Hong Kong Med J 2017 Jun;23(3):258–63 | Epub 3 Mar 2017
DOI: 10.12809/hkmj164852
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE
Factors that influence recurrent lumbar
disc herniation
Mesut E Yaman, MD1;
Atilla Kazancı, MD2;
Nur D Yaman, MD3;
Ferhat Baş4;
Gıyas Ayberk, MD2
1 Department of Neurosurgery, Memorial Ankara Hospital, Ankara, Turkey
2 Department of Neurosurgery, Ataturk Education and Research Hospital, Ankara, Turkey
3 Ankara University School of Medicine, Ankara, Turkey
4 Hacettepe University Graduate School of Health Sciences, Ankara, Turkey
An earlier version of this paper was presented orally at the 15th World
Congress of Neurosurgery held in Seoul, South Korea on 8-13 September 2013.
Corresponding author: Dr Mesut E Yaman (mesutemreyaman@hotmail.com)
Abstract
Introduction: The most common cause of poor
outcome following lumbar disc surgery is recurrent
herniation. Recurrence has been noted in 5% to 15% of
patients with surgically treated primary lumbar disc
herniation. There have been many studies designed
to determine the risk factors for recurrent lumbar
disc herniation. In this study, we retrospectively
analysed the influence of disc degeneration, endplate
changes, surgical technique, and patient’s clinical
characteristics on recurrent lumbar disc herniation.
Methods: Patients who underwent primary single-level
L4-L5 lumbar discectomy and who were reoperated
on for recurrent L4-L5 disc herniation were
retrospectively reviewed. All these operations were
performed between August 2004 and September
2009 at the Neurosurgery Department of Ataturk
Education and Research Hospital in Ankara, Turkey.
Results: During the study period, 126 patients were
reviewed, with 101 patients underwent primary single-level L4-L5 lumbar discectomy and 25 patients were
reoperated on for recurrent L4-L5 disc herniation.
Preoperative higher intervertebral disc height
(P<0.001) and higher body mass index (P=0.042)
might be risk factors for recurrence. Modic endplate
changes were statistically significantly greater in the
recurrent group than in the non-recurrent group
(P=0.032).
Conclusion: Our study suggests that patients
who had recurrent lumbar disc herniation had
preoperative higher disc height and higher body
mass index. Modic endplate changes had a higher
tendency for recurrence of lumbar disc herniation.
Well-planned and well-conducted large-scale
prospective cohort studies are needed to confirm
this and enable convenient treatment modalities to
prevent recurrent disc pathology.
New knowledge added by this study
- Preoperative higher disc height, higher body mass index, and greater Modic endplate changes are important factors in recurrent lumbar disc herniation.
- This study revealed that patients who had lumbar disc herniation with preoperative higher disc height and Modic changes have a higher tendency to recurrence of lumbar disc herniation.
- It is important to bear these factors in mind preoperatively and ensure discussion of expectations of surgery with the patient.
Introduction
Single-level lumbar discectomy is a very common
surgical procedure and has been proven to be
beneficial for patients with lumbar disc herniation
(LDH). Recurrent lumbar disc herniation (rLDH) is
defined as disc herniation at the same level, regardless
of ipsilateral or contralateral herniation, in a patient
who has experienced a pain-free interval of at least
6 months after surgery.1 2 The true incidence of same-level rLDH after lumbar discectomy is unclear.
The recurrence rate of LDH has been reported
to be 5% to 15%.1 2 3 4 5 There have been many studies
designed to determine the recurrence of LDH,
and various risk factors suggested including disc
degeneration, trauma, age, smoking, gender, and
obesity.1 3 6 Radiologically identifiable factors, such
as disc degeneration, disc height, and sagittal range
of motion have been shown to be related to spinal
instability and consequently to rLDH.7 8 9 In this
retrospective study, we analysed the influence of disc
degeneration, endplate changes, surgical technique,
and patient’s clinical characteristics on rLDH.
Methods
We examined factors that could influence the
recurrence of LDH, especially in those with
the highest recurrence rate, and to minimise
the biomechanical changes at every level. We
retrospectively reviewed the medical records of
patients with L4-L5 LDH who underwent lumbar
discectomy between August 2004 and September
2009 at the Neurosurgery Department of Ataturk
Education and Research Hospital in Ankara, Turkey.
This hospital is a tertiary referral hospital and a
centre for education and scientific research. This
study was approved by the Ethics Committee of
Ankara Ataturk Education and Research Hospital,
Turkey. The principles outlined in the Declaration of
Helsinki have also been followed.
Patients were excluded if they had any of
the following: prior lumbar surgery at another
institution, segmental instability, vertebral fractures
and spinal infections, other types of degenerative disc
disease, tumours, pregnancy, and age over 75 years.
Patients were included if they had radicular pain for
at least 3 months that was refractory to 6 weeks of
conservative treatment with or without neurological
deficit, numbness in the lumbar spine, buttock, and/or lower extremity, age between 21 and 75 years,
and magnetic resonance imaging (MRI) and/or
computed tomography demonstrating anatomical
unilateral LDH correlating with symptoms. In the
rLDH group, patients were additionally required to
have had a pain-free interval of at least 6 months
following the first surgery. We compared the
patients’ demographic and clinical characteristics
(age, sex, body mass index [BMI], diabetes mellitus,
smoking, herniation type), preoperative radiological
parameters (Pfirrmann disc degeneration grade,
Modic endplate changes, disc height), surgical
technique (microdiscectomy, open discectomy), and
duration of symptoms. All surgeries were performed
by the same group of surgeons via microdiscectomy
or open discectomy technique as previously reported
and standardised by Williams10 and Mixter.11 The type of herniation was classified as protrusion,
extrusion, or sequestration after retrospective review
of surgical records and MRI studies. The staff in the
radiological department were blinded to the outcome
of the study. Lumbar MRI and simple radiographic
examinations were performed in all patients before
surgery. Intervertebral disc height measurements
were calculated using the lateral radiographs. The
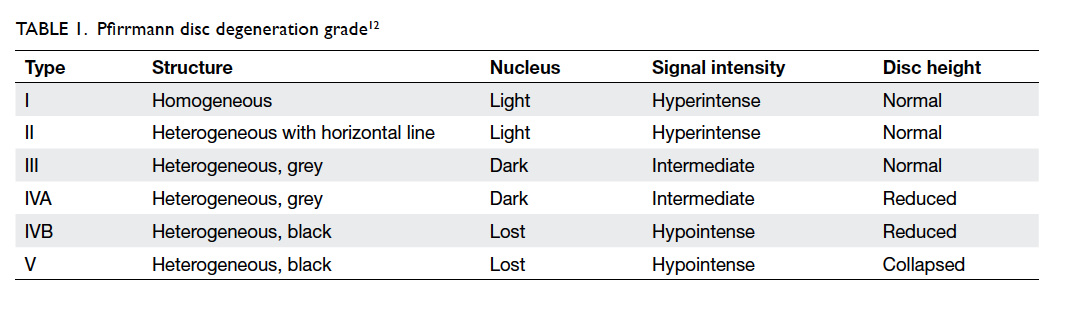
degree of disc degeneration was assessed on T2-weighted sagittal MRI sequences. Disc degeneration
was classified by our radiological department in
a retrospective and blinded manner according to
modified Pfirrmann criteria as shown in Table 1.12
Modic endplate changes were also classified with
the help of our radiological department on T1/T2-weighted sagittal MRI sequences, again blinded to
the outcome.13 14
Data analysis was performed using the
Statistical Package for the Social Sciences (Windows
version 11.5; SPSS Inc, Chicago [IL], United States). Test of
normality was applied to parametric data. Parametric
numerical data were compared with Student’s t test
and non-parametric data with Mann-Whitney U
test. Chi squared test was used with Fisher’s exact
test to compare categorical and nominal variables
as appropriate. Wilcoxon signed-rank test was used
to compare differences between paired data. To
identify the associations between recurrence and
diabetes mellitus and smoking, logistic regression
analysis was used. In detail, recurrence was included
in the regression model as a dependent variable;
smoking status and existence of diabetes mellitus
were included as covariants and the enter mode was
used. P value was used to determine whether the
differences were statistically significant. A P value of
<0.05 was considered statistically significant.
Results
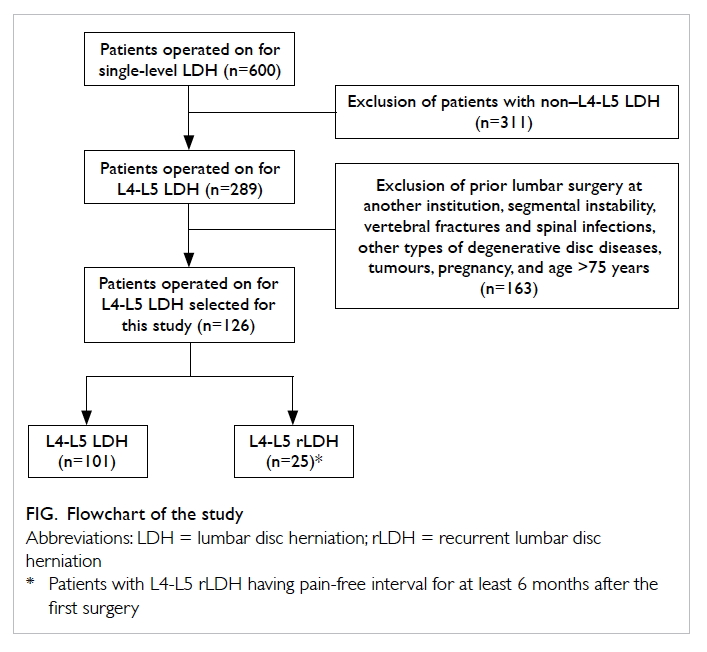
A retrospective analysis of 600 patients who
underwent surgery between August 2004 and
September 2009 for only a single-level LDH was
performed. The level of disc herniation was L1-L2 in
four (0.7%), L2-L3 in 17 (2.8%), L3-L4 in 39 (6.5%), L4-L5
in 289 (48.2%), and L5-S1 in 251 (41.8%) patients.
Of the 600 patients, 44 had rLDH; their respective
distributions of disc levels were 0, 1, 3, 25, and 15.
The total recurrence rate was 7.3%. Recurrence rate
for L4-L5 level was the highest at 8.6%. The mean
follow-up time of all patients was 323 days. The
mean symptom duration was 78 days for the non-recurrent
group and 77 days for the recurrent group.
Patients in the recurrent group were pain-free for at
least 6 months after the first operation with a median
of 240 days (range, 188-1260 days).
After applying the exclusion/inclusion
criteria, we retrospectively analysed 126 patients
who underwent primary single-level L4-L5 lumbar
discectomy and who were reoperated on for rLDH.
The patients were divided into recurrent (n=25) and
non-recurrent (n=101) group (Fig).
Univariate analysis for demographics, and
clinical and radiological characteristics of the
recurrent and non-recurrent groups is shown in
Table 2. There were no significant differences in the
age, sex, type of disc herniation, type of surgery, and
duration of symptoms between the two groups. Of
the patients, 13 (52.0%) in the recurrent group and
42 (41.6%) in the non-recurrent group were smokers.
In comparison with non-smokers, smokers had a
50% higher recurrence rate (odds ratio [OR]=1.52;
95% confidence interval [CI], 0.63-3.66). Five (20.0%)
patients in the recurrent group and 10 (9.9%) in the
non-recurrent group had diabetes mellitus. Patients
with diabetes mellitus had twice the recurrence
rate of those without (OR=2.27; 95% CI, 0.70-7.38).
Preoperative mean intervertebral disc heights
were significantly different between the recurrent
(19.1 mm) and non-recurrent (15.0 mm) groups
(P<0.001). A higher preoperative intervertebral disc
space might be a risk factor for recurrence. A higher
BMI was a statistically significant factor in the
recurrent group (P=0.042). Modic endplate changes
were statistically higher in the recurrent group than
in the non-recurrent group (P=0.032). In the non-recurrent
group, 13 (12.9%) patients showed grade II, 51 (50.5%) showed
grade III, 24 (23.8%) showed grade IVA, and 13
(12.9%) showed grade IVB Pfirrmann disc degeneration. Although Pfirrmann
disc degeneration was not statistically significant between the two groups (P=0.079), it might still be a
moderate marker for a potential risk of recurrence.
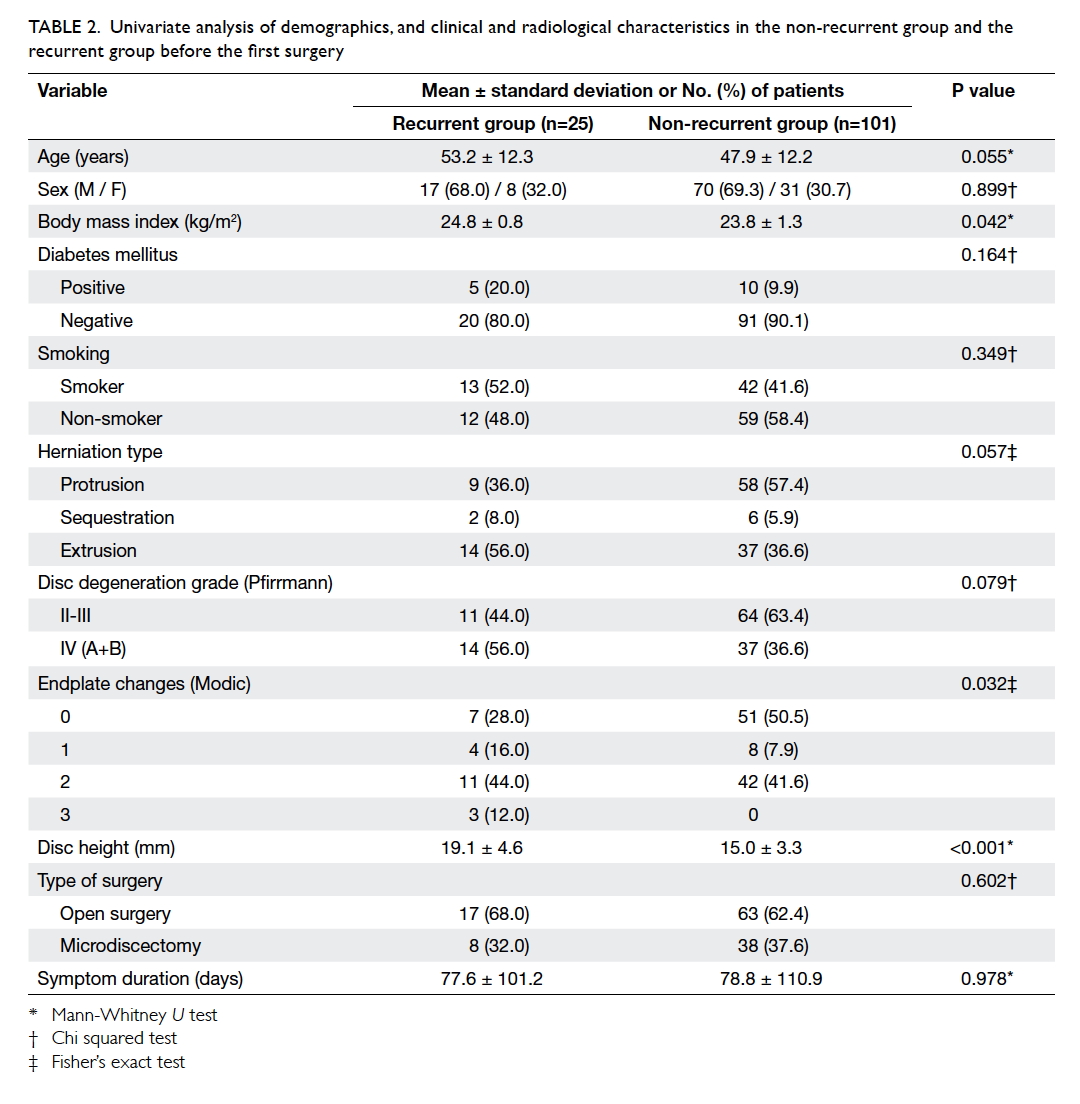
Table 2. Univariate analysis of demographics, and clinical and radiological characteristics in the non-recurrent group and the recurrent group before the first surgery
The comparative analysis of preoperative
clinical and radiological characteristics of the
recurrent group is shown in Table 3. Before the first
surgery, one (4%) patient showed grade II, 10 (40%) showed grade III, eight (32%)
showed grade IVA, and six (24%) showed grade IVB
Pfirrmann disc degeneration. In one patient, grade
II Pfirrmann degeneration progressed to IVA before
the second surgery. Six of 10 patients with grade
III changed to IVB, three changed to IVA, and one
remained unchanged with a Pfirrmann degeneration
grade III after recurrence.
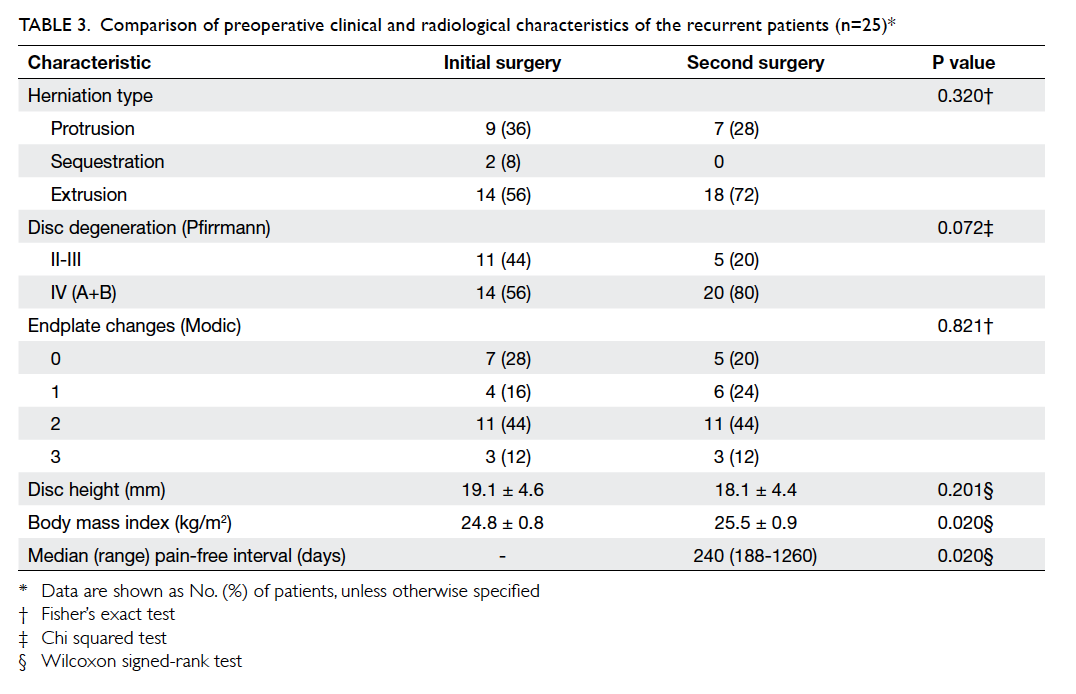
Table 3. Comparison of preoperative clinical and radiological characteristics of the recurrent patients (n=25)
These results led us to consider the relationship
between grade of degenerated disc and herniation
type. Herniation type was compared with Pfirrmann
disc degeneration degree and Modic endplate
changes. Patients with extrusion-sequestration
herniation had a statistically significant higher
Pfirrmann disc degeneration in contrast to patients
with protrusions (P=0.016). Nonetheless, there
was no correlation between Modic changes and
herniation type (P=0.279).
Discussion
Degenerative disc disease remains a poorly
understood phenomenon because of the lack of
precise definitions for healthy and degenerated discs.
Decreased nutrition is the final common pathway
for degenerative disc disease and the status of the
endplate plays a crucial role in controlling the extent
of diffusion and is the only source of nutrition.15
A recurrence rate of 5% to 15% for LDH has been reported.1 2 3 4 5 Differentiation of recurrent disc herniation from scar formation
will allow for improved treatment choices and
selection of patients who may benefit from a second
surgery. Gadolinium-enhanced MRI is thought
to be the best modality to differentiate between
these two diagnoses. There is much debate about
the risk factors for rLDH and it is very difficult to
define them because many clinical and complicated
biomechanical parameters are involved.
In this study, we analysed the influence of disc
degeneration, endplate changes, surgical technique,
and patient’s clinical characteristics (age, gender,
BMI, symptom duration, herniation type, smoking
status, and diabetes). Kim et al6 reported old age,
high BMI, protrusion type of disc herniation,
and positive Modic changes as risk factors after
percutaneous endoscopic discectomy. Swartz and
Trost,2 however, found that age, gender, smoking
status, level of herniation, and duration of symptoms
were not associated with rLDH. We showed that
disc height, BMI, and Modic endplate changes were
significantly correlated with a higher incidence of
rLDH. Although diabetes and smoking were not
statistically significant in our study, patients with
diabetes had twice the recurrence rate of those
without. Furthermore, patients who were a smoker
had a 50% higher recurrence rate in contrast to non-smokers.
The exact mechanism by which smoking
contributes to disc degeneration is incompletely
understood, but may be related to disc annulus
nutrition and oxygenation, as well as increases in
intradiscal pressure due to excessive coughing.
Vascular insufficiency as a result of atheromas should
also be considered.16 17 18 19 20 Analogous with our results, these presumptions may account for smoking as
a cause of rLDH. In contrast with these findings, however, some studies found no relationship between
smoking and rLDH.21 22 23
Clinical studies of disc height and recurrence
have shown that degenerative segments with
preserved disc height have a latent instability
compared with segments with collapsed discs.8
Other studies have shown that the restabilisation
stage begins when disc height is reduced by 50%.7
Similar to these studies, our study showed that
preoperative higher intervertebral disc space
measurements were significantly more important in
recurrence (P<0.001).
Pfirrmann disc degeneration grade was not
statistically significant in the recurrent group in
contrast to non-recurrent group (P=0.079), but
patients with extrusion and sequestration had
a statistically significant higher Pfirrmann disc
degeneration than patients with protrusions
(P=0.016). These findings provide evidence that
the healing processes that occur in the outer
lamellas after annular injury may not be sufficient
for effective reconstitution of the external
annulus in degenerated discs.24 25 Increases in disc degeneration cause larger volumes of herniation
type. Studies of Modic endplate changes after
lumbar discectomy have shown incremental changes
in disc degeneration grade.18 26 It is accepted that
Modic type 1 changes are dynamically unstable and
inflammatory lesions, whereas type 2 lesions are
much more stable and unchangeable.26 Therefore,
posterior lumbar interbody fusion combined with
pedicle screw fixation is suggested for degenerative
lumbar disc disease with Modic changes.27 Another
study suggested treatment of Modic type 1 and 2
lesions with degenerative disc disease with posterior
dynamic stabilisation.28 Our study showed that
Modic changes were statistically higher in the
recurrent group than the non-recurrent group
(P=0.032). These findings suggest that patients
with LDH and higher preoperative disc heights and
Modic changes have a higher risk and tendency to
recurrence of LDH. Although our study does not
include different modalities to include lumbar disc
diseases with Modic changes, the results might
suggest a supplemental approach such as posterior
stabilisation and fusion, or newly proposed treatment
options with dynamic posterior stabilisation.
This study has several limitations. It would have
a greater impact if we had included a larger subgroup
population, especially for rLDH. To investigate factors
that influence recurrence of L4-L5 disc herniation,
however, several clinical and radiological parameters
such as canal diameter, facet angle, annular defect
size, location of the herniation type etc would need
to be considered. The aim of this study was to focus
on the effect of disc height, endplate changes, and
disc degeneration in rLDH at L4-L5 level. As only
univariate analyses were performed, we have no
adjustment for potential confounding, hence the
independent effects of the risk factors could not
be documented. A prospective study would obtain
more precise results, especially due to standardised
sampling and classification of data.
Conclusion
This study suggests that patients who had LDH with
higher preoperative disc height, higher BMI, and
Modic endplate changes have a higher tendency for
rLDH. Well-planned and well-conducted large-scale
prospective cohort studies are essential to firmly
evaluate and determine factors involved in rLDH.
Acknowledgement
We thank Ms Fatma Kubra Erbay from Department of Micro and Nanotechnology, TOBB
University of Economics and Technology, Ankara,
Turkey for her great effort in revising the
statistical results of this study.
Declaration
All authors have disclosed no conflicts of interest.
References
1. Suk KS, Lee HM, Moon SH, Kimm NH. Recurrent lumbar
disc herniation: results of operative management. Spine
(Phila Pa 1976) 2001;26:672-6. Crossref
2. Swartz KR, Trost GR. Recurrent lumbar disc herniation.
Neurosurg Focus 2003;15:E10. Crossref
3. Connolly ES. Surgery for recurrent lumbar disc herniation.
Clin Neurosurg 1992;39:211-6.
4. Fandiño J, Botana C, Viladrich A, Gomez-Bueno J.
Reoperation after lumbar disc surgery: results in 130 cases.
Acta Neurochir (Wien) 1993;122:102-4. Crossref
5. Mobbs RJ, Newcombe RL, Chandran KN. Lumbar
discectomy and the diabetic patient: incidence and
outcome. J Clin Neurosci 2001;8:10-3. Crossref
6. Kim JM, Lee SH, Ahn Y, Yoon DH, Lee CD, Lim ST.
Recurrence after successful percutaneous endoscopic
lumbar discectomy. Minim Invasive Neurosurg 2007;50:82-5. Crossref
7. Axelsson P, Karlsson BS. Intervertebral mobility in the
progressive degenerative process. A radiostereometric
analysis. Eur Spine J 2004;13:567-72. Crossref
8. Hasegawa K, Kitahara K, Hara T, Takano K, Shimoda H,
Homma T. Evaluation of lumbar segmental instability
in degenerative diseases by using a new intraoperative
measurement system. J Neurosurg Spine 2008;8:255-62. Crossref
9. Zhao F, Pollintine P, Hole BD, Dolan P, Adams MA.
Discogenic origins of spinal instability. Spine (Phila Pa
1976) 2005;30:2621-30. Crossref
10. Williams RW. Microlumbar discectomy: a conservative
surgical approach to the virgin herniated lumbar disc.
Spine (Phila Pa 1976) 1978;3:175-82. Crossref
11. Mixter WJ. Pitfalls in the surgery of the ruptured
intervertebral disk. J Fla Med Assoc 1952;39:159-67.
12. Pfirrmann CW, Metzdorf A, Zanetti M, Hodler J, Boos N.
Magnetic resonance classification of lumbar intervertebral
disc degeneration. Spine (Phila Pa 1976) 2001;26:1873-8. Crossref
13. Modic MT, Masaryk TJ, Ross JS, Carter JR. Imaging of
degenerative disk disease. Radiology 1998;168:177-86. Crossref
14. Modic MT, Steinberg PM, Ross JS, Masaryk TJ, Carter
JR. Degenerative disk disease: assessment of changes
in vertebral body marrow with MR imaging. Radiology
1988;166(1 Pt 1):193-9. Crossref
15. Rajasekaran S, Venkatadass K, Naresh Babu J, Ganesh K,
Shetty AP. Pharmacological enhancement of disc diffusion
and differentiation of healthy, ageing and degenerated
discs: results from in-vivo serial post-contrast MRI studies
in 365 human lumbar discs. Eur Spine J 2008;17:626-43. Crossref
16. Akmal M, Kesani A, Anand B, Singh A, Wiseman M,
Goodship A. Effect of nicotine on spinal disc cells: a
cellular mechanism for disc degeneration. Spine (Phila Pa
1976) 2004;29:568-75. Crossref
17. Frymoyer JW, Pope MH, Costanza MC, Rosen JC, Goggin
JE, Wilder DG. Epidemiologic studies of low-back pain.
Spine (Phila Pa 1976) 1980;5:419-23. Crossref
18. Iwahashi M, Matsuzaki H, Tokuhashi Y, Wakabayashi K,
Uematsu Y. Mechanism of intervertebral disc degeneration
caused by nicotine in rabbits to explicate intervertebral
disc disorders caused by smoking. Spine (Phila Pa 1976)
2002;27:1396-401. Crossref
19. Nemoto Y, Matsuzaki H, Tokuhasi Y, et al. Histological
changes in intervertebral discs after smoking cessation:
experimental study using a rat passive smoking model. J
Orthop Sci 2006;11:191-7. Crossref
20. Stairmand JW, Holm S, Urban JP. Factors influencing
oxygen concentration gradients in the intervertebral disc.
A theoretical analysis. Spine (Phila Pa 1976) 1991;16:444-9. Crossref
21. Kara B, Tulum Z, Acar U. Functional results and the risk
factors of reoperations after lumbar disc surgery. Eur Spine
J 2005;14:43-8. Crossref
22. Meredith DS, Huang RC, Nguyen J, Lyman S. Obesity
increases the risk of recurrent herniated nucleus pulposus
after lumbar microdiscectomy. Spine J 2010;10:575-80. Crossref
23. Palma L, Carangelo B, Muzii VF, Mariottini A, Zalaffi
A, Capitani S. Microsurgery for recurrent lumbar disk
herniation at the same level and side: do patients fare
worse? Experience with 95 consecutive cases. Surg Neurol
2008;70:619-21. Crossref
24. Hampton D, Laros G, McCarron R, Franks D. Healing
potential of the anulus fibrosus. Spine (Phila Pa 1976)
1989;14:398-401. Crossref
25. Osti OL, Vernon-Roberts B, Fraser RD. 1990 Volvo Award
in experimental studies. Anulus tears and intervertebral
disc degeneration. An experimental study using an animal
model. Spine (Phila Pa 1976) 1990;15:762-7. Crossref
26. Rahme R, Moussa R, Bou-Nassif R, et al. What happens to
Modic changes following lumbar discectomy? Analysis of a
cohort of 41 patients with a 3- to 5-year follow-up period. J
Neurosurg Spine 2010;13:562-7. Crossref
27. Kwon YM, Chin DK, Jin BH, Kim KS, Cho YE, Kuh
SU. Long term efficacy of posterior lumbar interbody
fusion with standard cages alone in lumbar disc diseases
combined with modic changes. J Korean Neurosurg Soc
2009;46:322-7. Crossref
28. Öktenoglu T, Ozer AF, Sasani M, et al. Posterior dynamic
stabilization in the treatment of lumbar degenerative disc
disease: 2-year follow-up. Minim Invasive Neurosurg
2010;53:112-6. Crossref