Hong Kong Med J 2018 Apr;24(2):128–36 | Epub 4 Apr 2018
DOI: 10.12809/hkmj176960
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE
Effect of a financial incentive on the acceptance of a
smoking cessation programme with service charge: a cluster-controlled
trial
KS Wong, MB, BS1; SN Fu, MB, BS, MFM2;
KL Cheung, MB, ChB2; MC Dao, MB, BS2; WM Sy, MB, BS2
1 Family Medicine and General
Out-patient Clinics, Kowloon Central Cluster, Hospital Authority, Hong
Kong
2 Family Medicine & Primary Health
Care, Kowloon West Cluster, Hospital Authority, Hong Kong
Corresponding author: Dr KS Wong (wks638@ha.org.hk)
Abstract
Introduction: Frontline health
care professionals in Hong Kong may encounter high refusal rates for the
Hospital Authority’s Smoking Counselling and Cessation Programme (SCCP)
when smokers know it is subject to a service charge. We compared SCCP
booking and attendance rates among smokers with or without a financial
incentive.
Methods: In this multicentre
non-randomised cluster-controlled trial, adult smokers who attended one
of six general out-patient clinics between November 2015 and April 2016
were invited to join an SCCP. Attendees in the three intervention-group
centres but not the three control-group centres received a supermarket
coupon to offset the service charge.
Results: A total of 173 smokers
aged 18 years or older (92 in the intervention group and 81 in the
control group) were recruited into the study. In the intervention group,
47 smokers (51%) agreed via a questionnaire that they would join the
SCCP, compared with only 23 smokers in the control group (28%). The
booking rates were 83% (n=39) in the intervention group and 83% (n=19)
in the control group. Among those who had booked a place, 19 (49%)
intervention-group participants and 11 (58%) control-group participants
attended an SCCP session. Multivariable logistic regression revealed
that offering a coupon was associated with agreeing to join an SCCP
(odds ratio=4.963, 95% confidence interval=2.173-11.334; P<0.001) and
booking an SCCP place (odds ratio=4.244, 95% confidence
interval=1.838-9.799; P<0.001).
Conclusion: Provision of a
financial incentive was positively associated with agreement to join an
SCCP and booking an SCCP place. Budget holders should consider providing
the SCCP free of charge to increase smokers’ access to the
service.
New knowledge added by this study
- This study reveals that provision of a financial incentive to offset the service charge of the Smoking Counselling and Cessation Programme in Hong Kong might increase the proportion of smokers who agree to join the programme and make an appointment.
- Budget holders should consider providing a free Smoking Counselling and Cessation Programme to increase smokers’ access to the service.
Introduction
There is no doubt that smoking is a serious hazard
to health.1 2 3 One in two
smokers will be killed by smoking; if one can help two smokers to quit, at
least one life will be saved.4
Individual counselling by trained therapists can assist smokers to quit.5 6
7 The counselling usually involves
review of the participant’s smoking history and motivation to quit,
provision of problem-solving strategies to deal with high-risk situations,
and encouragement. Smokers who receive individual counselling are 39% more
likely to cease smoking in the long term than smokers who receive minimal
behavioural intervention.5 Another
method to increase the smoking cessation rate is nicotine replacement
therapy (NRT). Such therapy (eg, gum, transdermal patch, and lozenges) is
cost-effective in smoking cessation and increases the rate of quitting by
50% to 70%.8 9 10 11 Combining counselling and pharmacotherapy has been
shown to further increase smoking cessation success rates by more than 80%
when compared with minimal intervention or usual care.12 If a smoker quits smoking in the absence of external
assistance, there is only a 3% to 5% chance of sustained abstinence at 6
to 12 months.13
In Hong Kong, the Smoking Counselling and Cessation
Programme (SCCP) consists of individual counselling and provision of NRT
and is available from the Hospital Authority; similar services are also
provided by the Department of Health and the Tung Wah Group of Hospitals.14 The Hospital Authority operates
58 smoking cessation and counselling centres. Despite this available
support, only about 19% of current smokers in Hong Kong have tried a
smoking cessation service.15 In
contrast, the prevalence of assisted quit attempts was 59.4% in Australia
in 2008-2009 and 53.6% in the United Kingdom in 2010.16
The SCCP in Hong Kong is offered as part of chronic
care, and general out-patient clinics (GOPCs) provide a good opportunity
for health care professionals to refer smokers to an SCCP. Frontline GOPC
health care professionals in Hong Kong may encounter high refusal rates of
SCCP service when smokers know they must pay a service charge. Currently,
smoking cessation and counselling centres SCCC charge HK$50 [~US$6.40]
(HK$45 [~US$5.80] at the time of this study) for an initial face-to-face
consultation, unless the client is exempt (eg, those receiving the
Comprehensive Social Security Allowance or civil servants). There is no
extra charge for NRT.
A review article in the Cochrane Library by Reda et
al17 proposed that if all costs to smokers are covered, the proportion of
smokers who attempt to quit, use smoking cessation treatments, and succeed
in quitting will significantly increase compared with provision of no
financial support. Reda et al17
also suggested that even though the absolute differences in quitting were
small when an intervention group was compared with a control group (total
events: 134 of 1409 vs 75 of 1351, respectively), the costs per person
successfully quitting were low or moderate (US$119 to US$6450). However,
all the studies included in that review were conducted in western
countries, where the health care financing systems may differ from that of
Hong Kong. In this study, we aimed to determine whether the booking and
attendance rates at a smoking cessation service (SCCP) in a primary care
setting could be increased if the patient received a financial incentive,
as payment-in-kind, to offset the service fee.
Methods
Study design and population
This was a multicentre non-randomised
cluster-controlled trial involving six GOPCs of the Hong Kong Hospital
Authority’s Kowloon West Cluster and conducted from November 2015 to April
2016. The study protocol was approved by the Hospital Authority Kowloon
West Cluster Research Ethics Committee (Ref No. KW/EX-15-169(91-08)).
Non-random cluster sampling was used to choose participating clinics and
assign them to study group, in order to avoid contamination of
participants between the intervention and control groups. Three clinics
(Ha Kwai Chung GOPC, West Kowloon GOPC, and Tsing Yi Cheung Hong GOPC)
were assigned to the intervention group and three (Cheung Sha Wan GOPC, Li
Po Chun GOPC, and South Kwai Chung GOPC) to the control group. A standard
regular SCCP was available at all six clinics. The SCCP counsellors were
trained nurses or pharmacists and all underwent the same smoking cessation
counselling training provided by the Hospital Authority Head Office. The
GOPC staff and SCCP counsellors were not involved in clinic selection or
assignment.
The study centres were six of the 73
government-funded primary care GOPCs, and the majority of their patients
were from a lower socio-economic class or older patients with chronic
illnesses. The patient profiles from the six GOPCs shared a similar
socio-demographic background and disease profile. There was no pre-study
SCCP booking rate available, but the total number of smokers recruited
from the three control clinics into the SCCP during the study period was
similar to the number of SCCP referrals made by the three clinics during
an equivalent period in the previous year (November 2014 to April 2015).
The attendance rate for booked SCCP appointments was logged by the clinic
computer system and was 50% to 60% among all six clinics.
Convenience sampling was used to recruit current
smokers at the time of recruitment,15
who were identified during a doctor’s consultation or nurse’s assessment
during the daytime. Information about this study and possible recruitment
of patients for SCCP referral was given to doctors and nurses before the
start of the study. After valid consent had been obtained, participants
were invited to complete a questionnaire to provide background
information, smoking status, and decision to join an SCCP. Assistance was
given with the questionnaire if required. The questionnaires distributed
to the control group (online supplementary Appendix 1) and the intervention group (online
supplementary Appendix 2) stated the usual SCCP service charge of
HK$45. The intervention group’s questionnaire additionally stated that a
HK$50 supermarket coupon would be given to SCCP attendees. Those who
agreed to participate in the SCCP were directed to make an appointment via
the registration counter.
The SCCP counsellors in the intervention group were
briefed by the authors about the process of issuing a supermarket coupon
as payment in-kind to SCCP attendees. The SCCP session was carried out as
usual, regardless of study group. In clinics in the intervention group,
the supermarket coupon was given to SCCP participants after payment of the
service charge.
Inclusion and exclusion criteria
Current smokers who were aged 18 years or older
were eligible for the study. Participants were excluded if (1) the SCCP
service charge was waived—for example, if they were a Comprehensive Social
Security Allowance recipient or a civil servant; (2) they were as mentally
incapacitated and unable to give consent; or (3) they were pregnant, as
there was concern that NRT may increase the risk of congenital respiratory
anomalies.18
Recruitment questionnaire
A structured questionnaire in traditional Chinese
script (online supplementary Appendices 1 and 2) was used to collect the
following information:
(1) Age, sex, mean personal monthly income, and
whether the participant thought the clinic was a convenient place to go;
(2) Smoking history: age when starting smoking,
number of years of smoking, the mean number of cigarettes consumed per day
(CPD), and time to the first cigarette of the day (TTFC) after waking. The
nicotine dependence level was measured by CPD and TTFC, which have been
shown to be independent predictors of quitting outcome.19 A categorical scoring method has been deemed adequate
for many purposes19 and was
adopted in this study (CPD categories of 0-10, 11-20, 21-30, and ≥31; TTFC
categories of ≤5, 6-30, 31-60, and ≥61 minutes);
(3) Rating (range, 0-10) of perceived importance
of, readiness for, and confidence in smoking cessation, which have been
reported to be associated with smoking behavioural change20;
(4) If the smoker agrees to join the SCCP.
The questionnaire comprised 14 questions. The
relevance and content validity of the questionnaire were reviewed by
senior doctors. It was also pilot-tested in 10 smokers for face validity.
Outcome measures
The rates of agreement between questionnaire
response rate for intention to book an SCCP appointment, actual SCCP
booking rate via the registration counter, and SCCP attendance rate were
compared between the intervention and control groups. Defaulters or
participants who rescheduled their SCCP sessions outside the study period
were treated as non-attendees. Smokers who joined the SCCP were followed
up by telephone by smoking-cessation counsellors on the seventh day after
the first consultation to enquire whether they had quit smoking and were
not smoking on the day of the call. This is a standard outcome measure of
the SCCP used by the Hospital Authority.
Sample-size calculation
The sample size was based on the annual quit rate
of smokers in 2014 (of 9.6%) for all GOPCs under the Hospital Authority,
according to an internal report. In a Cochrane review of health care
financing systems to increase the uptake of tobacco-dependence treatment,
full financial interventions (ie, covering all costs) directed at smokers
could increase abstinence rate at 6 months or longer by 2.45 times that of
smokers with no financial intervention (risk ratio=2.45, 95% confidence
interval [CI]=1.17-5.12, I2=59%, 4 studies).17 In a study by Kaper et al,21
the adjusted odds ratio for abstinence after reimbursement was 2 to 4
times that after no reimbursement. It was thus estimated that offering
reimbursement to attend an SCCP would triple the programme attendance
rate. Using the formula established by Casagrande et al,22 65 participants were required in each group in order
to obtain an alpha of 0.05 and 80% power. Assuming a 20% attrition rate,
80 participants were required in each group.
Statistical analysis
Data analysis was performed with SPSS (Windows
version 20.0; IBM Corp, Armonk [NY], United States). The level of
significance was set at 5%. Data of the intervention and the control
groups were summarised by descriptive statistics. Categorical variables
were expressed as percentages and compared between the two groups by
Pearson’s chi-square test or Fisher’s exact test. Continuous variables
were tested for normality with Shapiro-Wilk’s test. Normally distributed
variables were expressed as means with standard deviations and compared
with Student’s t test. Variables that were non-normally
distributed were presented as medians with interquartile ranges and
compared with the Mann-Whitney U test. The association between
participants’ characteristics, reimbursement, and outcomes were studied by
univariate logistic regression analysis and multivariable logistic
regression analysis using backward elimination, yielding crude odds ratios
(ORs) and 95% CIs. Intention-to-treat analysis was used, and missing data
were handled by listwise deletion.
Results
Participant recruitment
In the control group clinics, a total of 90 smokers
were approached, of whom two refused to participate in the study (response
rate, 98%). Seven were excluded, as their questionnaires were incomplete
or their SCCP fee would have been waived. In the intervention group
clinics, a total of 151 smokers were approached, of whom 28 refused to
participate in the study (response rate, 81%). Thirty-one were excluded,
as their questionnaires were incomplete or their SCCP fee would have been
waived. There were 81 and 92 smokers (total, 173) recruited into the
control group and intervention group, respectively.
Study population characteristics
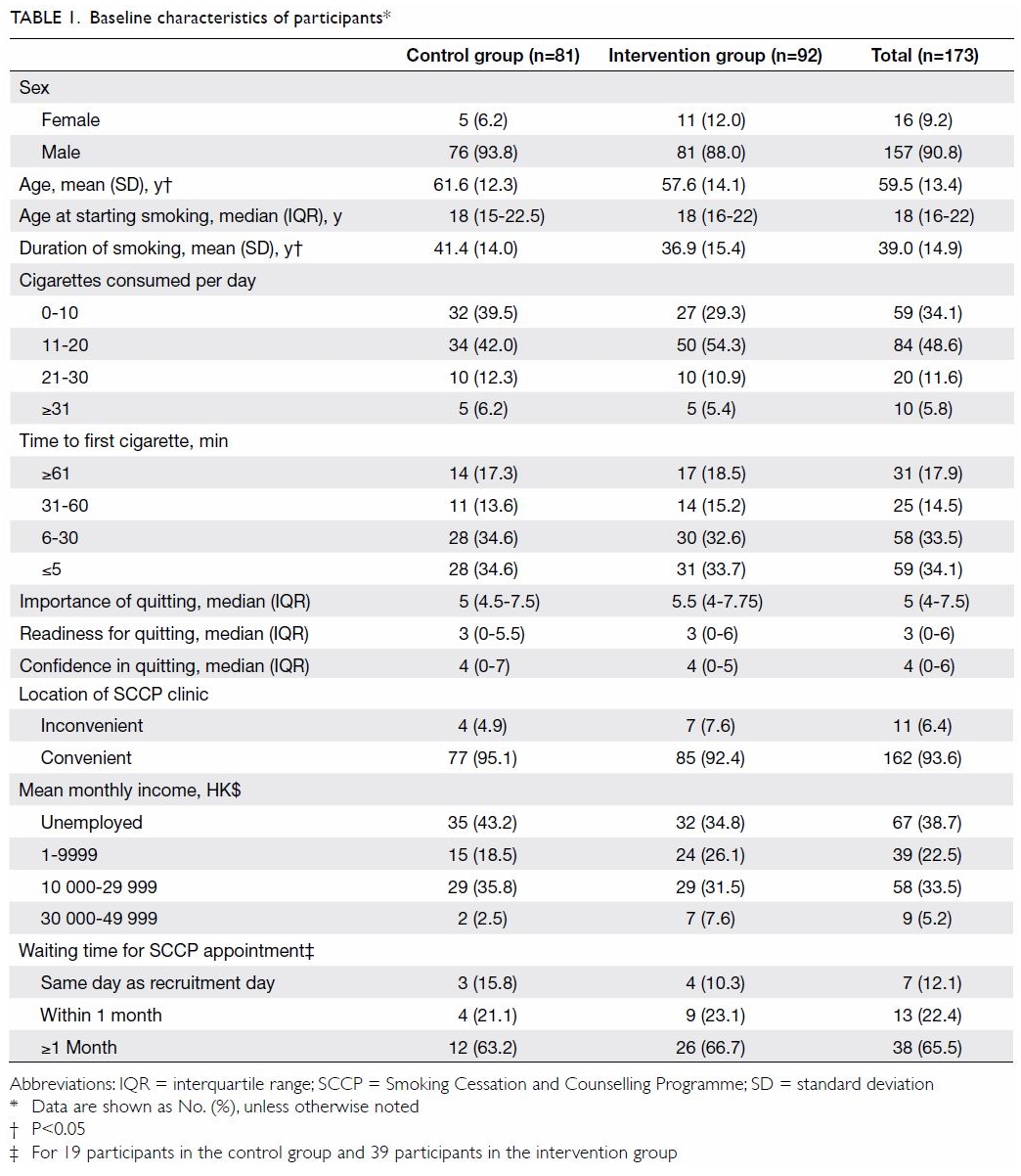
There was no statistical difference between the two
groups in terms of sex; age when starting smoking; mean cigarette
consumption per day; TTFC; perceived importance of, readiness for, and
confidence in smoking cessation; perceived convenience of clinic location;
mean monthly income; and waiting time for SCCP (Table 1). More than 90% of participants were male,
had a mean monthly income of <HK$30 000, and believed that the SCCP
clinic was conveniently located. The median age at starting smoking was 18
years. Nearly half of the smokers were medium smokers, consuming 11 to 20
CPD. The TTFC was less than 31 minutes for more than 67% of smokers. The
rating (from 0 to 10) of perceived importance of, readiness for, and
confidence in quitting was 5, 3, and 4, respectively. The waiting time for
an SCCP appointment was longer than 1 month for over 65% of participants.
The age and the duration of smoking of the
participants were statistically different between the two groups. The mean
age of the control group was 4 years older than that of the intervention
group (61.6 vs 57.6 years; P=0.048). The mean duration of smoking in the
control group was 4 years longer than that in the intervention group (41.4
vs 36.9 years; P=0.047).
Outcomes
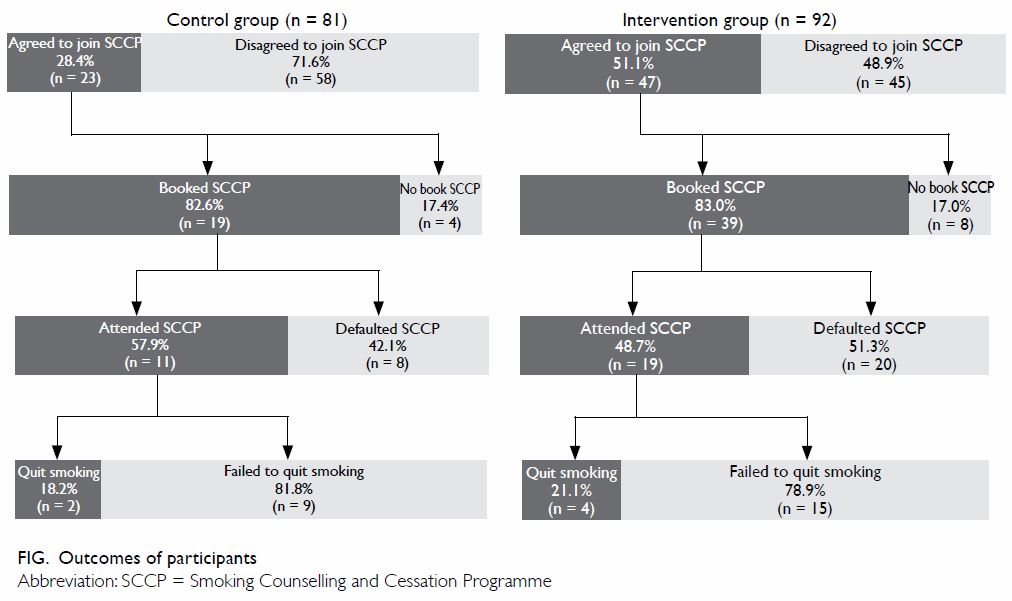
The Figure summarises the SCCP booking and attendance
rates. In the intervention group, 47 smokers (51%) indicated on the
questionnaire their agreement to join an SCCP, whereas only 23 smokers
(28%) did so in the control group. Of those who agreed in principle, 39
(83%) in the intervention group made a booking compared with only 19 (83%)
in the control group. For those who had booked an SCCP place, 19 (49%) and
11 (58%) attended the sessions in the intervention and control group,
respectively. Three smokers (16%) in the intervention group were lost to
follow-up and were counted as non-quitters. Four smokers (21%) in the
intervention group and two (18%) in the control group quit successfully by
the seventh day.
Univariate logistic regression analysis (Table
2) revealed that the financial intervention was associated with a
higher rate of agreeing to join an SCCP (OR=2.634, 95% CI=1.399-4.959;
P=0.003) and booking of an SCCP appointment (OR=2.401, 95% CI=1.242-4.644;
P=0.009), but not with attending an SCCP. Factors that were associated
with a higher rate of agreeing to join, booking, and attending an SCCP
session were consuming 11 to 20 CPD and higher ratings of perceived
readiness for and confidence in smoking cessation. Other factors that were
associated with a higher rate of agreeing to join and booking an SCCP
session were ≤5 minutes for TTFC and higher rating of perceived importance
of smoking cessation.
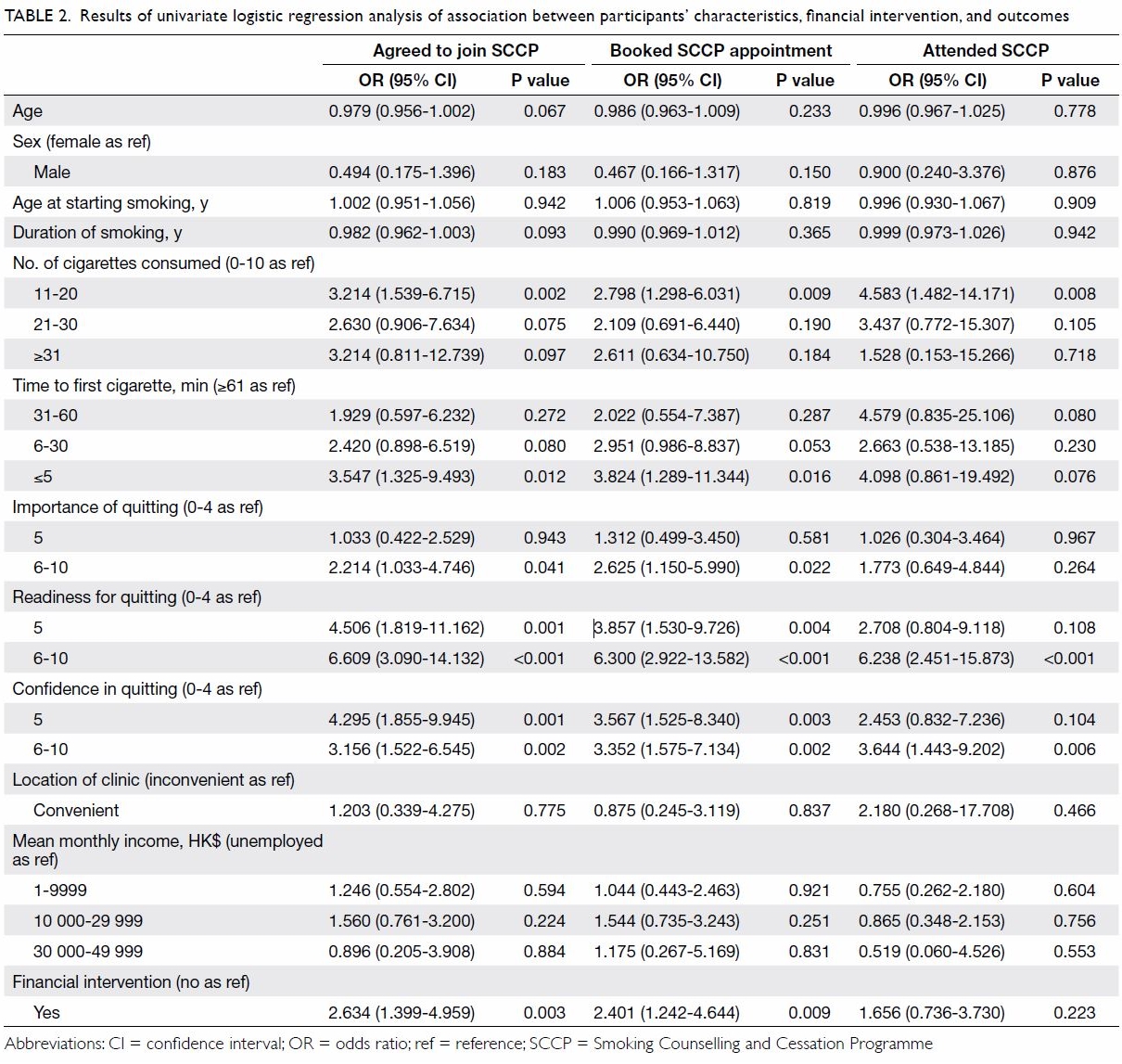
Table 2. Results of univariate logistic regression analysis of association between participants’ characteristics, financial intervention, and outcomes
Multivariable logistic regression analysis (Table
3) revealed that the financial intervention was associated with a
higher rate of agreeing to join an SCCP (OR=4.963, 95% CI=2.173-11.334;
P<0.001) and of booking an SCCP appointment (OR=4.244, 95%
CI=1.838-9.799; P<0.001), but not with actual attendance. Higher
ratings of smokers’ perceived readiness for smoking cessation was
associated with a higher rate of agreeing to join, booking, and attending
an SCCP session. Other factors that were associated with a higher rate of
agreeing to join an SCCP and making a booking were ≤5 minutes and 6-30
minutes of TTFC and a mean monthly income of HK$10 000-29 999. Mean
cigarette consumption of 11 to 20 CPD was associated with a higher rate of
attendance at an SCCP.
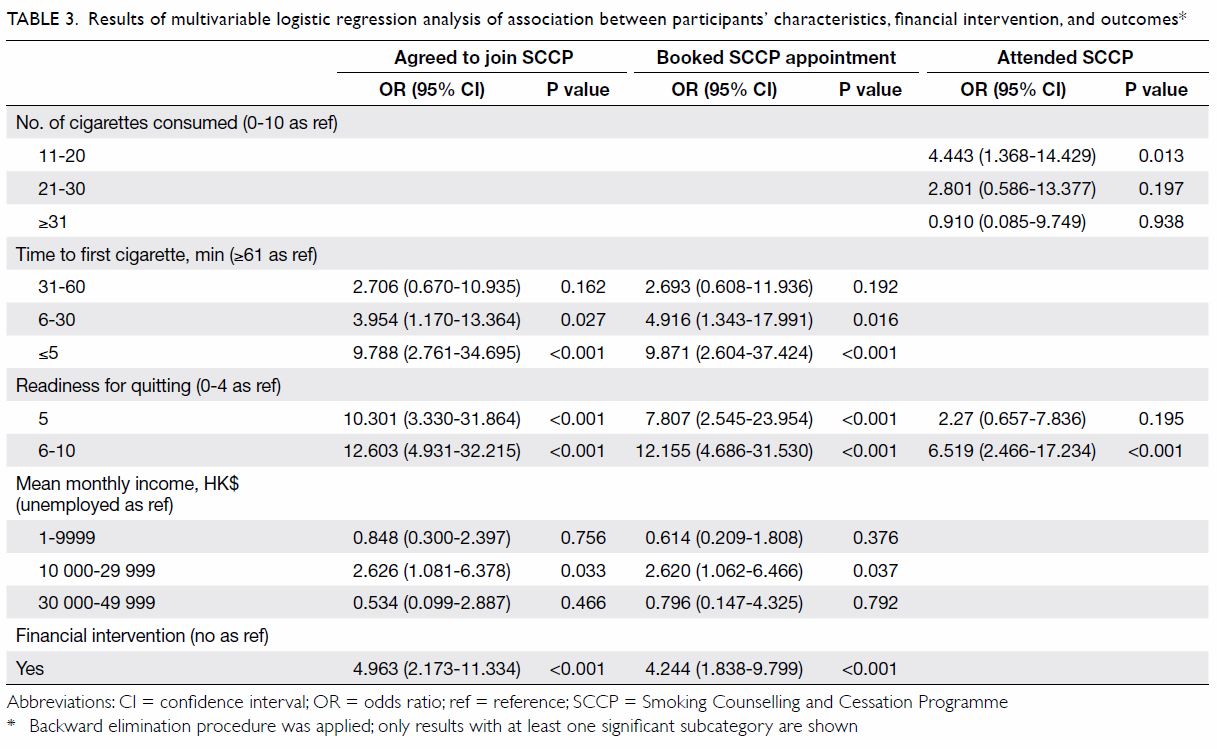
Table 3. Results of multivariable logistic regression analysis of association between participants’ characteristics, financial intervention, and outcomes
Discussion
In Hong Kong, there are so far no published data on
the effect of reimbursement on booking and attendance rates for smoking
cessation programmes. Overseas studies have evaluated the effect of
reimbursement on quitting attempts and abstinence rates, but not
attendance at smoking cessation services. This study provides some
insights into this area.
The participants in the control and intervention
group were comparable except for mean age (62 vs 58 years) and duration of
smoking (41 vs 37 years). Simply offsetting the HK$45 SCCP fee with a
HK$50 supermarket coupon significantly increased smokers’ willingness to
join or actually book an SCCP session (OR=4.963 and 4.244, respectively) [Table 3]. This finding suggests that a financial
intervention may make more smokers consider joining an SCCP. With further
counselling and NRT in the SCCP, the road to successful smoking cessation
may be shortened.
The lack of an association between attendance rate
and reimbursement might be explained by the waiting time for SCCP (Table
4). Owing to human resource constraints, more than 65% of SCCP
appointments had to be scheduled for over a month after participant
recruitment. The mean waiting time was 37 days for the intervention group
and 33 days for the control group. The attendance rate dropped from 69% to
37% when the appointment date was over a month away. This finding was in
keeping with an overseas study that reported long waiting times as one of
the reasons for non-attendance at a quitting programme.23 Future local studies might involve exploring the
reasons for programme non-attendance and would help service providers to
improve the SCCP and help more smokers quit.
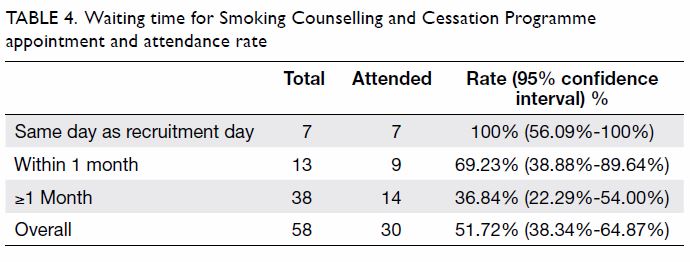
Table 4. Waiting time for Smoking Counselling and Cessation Programme appointment and attendance rate
In a local evaluative study of the integrated
smoking cessation services of the Tung Wah Group of Hospitals in 2011, the
majority of clients (52.6%) consumed 11-20 CPD.24
More than half (54.4%) of those who attended smoking cessation clinics of
the Tung Wah Group of Hospitals had a high dependency on nicotine.24 In agreement, our study found that smokers consuming
11-20 CPD were significantly more likely to attend an SCCP than lighter
smokers (OR=4.443). We also found that smokers with shorter TTFC were
significantly more likely to agree to join or book an SCCP session (TTFC
≤5 minutes: OR=9.788 and 9.871, respectively; TTFC 6-30 minutes: OR=3.954,
and OR=4.916, respectively).
Individuals in the quitting preparation stage
display the highest motivation-ruler ratings.20
In our study, smokers with a higher rating of readiness were more likely
to have a higher rate of deciding to join, book, or attend an SCCP (Table
3). This finding indicates that smokers who were recruited to join
an SCCP were prepared to quit. Concerns that offering a financial
incentive might invite smokers who had no genuine intention to quit are
unfounded. Offering help to smokers for quitting was one of the MPOWER
(Monitor, Protect, Offer, Warn, Enforce, and Raise) measures described by
the World Health Organization to combat the global tobacco epidemic.25 Hong Kong is fortunate to have a well-established
smoking cessation programme, so the service deserves to be fully used.
Limitations
The smokers recruited into this study were a
convenience sample of attendees at GOPCs, so their characteristics would
differ from those of the general smoking population in Hong Kong15 in terms of a larger proportion of males (90.8% vs
83.9%), higher daily cigarette consumption (48.6% consuming 11-20 CPD vs
56.0% consuming 1-10 CPD), and larger proportion of economically inactive
smokers (38.7% vs 21.0%). The results thus may not be generalised to the
whole population of Hong Kong smokers. Furthermore, retirement and
economic inactivity may influence smoking habits26
and act as confounders, but these were not controlled in the multivariable
analyses.
The control and intervention groups were not very
comparable: the control group was slightly older and had smoked for
slightly longer. Estimation of the sample size was suboptimal, as the
total numbers of eligible smokers during the recruitment period and the
estimated increase in attendance rate by financial incentives were not
available before the study. Sample-size estimation was based on abstinence
rates from previous studies instead of attendance rates. The number of
participants who actually attended (19+11=30) may be too small to show any
statistical difference between SCCP attendance rates because the
difference was less than the three-fold increase for the sample-size
calculation.
In addition, the SCCP service in some clinics was
restricted to certain days or times of the week owing to availability of
counsellors. Some smokers, especially those who were working, may not have
been able to find a session at a convenient time. This situation could
have affected the booking and attendance rate between different clinics.
In one of the returned questionnaires in which the participant ticked the
box “agree to join SCCP” but did not make a booking, there was a written
remark in Chinese: “Time does not fit”.
This study was non-randomised and the doctors and
nurses were not blinded to the financial intervention, because of the
difficulty of running a complex workflow with limited resources. We
assumed all doctors and nurses tried their best to assist smokers to quit.
The possibility that those in the intervention group were more passionate
in persuading patients to quit smoking cannot be excluded. The assignment
of participants to the intervention or control group was not random and
may explain the differences in the baseline characteristics of
participants in the two groups. Moreover, it is unknown whether there
would be a difference in behaviour if free SCCP was offered from the
beginning, instead of providing a fixed-amount HK$50 supermarket coupon
that offered an extra HK$5. Only the 7-day quit rate was used as the final
programme outcome, as it was a standard outcome in the study centres.
Future research with a robust randomisation process may be considered, as
well as the use of longer abstinence periods such as 1 month, 3 months,
and 12 months.
Conclusion
This study revealed that provision of a financial
incentive that would indirectly cover the SCCP service fee might increase
the proportion of smokers who agree to attend and make a booking to attend
an SCCP. To reduce the barriers to accessing an SCCP service, budget
holders should consider providing free and timely SCCP to motivated
smokers. It is essential to catch smokers’ moment of hesitation and to
increase their access to the service.
Supplementary information
Online supplementary information (Appendices
1 and 2) is available for this article at www.hkmj.org.
Acknowledgements
We thank the Hong Kong College of Family Physicians
(HKCFP) for granting the HKCFP Trainee Research Fund 2015 for this study.
We also thank the doctors and nurses in Cheung Sha Wan GOPC, Ha Kwai Chung
GOPC, Li Po Chun GOPC, West Kowloon GOPC, South Kwai Chung GOPC, and Tsing
Yi Cheung Hong GOPC for participant recruitment; Drs LS Chu, T Fong, KM
Ho, and SY Tse for advice during research design; and Ms Ellen Yu and Mr
Edward Choi for their support during the statistical analyses.
Declaration
The authors have no conflicts of interest to
disclose.
References
1. National Center for Chronic Disease
Prevention and Health Promotion (US) Office on Smoking and Health. The
Health Consequences of Smoking—50 Years of Progress: a Report of the
Surgeon General. 2014. Available from:
http://www.ncbi.nlm.nih.gov/pubmed/24455788. Accessed 6 Jun 2016.
2. Lam TH, Ho SY, Hedley AJ, et al.
Mortality and smoking in Hong Kong: case-control study of all adult deaths
in 1998. BMJ 2001;323:361. Crossref
3. McGhee SM, Ho LM, Lapsley HM, et al.
Cost of tobacco-related diseases, including passive smoking, in Hong Kong.
Tob Control 2006;15:125-30. Crossref
4. Lam TH. Absolute risk of tobacco deaths:
one in two smokers will be killed by smoking: comment on “Smoking and
all-cause mortality in older people”. Arch Intern Med 2012;172:845-6. Crossref
5. Simon JA, Carmody TP, Hudes ES, et al.
Intensive smoking cessation counseling versus minimal counseling among
hospitalized smokers treated with transdermal nicotine replacement: a
randomized trial. Am J Med 2003;114:555-62. Crossref
6. Ibrahim MI, N.A. Magzoub NA, Maarup N.
University-based smoking cessation program through pharmacist-physician
initiative: an economic evaluation. J Clin Diagn Res 2016;10:LC11-5.
7. Lancaster T, Stead LF. Individual
behavioural counselling for smoking cessation. Cochrane Database Syst Rev
2005;(2)CD001292. Crossref
8. Cornuz J, Pinget C, Gilbert A, et al.
Cost-effectiveness analysis of the first-line therapies for nicotine
dependence. Eur J Clin Pharmacol 2003;59:201-6. Crossref
9. Wang D, Connock M, Barton P, et al. ‘Cut
down to quit’ with nicotine replacement therapies in smoking cessation: a
systematic review of effectiveness and economic analysis. Health Technol
Assess 2008;12:iii-iv, ix-xi, 1-135.
10. Etter JF, Stapleton JA. Nicotine
replacement therapy for long-term smoking cessation: a meta-analysis. Tob
Control 2006;15:280-5. Crossref
11. Stead LF, Perera R, Bullen C, et al.
Nicotine replacement therapy for smoking cessation. Cochrane Database Syst
Rev 2012;(11):CD000146. Crossref
12. Stead LF, Koilpillai P, Fanshawe TR,
et al. Combined pharmacotherapy and behavioural interventions for smoking
cessation. Cochrane Database Syst Rev 2016(3):CD008286. Crossref
13. Hughes JR, Keely J, Naud S, et al.
Shape of the relapse curve and long-term abstinence among untreated
smokers. Addiction 2004;99:29-38. Crossref
14. Hong Kong Council on Smoking and
Health. Smoking Cessation Service Providers in Hong Kong. Available from:
http://smokefree.hk/en/content/web.do?page=Services. Accessed 7 Jun 2015.
15. Census and Statistics Department,
Government of the Hong Kong Special Administrative Region. Thematic
Household Survey Report No. 59. Available from:
http://www.statistics.gov.hk/pub/B11302592016XXXXB0100.pdf. Accessed 1 Jul
2016.
16. Edwards SA, Bondy SJ, Callaghan RC, et
al. Prevalence of unassisted quit attempts in population-based studies: a
systemic review of the literature. Addict Behav 2014;39:512-9. Crossref
17. Reda AA, Kotz D, Evers SM, et al.
Healthcare financing systems for increasing the use of tobacco dependence
treatment. Cochrane Database Syst Rev 2012;(6):CD004305. Crossref
18. Dhalwani NN, Szatkowski L, Coleman T,
et al. Nicotine replacement therapy in pregnancy and major congenital
anomalies in offspring. Pediatrics 2015;135:859-67. Crossref
19. Borland R, Yong HH, O’Connor R, et al.
The reliability and predictive validity of the Heaviness of Smoking Index
and its two components: findings from the International Tobacco Control
Four Country study. Nicotine Tob Res 2010;12 Suppl:S45-50. Crossref
20. Boudreaux ED, Sullivan A, Abar B, et
al. Motivation rulers for smoking cessation: a prospective observational
examination of construct and predictive validity. Addict Sci Clin Pract
2012;7:8. Crossref
21. Kaper J, Wagena EJ, Willemsen MC, et
al. A randomized controlled trial to assess the effects of reimbursing the
costs of smoking cessation therapy on sustained abstinence. Addiction
2006;101:1656-61. Crossref
22. Casagrande JT, Pike MC, Smith PG. An
improved approximate formula for calculating sample sizes for comparing
two binomial distributions. Biometrics 1978;34:483-6. Crossref
23. Sharp DJ, Hamilton W. Non-attendance
at general practices and outpatient clinics: Local systems are needed to
address local problems. BMJ 2001;323:1081-2. Crossref
24. Chan SC, Leung YP, Chan CH, et al. An
Evaluative Study of the Integrated Smoking Cessation Services of Tung Wah
Group of Hospitals. Tung Wah Group of Hospitals. 2011. Available from:
http://icsc.tungwahcsd.org/file/evaluative_study.pdf. Accessed 1 Jul 2016.
25. World Health Organization. WHO Report
on the Global Tobacco Epidemic, 2015: Raising Taxes on Tobacco. Available
from:
http://apps.who.int/iris/bitstream/10665/178574/1/9789240694606_eng.pdf?ua=12015.
Accessed 1 Jul 2016.
26. Lang IA, Rice NE, Wallace RB, et al.
Smoking cessation and transition into retirement: analyses from the
English longitudinal study of ageing. Age Ageing 2007;36:638-43. Crossref