DOI: 10.12809/hkmj166276
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
CASE REPORT
Mesenteric fibromatosis: a rare cause of peritonitis
Eugene PL Ng, MB, ChB, MRCSEd1; SY
Kwok, MB, ChB, FHKAM (Surgery)1; KF Lok, MB, ChB, FRCPath2;
MP Chow, MB, BS, FHKAM (Surgery)1; Patrick YY Lau, MB, BS,
FHKAM (Surgery)1
Departments of 1Surgery and 2Pathology,
Kwong Wah Hospital, Yaumatei, Hong Kong
Corresponding author: Dr Eugene PL Ng (eugeneg1@hotmail.com)
Case presentation
A 65-year-old Chinese man presented with a 2-day
history of left-sided abdominal pain with fever and watery diarrhoea in
February 2016. Systemic enquiry was unremarkable and he had no recent
travel or contact history. On admission, his blood pressure was 127/67 mm
Hg, pulse rate was 110 beats/min, and body temperature was 37.8ºC.
Abdominal examination revealed peritoneal signs over the left side of the
abdomen and evidence of a tender irregular firm mass. There was no
organomegaly or ascites. Blood tests demonstrated leukocytosis with white
cell count of 11.8 × 109 /L but findings were otherwise normal.
Both chest and abdominal X-rays were unremarkable.
Urgent contrast-enhanced computed tomography (CT)
of the abdomen and pelvis revealed a circumscribed mass (10.2 cm x 11.1 cm
x 10.3 cm) located in the left abdominal cavity that could not be
delineated from adjacent small bowel loops. A 1.6-cm thick layer of
rim-enhancing collection with gas density was closely related to the left
posterolateral aspect of the mass and there was a small amount of
peritoneal fluid at the pelvic and left side of the abdominal cavity (Fig
1a and 1b). Radiological features were consistent with a
gastrointestinal stromal tumour (GIST) complicated by abscess formation.
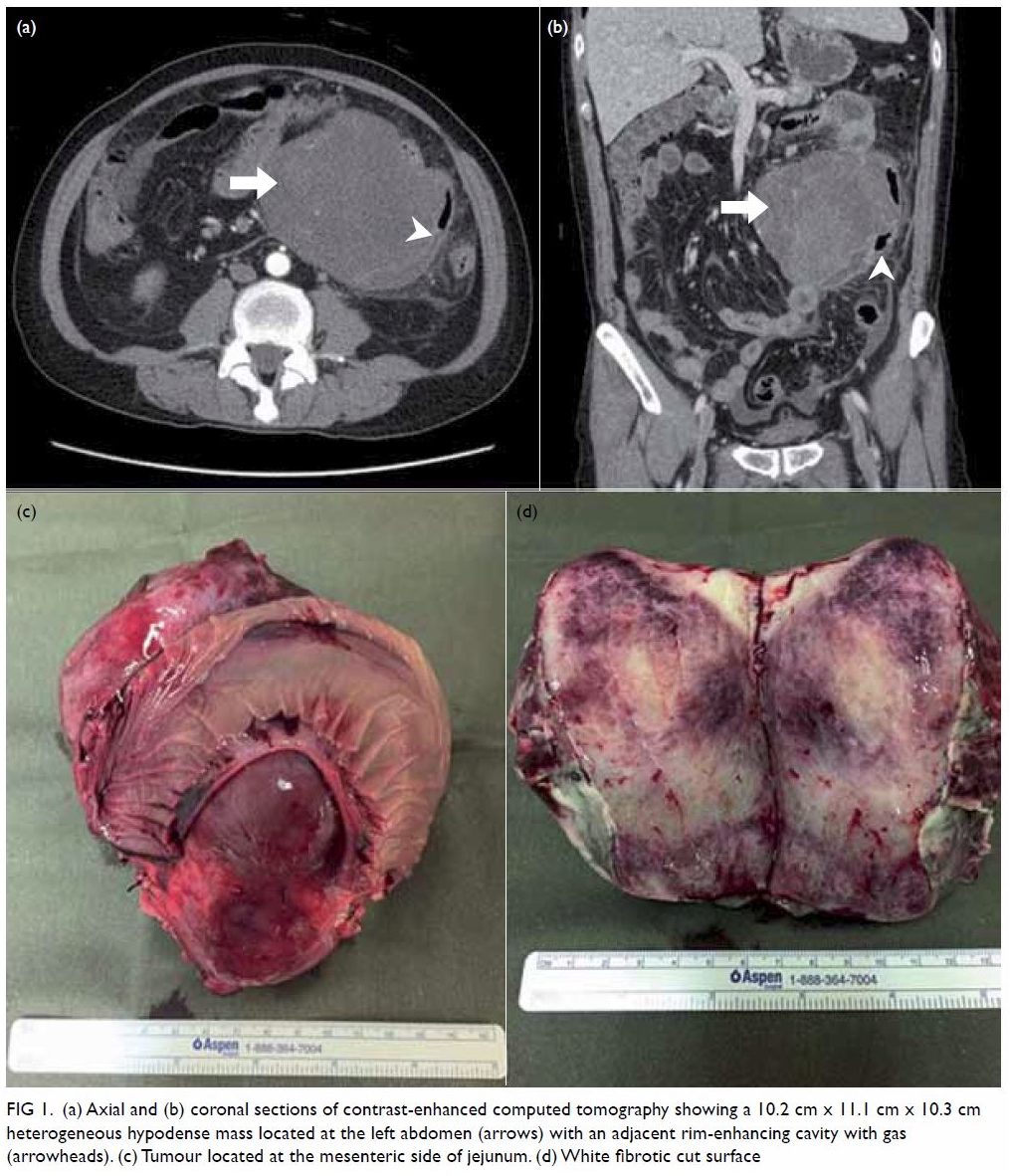
Figure 1. (a) Axial and (b) coronal sections of contrast-enhanced computed tomography showing a 10.2 cm x 11.1 cm x 10.3 cm heterogeneous hypodense mass located at the left abdomen (arrows) with an adjacent rim-enhancing cavity with gas (arrowheads). (c) Tumour located at the mesenteric side of jejunum. (d) White fibrotic cut surface
Broad-spectrum empirical antibiotic was started and
emergency laparotomy was arranged. At laparotomy, there was generalised
peritonitis with purulent peritoneal fluid. An 11 cm x 13 cm tumour was
found at the mesenteric side of the proximal jejunum which had ruptured
with abscess formation. The tumour involved the jejunal wall but there was
no mucosal lesion (Fig 1c). Laparotomy was otherwise unremarkable.
En-bloc resection of the tumour with the adjacent jejunum was performed
followed by primary anastomosis.
Gross examination showed a multinodular tumour with
an area of purulent material on the surface at the serosa, measuring up to
11 cm in diameter. The tumour showed a fibrotic and whitish cut surface (Fig 1d). On light microscopy, a circumscribed and
non-encapsulated spindle cell neoplasm was seen centred at the subserosa
and muscularis propria (Fig 2a). The spindle cells were arranged in vague
fascicles and possessed elongated nuclei with a small amount of
amphophilic cytoplasm set in a collagenous background. There was no
significant nuclear atypia and mitotic figures were present at up to 1 per
50 high-power field. Scattered linear blood vessels were noted among the
spindle cells. Ulceration with fibrinous exudation, granulation tissue
reaction, and mixed inflammatory cell infiltration were noted at the
serosal surface. On immunohistochemical staining, tumour cells exhibited a
beta-catenin nuclear translocation pattern and were weakly positive for
c-Kit (Fig 2b and 2c). They were negative for DOG-1, CD34
(GIST markers) [Fig 2d], MNF116 (cytokeratin marker), S100 (Schwann
cell marker), and actin and desmin (smooth muscle markers). The overlying
small intestine mucosa was unremarkable. The features were compatible with
a diagnosis of mesenteric fibromatosis (MF).
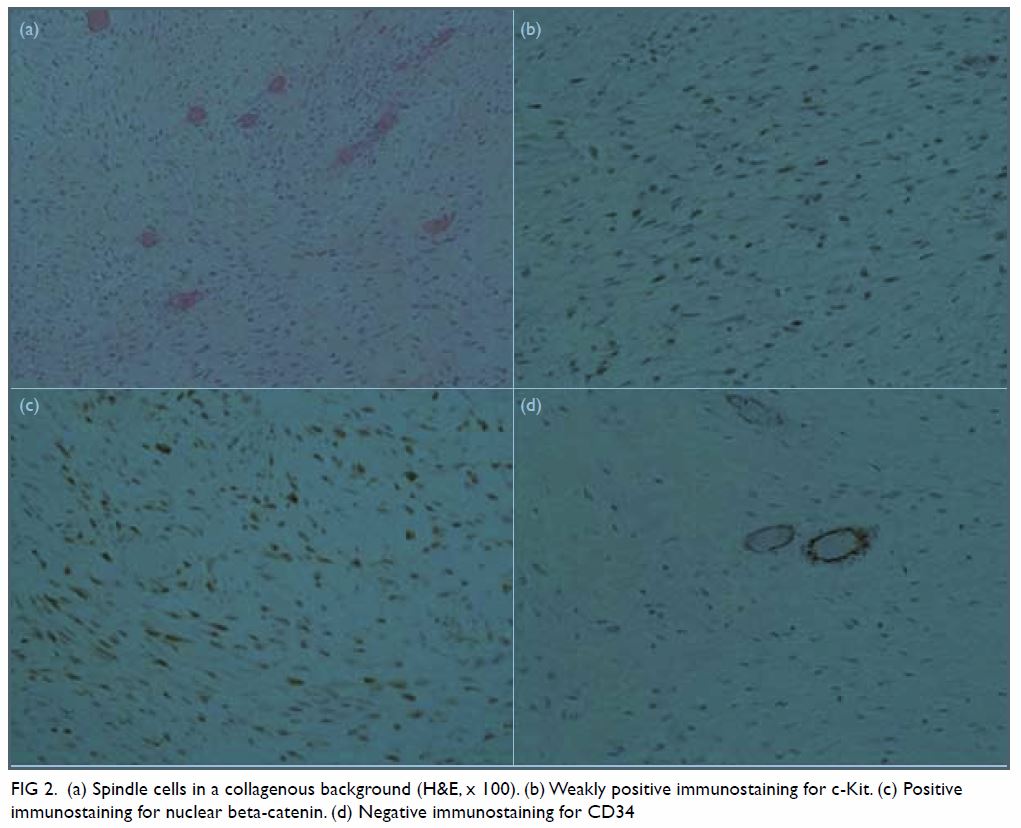
Figure 2. (a) Spindle cells in a collagenous background (H&E, x 100). (b) Weakly positive immunostaining for c-Kit. (c) Positive immunostaining for nuclear beta-catenin. (d) Negative immunostaining for CD34
The patient had an intra-abdominal collection
postoperatively that was successfully treated by ultrasound-guided
drainage and antibiotics. He was discharged 2 weeks later.
Discussion
Mesenteric fibromatosis is a rare sporadic
mesenchymal neoplasm of the small bowel mesentery that arises from
myofibroblasts. It is a histologically benign disease and lacks the
capacity to metastasise.1 2 3 Nonetheless,
MF is locally aggressive with a high recurrence rate after surgical
resection. Symptomatic MF mostly presents with abdominal pain or a
palpable mass on physical examination. Gastrointestinal perforation is a
rare manifestation. The first case of peritonitis secondary to MF reported
in the literature was by Gorlin and Chaudhry in 1960.4 The case presented here was initially misinterpreted as
a ruptured GIST. Although MF and GIST are completely different entities,
their clinical, radiological, and histological features frequently overlap
and may confuse clinicians.
Computed tomography is the mainstay of diagnosis
and typically demonstrates an infiltrative homogeneous soft tissue mass
that abuts or extends into the gastrointestinal wall.3 The case presented here demonstrated a mass that could
not be delineated from adjacent small bowel wall thus mimicking a
small-bowel GIST. To distinguish MF from GIST on CT, Zhu et al1 suggested a number of differentiating features in
favour of MF including extra-gastrointestinal location, ovoid or irregular
contour, homogeneous enhancement, absence of intralesional necrosis, lower
degree of enhancement and lesion-to-aorta CT attenuation ratio. Magnetic
resonance imaging of MF typically demonstrates low-signal intensity
relative to muscle on the T1-weighted image and variable signal intensity
on the T2-weighted image. On the contrary, GIST typically has high-signal
intensity on T2-weighted images.3
Gross pathological examination of MF usually shows
a well-circumscribed hard-to-firm mass with white glistening on the cut
section. Microscopically, MF has a number of characteristics similar to
GIST, with frequently overlapping immunophenotypes. Distinction of MF from
GIST is clinically important, as they are different entities with a
different clinical course, treatment options, and prognosis. On light
microscopy, MF samples typically demonstrate homogeneous spindle cells
without atypia, infrequent mitotic figures, and abundant collagen among
dilated vessels.2 3 In contrast, GIST samples demonstrate spindle cells
forming fascicles commonly with atypia and higher cellularity with
necrosis often present. Both MF and GIST may manifest overexpression of
c-Kit.2 3
Nonetheless, nuclear beta-catenin is expressed in MF but not in GIST, and
MF is negative for CD34.
Treatment of MF should be tailored to the
individual patient. Although watchful waiting may be offered for
asymptomatic MF, surgical resection is usually indicated in large
symptomatic cases of MF or in MF with complications.5 Such MF is known to be locally aggressive and tends to
recur when incompletely resected.2
3 5
The decision for radiotherapy or systemic treatment with chemotherapy or
hormonal therapy should be made after discussion with oncologists.
Recently the use of imatinib, a tyrosine kinase inhibitor, has shown
success in the treatment of locally advanced MF.5
Declaration
The authors have disclosed no conflicts of
interest.
References
1. Zhu H, Chen H, Zhang S, Peng W.
Intra-abdominal fibromatosis: Differentiation from gastrointestinal
stromal tumour based on biphasic contrast-enhanced CT findings. Clin
Radiol 2013;68:1133-9. Crossref
2. Rodriguez JA, Guarda LA, Rosai J.
Mesenteric fibromatosis with involvement of the gastrointestinal tract. A
GIST simulator: a study of 25 cases. Am J Clin Pathol 2004;121:93-8. Crossref
3. Wronski M, Ziarkiewicz-Wroblewska B,
Slodkowski M, Cebulski W, Gornicka B, Krasnodebski IW. Mesenteric
fibromatosis with intestinal involvement mimicking a gastrointestinal
stromal tumour. Radiol Oncol 2011;45:59-63. Crossref
4. Gorlin RJ, Chaudhry AP. Multiple
osteomatosis, fibromas, lipomas and fibrosarcomas of the skin and
mesentery, epidermoid inclusion cysts of the skin, leiomyomas and multiple
intestinal polyposis: a heritable disorder of connective tissue. N Engl J
Med 1960;263:1151-8. Crossref
5. Kasper B, Baumgarten C, Bonvalot S, et
al. Management of sporadic desmoid-type fibromatosis: a European consensus
approach based on patients’ and professionals’ expertise—a sarcoma
patients EuroNet and European Organisation for Research and Treatment of
Cancer/Soft Tissue and Bone Sarcoma Group initiative. Eur J Cancer
2015;51:127-36. Crossref

