DOI: 10.12809/hkmj154616
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
CASE REPORT
Liver transplantation: a life-saving procedure
following amatoxin mushroom poisoning
KW Ma, MB, BS, FHKAM (Surgery)1; Kenneth SH Chok, MS, FHKAM (Surgery)1,2; CK Chan, MB, BS, FHKAM (Emergency Medicine)3; WC Dai, MB, BS, FHKAM (Surgery)1,2; SL Sin, MB, ChB, FHKAM (Surgery)1; FL Lau, MB, BS, FHKAM (Emergency Medicine)3; SC Chan, MD, FHKAM (Surgery)2; CM Lo, MS, FHKAM (Surgery)1,2
1 Department of Surgery, Queen Mary Hospital, Pokfulam, Hong Kong
2 Department of Surgery, The University of Hong Kong, Pokfulam, Hong Kong
3 Hong Kong Poison Information Centre, United Christian Hospital, Kwun Tong, Hong Kong
Corresponding author: Dr Kenneth SH Chok (kennethchok@gmail.com)
Case reports
Case 1
In April 2013, a 48-year-old man and his wife picked
wild mushrooms near Shing Mun Reservoir. After
eating the cooked mushrooms, they developed
symptoms resembling gastroenteritis and attended
accident and emergency department (A&E) around
12 hours later. The husband was alert with normal
blood test results at 18 hours following ingestion.
Thirty hours later, his total bilirubin increased to
54 µmol/L (reference range, 4-23 µmol/L), serum
alanine transaminase (ALT) to 2928 IU/L (reference
range, 8-58 IU/L), serum creatinine to 229 µmol/L
(reference range, 67-109 µmol/L), and international
normalised ratio (INR) to 1.56 (reference level, <1.1).
Mushroom poisoning was suspected and the Hong
Kong Poison Information Centre was contacted. He
was given N-acetylcysteine (NAC), silibinin, and
penicillin G in the intensive care unit. Subsequent
blood tests showed no improvement and around 48
hours after ingestion, his serum ALT climbed to 4856 IU/L
and INR to 2.25. He was transferred to the intensive
care unit of Queen Mary Hospital (QMH) for further
care.
At QMH, computed tomography of the
abdomen revealed hypo-enhancement of the liver
parenchyma. Liver transplant workup was initiated
in view of impending liver failure. Fortunately
his liver function started to stabilise 8 hours after
admission to QMH, with a serum ALT peak at 3856 IU/L
and INR at 3.5. He then made progressive recovery
and was discharged 10 days after admission.
Case 2
The 47-year-old wife of the patient in case 1 had a
high fever of 38.8°C upon admission. Blood tests
taken around 12 hours after ingestion showed
normal results. Twenty-four hours later, her serum
ALT rose to 751 IU/L. Thirty-six hours later, it rose
further to 2654 IU/L with an INR of 2.59. A clinical
toxicologist was consulted and amatoxin poisoning
was diagnosed; NAC, penicillin G, vitamin K,
and silibinin were commenced. At 72 hours after
ingestion, her serum ALT surged to 5132 IU/L, INR 5.28,
total bilirubin 42 µmol/L, and ammonia 35 µmol/L.
She was transferred to QMH.
Upon arrival, computed tomographic features
were similar to those of her husband, with liver
necrosis suggested. Her INR surged further to 7.2.
According to the King’s College Criteria for acute
liver failure, liver transplantation was indicated
and transplant workup started. Fortunately, an
ABO-compatible deceased donor liver graft was
available. Liver transplantation was performed 36
hours after admission (about 5 days after ingestion).
The operation took 7 hours, and the patient had
3 L of blood loss. Pathological examination
of the explant showed massive necrosis. She was
discharged on postoperative day 30, requiring life-long
immunosuppression.
Case 3
A 29-year-old man ate raw, whitish yellow
mushrooms while hiking at Ma On Shan in March
2015. Twelve hours later he developed vomiting and
diarrhoea. His symptoms improved afterwards. On
day 4 after ingestion, he was found to have jaundice
and confusion and was brought to A&E. Upon
arrival, his Glasgow Coma Scale score was 14/15.
The first blood tests showed grossly deranged results:
serum creatinine 241 µmol/L, sodium 117 mmol/L,
potassium 6.1 mmol/L, total bilirubin 246 µmol/L,
serum ALT 9390 IU/L, and INR >8. Before he was
transferred to QMH, NAC, penicillin G, vitamin K1,
and fresh frozen plasma were given.
At QMH, liver transplant workup was
started, but his elder brother was not accepted
for liver donation as he was shown to have severe
fatty liver on computed tomography. The patient’s
condition deteriorated. His Glasgow Coma Scale
score dropped to 4/15, and oxygen desaturation
and seizure developed. With the presence of severe
hepatic encephalopathy, any delay in rescue would
increase the chance of irreversible brain insult due
to cerebral oedema. Coincidentally, a liver from a
60-year-old brain-dead woman whose blood group
was identical to the patient’s was available.
A multidisciplinary clinical team involving
cardiac and respiratory physicians, radiologists,
anaesthesiologists, intensivists, cardiothoracic
surgeons, and liver transplant surgeons coordinated
to expedite the operation. Liver procurement and
implantation were started within a few hours, with
two teams of liver transplant surgeons working
in parallel. The recipient operation took 6 hours.
Pathological examination of the explant showed
confluent necrosis. The patient was discharged on
day 20.
Discussion
According to the Hong Kong Poison Information
Centre database, there have been seven documented
cases of amatoxin mushroom poisoning since
July 2005, resulting in one death and two liver
transplantations (Table). Amatoxin poisoning leads to the most serious consequences and accounts for
more than 90% of mushroom-related mortalities.1
Amatoxins, phallotoxins, and other toxic
cyclopeptides are produced by certain mushroom
species of three genera, namely the Amanita,
Galerina, and Lepiota, while Amanita phalloides is
the most infamous type, also known as the “death
cap”.2 Amatoxins are highly toxic and cannot be
destroyed by any means of food processing.3 The
liver is the most affected organ, as amatoxins are
absorbed preferentially by hepatocytes and go
through the enterohepatic circulation. Other organs
can also be intoxicated. If the kidneys are involved,
acute renal failure secondary to acute tubular
necrosis may result.2
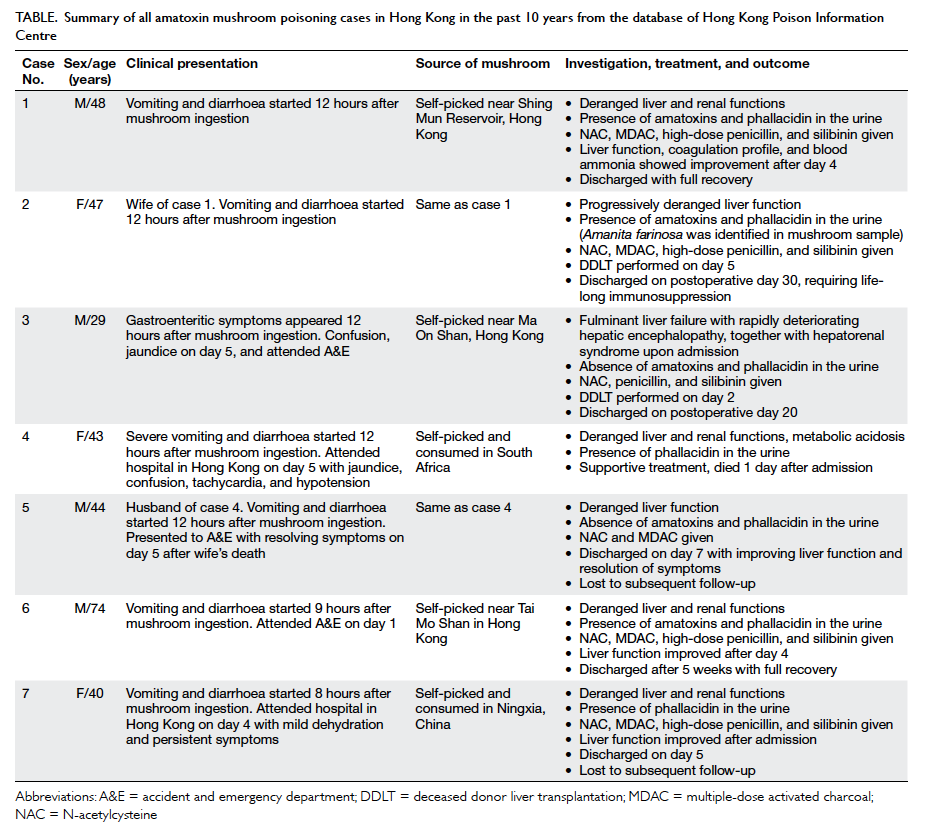
Table. Summary of all amatoxin mushroom poisoning cases in Hong Kong in the past 10 years from the database of Hong Kong Poison Information Centre
The clinical manifestation of amatoxin
poisoning typically consists of four sequential
phases. In the first phase, the ‘lag phase’, the patient
remains asymptomatic for at least 6 hours after
ingestion.4 This is one of the distinguishing features
of amatoxin poisoning, as most benign mushroom
poisonings cause gastrointestinal symptoms within 4
hours of ingestion. The ‘gastrointestinal phase’ comes
next, starting at 6 to 24 hours after ingestion, with
symptoms resembling severe gastroenteritis. Blood
tests in this phase usually show normal results unless
there is significant fluid loss via the gastrointestinal
tract.5 6 7 8 9 The ‘apparent convalescence phase’ follows at 36 to 48 hours after ingestion. In this period,
the patient has some relief from gastrointestinal
symptoms, but at the same time amatoxins start
to cause discernible hepatic injury presenting as
jaundice and a rise in serum aminotransferase.
Finally, the ‘acute liver failure phase’ sets in, with
drastic surges in liver enzymes, renal failure,
encephalopathy, hepatorenal syndrome,10 and multi-organ
failure. Without liver transplantation, severe
cases end in mortality 1 to 2 weeks after ingestion.11
Recovery with supportive treatment is possible in
cases of mild intoxication.
Tests including radioimmunoassay, enzyme-linked
immunosorbent assay, and high-performance
liquid chromatography are used to detect amatoxins
in body fluids or liver explants or as part of an
autopsy for confirmation. The sensitivity of these
tests depends on the time of sample collection.
The detection window of amatoxins is up to 5
days after ingestion in urine and up to 22 days in
tissue.12 Residual mushroom sample can be used
for mycological assessment. Urine amatoxin testing
was performed in the three cases reported above.
Cases 1 and 2 had positive results, whereas the
result in case 3 was negative, apparently because
the patient was brought to clinical attention several
days after ingestion; the negative result did not
exclude amatoxin poisoning. Diagnosis of amatoxin
poisoning requires a high index of suspicion and
detailed history taking, with particular attention to
the sequencing of events.
Management of amatoxin poisoning can be
classified as supportive with specific treatments. The
survival chance is 70% to 100% with early diagnosis
and intensive care.4 Patients who suffer from severe
gastrointestinal symptoms or organ failure require
intensive care aiming at an hourly urine output of
100 to 200 mL.4 Significant coagulopathy must be
corrected. Specific treatment can be subclassified
into medical and surgical one. N-acetylcysteine,
silibinin, penicillin G, multiple-dose activated
charcoal, and enhanced elimination methods
constitute the mainstay of medical treatment.4 5 6 7 9
N-acetylcysteine protects the liver by being an
oxygen free radical scavenger, while silibinin works
by inhibiting the organic anion transmembrane
transporter responsible for the uptake of amatoxins by
hepatocytes and the enterohepatic recycling of these
toxins.4 The role of penicillin G in treating amatoxin
poisoning is controversial. Penicillin G blocks uptake
of amatoxins by hepatocytes and binds to circulating
amatoxins. Oral multiple-dose activated charcoal
can be administered within 3 days of ingestion. It
works by inhibiting amatoxin absorption through
the intestinal mucosa and reabsorption via the
enterohepatic circulation. Enhanced elimination
methods including extracorporeal albumin dialysis,
the molecular adsorbent recirculating system, and
the fractionated plasma separation and adsorption
system (the Prometheus System) are investigational
therapies for amatoxin poisoning.
Conventional therapies fail in 10% to 20%
of cases.6 Death resulting from fulminant liver
failure is inevitable if timely liver transplantation
is not performed. As to when liver transplantation
is needed, there are different sets of parameters in
use, but none has gained universal acceptance in the
context of amatoxin-related liver failure. At QMH,
the King’s College Criteria are adopted. Pathological
examination suggested irreversible liver damage
in the explants in cases 2 and 3, and justified our
decision regarding transplantation.
Amatoxin poisoning is lethal. Clinicians should
be aware of its natural history and start treatment
early. Transferal, if needed, has to be timely. Public
education about the dangers of wild mushroom
consumption is vital.
Acknowledgements
We would like to thank Dr James YY Fung, Consultant
Hepatologist at Queen Mary Hospital, for his expert
advice on managing the above patients. We also
thank Dr SH Tsui for providing patient data for this
case report.
References
1. Bryngil J. Amanita phalloides. Clin Toxicol Rev
1999;21:191-8.
2. Himmelmann A, Mang G, Schnorf-Huber S. Lethal
ingestion of stored Amanita phalloides mushrooms. Swiss
Med Wkly 2001;131:616-7.
3. Gibbons RB. Mushroom poisoning. Compr Ther 1982;8:33-9.
4. Goldfrank LR. Mushrooms. In: Hoffman RS, Howland
MA, Lewin NA, Nelson LS, Goldfrank LR, editors.
Goldfrank’s toxicologic emergencies. 10th ed. New
York: McGraw-Hill; 2015: 1500-14.
5. Enjalbert F, Rapior S, Nouguier-Soulé J, Guillon S,
Amouroux N, Cabot C. Treatment of amatoxin poisoning:
20-year retrospective analysis. J Toxicol Clin Toxicol
2002;40:715-57. Crossref
6. Broussard CN, Aggarwal A, Lacey SR, et al. Mushroom
poisoning—from diarrhea to liver transplantation. Am J
Gastroenterol 2001;96:3195-8. Crossref
7. Berger KL, Guss DA. Mycotoxins revisited: part I. J Emerg
Med 2005;28:53-62. Crossref
8. Leist M, Gantner F, Naumann H, et al. Tumor necrosis
factor–induced apoptosis during the poisoning of mice
with hepatotoxins. Gastroenterology 1997;112:923-34. Crossref
9. Paaso B, Harrison DC. A new look at an old problem:
mushroom poisoning. Clinical presentations and
new therapeutic approaches. Am J Med 1975;58:505-9. Crossref
10. Sanz P, Reig R, Borrás L, Martínez J, Máñez R, Corbella J. Disseminated intravascular coagulation and mesenteric
venous thrombosis in fatal amanita poisoning. Hum
Toxicol 1988;7:199-201. Crossref
11. Butera R, Locatelli C, Coccini T, Manzo L. Diagnostic
accuracy of urinary amanitin in suspected mushroom
poisoning: a pilot study. J Toxicol Clin Toxicol 2004;42:901-12. Crossref
12. Jaeger A, Jehl F, Flesch F, Sauder P, Kopferschmitt J.
Kinetics of amatoxins in human poisoning: therapeutic
implications. J Toxicol Clin Toxicol 1993;31:63-80. Crossref

