. Ooi WL, Barrett S, Hossain M,
Kelley-Gagnon M, Lipsitz LA. Patterns of orthostatic blood pressure change
and their clinical correlates in a frail, elderly population. JAMA
1997;277:1299-304. Crossref
11. Freeman R, Wieling W, Axelrod FB, et
al. Consensus statement on the definition of orthostatic hypotension,
neutrally mediated syncope and the postural tachycardia syndrome. Auton
Neurosci 2011;161:46-8. Crossref
12. Kamaruzzaman S, Watt H, Carson C,
Ebrahim S. The association between orthostatic hypotension and medication
use in British women’s heart and health study. Age Ageing 2010;39:51-6. Crossref
13. Poon IO, Braun U. High prevalence of
orthostatic hypotension and its correlation with potentially causative
medications among elderly veterans. J Clin Pharm Ther 2005;30:173-8. Crossref
14. Zou X, Cao J, Li JH, et al. Prevalence
of and risk factors for postprandial hypotension in older Chinese men. J
Geriatr Cardiol 2015;12:600-4.
15. Lipsitz LA, Pluchino FC, Wie JY, Rowe
JW. Syncope in institutionalized elderly: the impact of multiple
pathological conditions and situational stress. J Chronic Dis
1986;39:619-30. Crossref
16. Jansen RW, Lipsitz LA. Postprandial
hypotension: epidemiology, pathophysiology, and clinical management. Ann
Intern Med 1995;122:286-95. Crossref
17. Vloet LC, Pel-Little RE, Jansen PA,
Jansen RW. High prevalence of postprandial and orthostatic hypotension
among geriatric patients admitted to Dutch hospitals. J Gerontol A Biol
Sci Med Sci 2005;60:1271-7. Crossref
18. Puisieux F, Bulckaen H, Fauchais AL,
Drumez S, Salomez-Granier F, Dewailly P. Ambulatory blood pressure
monitoring and postprandial hypotension in elderly persons with falls or
syncopes. J Gerontol A Biol Sci Med Sci 2000;55:M535-40. Crossref
19. Luciano GL, Brennan MJ, Rothberg MB.
Postprandial hypotension. Am J Med 2010;123:281.e1-6. Crossref
20. Galizia G, Abete P, Mussi C, et al.
Role of early symptoms in assessment of syncope in elderly people: results
from the Italian group for the study of syncope in the elderly. J Am
Geraitr Soc 2009;57:18-23. Crossref
21. Iivanainen AM, Lindroos M, Tilvis R,
Heikklä J, Kupari M. Natural history of aortic valve stenosis of varying
severity in the elderly. Am J Cardiol 1996;78:97-101. Crossref
22. Kapoor W, Snustad D, Peterson J,
Wieand HS, Cha R, Karpf M. Syncope in the elderly. Am J Med
1986;80:419-28. Crossref
23. Edvardsson N, Frykman V, van Mechelen
R, et al. Use of an implantable loop recorder to increase the diagnostic
yield in unexplained syncope: results from the PICTURE registry. Europace
2011;13:262-9. Crossref
24. Chen LY, Gersh BJ, Hodge DO, Wieling
W, Hammill SC, Shen WK. Prevalence and clinical outcomes of patients with
multiple potential causes of syncope. Mayo Clin Proc 2003;78:414-20. Crossref
25. Lipsitz LA. Altered blood pressure
homeostasis in advancing age: clinical and research implications. J
Gerontol 1989;44:M179-83. Crossref
26. Bauer JH. Age-related changes in the
renin-aldosterone system, Physiological effect and clinical implication.
Drugs Aging 1993;3:238-45. Crossref
27. Davis KM, Fush LC, Minaker KL, Elahi
D. Atrial natriuretic peptide levels in the elderly: differentiating
normal aging changes from disease. J Gerontol A Biol Sci Med Sci
1996;51:M95-101. Crossref
28. Bristow JD, Honour AJ, Pickering GW,
Sleight P, Smith HS. Diminished baroreflex sensitivity in high blood
pressure. Circulation 1969;39:48-54. Crossref
29. Strandgaard S. Autoregulation of
cerebral blood flow in hypertensive patients. The modifying influence of
prolonged antihypertensive treatment on the tolerance to acute,
drug-induced hypotension. Circulation 1976;53:720-7. Crossref
30. Brown KA, Maloney JD, Smith CH,
Haritzler GO, Ilstrup DM. Carotid sinus reflex in patients undergoing
coronary angiography: relationship of degree and location of coronary
artery disease to response to carotid sinus massage. Circulation
1980;62:697-703. Crossref
31. Hajjar I. Postural blood pressure
changes and orthostatic hypotension in the elderly patient: impact of
antihypertensive medications. Drugs Aging 2005;22:55-68. Crossref
32. Masuo K, Mikami H, Ogihara T, Tuck ML.
Changes in frequency of orthostatic hypotension in elderly hypertensive
patients under medications. Am J Hypertens 1996;9:263-8. Crossref
33. Yap YG, Camm AJ. Drug induced QT
prolongation and torsades de pointes. Heart 2003;89:1363-72. Crossref
34. Stuempfle KJ, Drury DG. The
physiological consequences of bed rest. J Exerc Physiol Online
2007;10:32-41.
35. Alshekhlee A, Shen WK, Mackall J,
Chelimsky TC. Incidence and mortality rates of syncope in the United
States. Am J Med 2009;122:181-8. Crossref
36. Racco F, Sconocchini C, Alesi C,
Zappelli L, Pratillo G. Long-term follow-up after syncope. A group of 183
patients observed for 5 years [in English, Italian]. Minerva Cardioangiol
2000;48:69-78.
37. Ungar A, Galizia G, Morrione A, et al.
Two-year morbidity and mortality in elderly patients with syncope. Age
Ageing 2011;40:696-702. Crossref
38. Kapoor WN. Evaluation and outcome of
patients with syncope. Medicine (Baltimore) 1990;69:160-75. Crossref
39. Ricci F, Fedorowski A, Radico F, et
al. Cardiovascular morbidity and mortality related to orthostatic
hypotension: a meta-analysis of prospective observational studies. Eur
Heart J 2015;36:1609-17. Crossref
40. Kapoor WN, Hanusa BH. Is syncope a
risk factor for poor outcomes? Comparison of patients with and without
syncope. Am J Med 1996;100:646-55. Crossref
41. Middlekauff HR, Stevenson WG,
Stevenson LW, Saxon LA. Syncope in advanced heart failure: high risk of
sudden death regardless of origin of syncope. J Am Coll Cardiol
1993;21:110-6. Crossref
42. Ruwald MH, Hansen ML, Lamberts M, et
al. Comparison of incidence, predictors, and the impact of co-morbidity
and polypharmacy on the risk of recurrent syncope in patients <85 years
versus ≥85 years of age. Am J Cardiol 2013;112:1610-5. Crossref
43. Kenny RA, Bhangu J, King-Kallimanis
BL. Epidemiology of syncope/collapse in younger and older Western patient
populations. Prog Cardiovasc Dis 2013;55:357-63. Crossref
44. van Dijk N, Sprangers MA, Boer KR,
Colman N, Wieling W, Linzer M. Quality of life within one year following
presentation after transient loss of consciousness. Am J Cardiol
2007;100:672-6. Crossref
45. O’Dwyer C, Bennett K, Langan Y, Fan
CW, Kenny RA. Amnesia for loss of consciousness is common in vasovagal
syncope. Europace 2011;13:1040-5. Crossref
46. Rubenstein LZ, Josephson KR. The
epidemiology of falls and syncope. Clin Geriatr Med 2002;18:141-58. Crossref
47. Guideline for the prevention of falls
in older persons. American Geriatric Society, British Geriatrics Society,
and American Academy of Orthopaedic Surgeons Panel on Falls Prevention. J
Am Geriatr Soc 2001;49:664-72.
48. Kenny RA, Parry SW. Syncope-related
falls in the elderly. J Geriatr Cardiol 2005;2:74-83.
49. Fried LP, Tang CM, Walston J, et al.
Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci
Med Sci 2001;56:M146-56. Crossref
50. Wolff JL, Starfield B, Anderson G.
Prevalence, expenditures, and complication of multiple chronic conditions
in the elderly. Arch Intern Med 2002;162:2269-76. Crossref
51. Wong CH, Weiss D, Sourial N, et al.
Frailty and its association with disability and comorbidity in a
community-dwelling sample of seniors in Montreal: a cross-sectional study.
Aging Clin Exp Res 2010;22:54-62. Crossref
52. Shen WK, Sheldon RS, Benditt DG, et
al. 2017 ACC/AHA/HRS guideline for the evaluation and management of
patients with syncope: a report of the American College of
Cardiology/American Heart Association Task Force on Clinical Practice
Guidelines and the Heart Rhythm Society. J Am Coll Cardiol
2017;70:e39-110. Crossref
53. van Dijk N, Boer KR, Colman N, et al.
High diagnostic yield and accuracy of history, physical examination, and
ECG in patients with transient loss of consciousness in FAST: the Fainting
Assessment study. J Cardiovasc Electophysiol 2008;19:48-55.
54. Rubenstein LZ, Struck AE, Siu AL,
Wieland D. Impacts of geriatric evaluation and management programs on
defined outcomes: overview of the evidence. J Am Geriatr Soc 1991;39(9 Pt
2):8S-16S. Crossref