Hong Kong Med J 2017 Feb;23(1):35–40 | Epub 2 Dec 2016
DOI: 10.12809/hkmj164899
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE
Chaperones and intimate physical examinations:
what do male and female patients want?
VC Fan, BSc1;
HT Choy, BSc1;
George YJ Kwok1;
HG Lam1;
QY Lim1;
YY Man1;
CK Tang1;
CC Wong1;
YF Yu1;
Gilberto KK Leung, MB, BS, PhD2
1 Department of Community Medicine, Li Ka Shing Faculty of Medicine, The University of Hong Kong, Pokfulam, Hong Kong
2 Department of Surgery, Li Ka Shing Faculty of Medicine, The University of Hong Kong, Pokfulam, Hong Kong
Corresponding author: Dr Gilberto KK Leung (gilberto@hku.hk)
Abstract
Introduction: Many studies of patients’ perception
of a medical chaperone have focused on female
patients; that of male patients are less well studied.
Moreover, previous studies were largely based on
patient populations in English-speaking countries.
Therefore, this study was conducted to investigate
the perception and attitude of male and female
Chinese patients to the presence of a chaperone
during an intimate physical examination.
Methods: A cross-sectional guided questionnaire
survey was conducted on a convenient sample of 150
patients at a public teaching hospital in Hong Kong.
Results: Over 90% of the participants considered
the presence of a chaperone appropriate during
intimate physical examination, and 84% felt that
doctors, irrespective of gender, should always
request the presence of a chaperone. The most
commonly cited reasons included the availability
of an objective account should any legal issue arise,
protection against sexual harassment, and to provide
psychological support. This contrasted with the
experience of those who had previously undergone
an intimate physical examination of whom only
72.6% of women and 35.7% of men had reportedly
been chaperoned. Among female participants,
75.0% preferred to be chaperoned during an
intimate physical examination by a male doctor,
and 28.6% would still prefer to be chaperoned
when being examined by a female doctor. Among
male participants, over 50% indicated no specific
preference but a substantial minority reported a
preference for chaperoned examination (21.2% for
male doctor and 25.8% for female doctor).
Conclusions: Patients in Hong Kong have a high
degree of acceptance and expectations about the
role of a medical chaperone. Both female and male
patients prefer such practice regardless of physician
gender. Doctors are strongly encouraged to discuss
the issue openly with their patients before they
conduct any intimate physical examination.
New knowledge added by this study
- Hong Kong patients have a high degree of acceptance and expectations about the presence of a medical chaperone during an intimate physical examination (IPE), but in actual practice, females and especially male patients are chaperoned less often than they would have preferred.
- A substantial minority (21%-29%) of Hong Kong patients of both genders preferred to be chaperoned for an IPE even when examined by a doctor of the same gender.
- More than a quarter (26%) of male patients preferred to be chaperoned for an IPE when examined by a female doctor.
- Before any IPE, regardless of doctor or patient gender, it is advisable for doctors to ask their patients if they would like to be chaperoned in order to respect for patient preferences.
Introduction
In this current era when personal privacy is highly
regarded, it may seem counterintuitive for patients
to prefer the presence of a third party during an
intimate physical examination (IPE). The presence
of a medical chaperone, however, may offer
comfort and psychological support for patients in
protecting them against indecent behaviour, and is
now an established good practice.1 Conversely, in
an increasingly litigious society, a chaperone may
serve as a witness to protect doctors against false
allegations.2 Usually IPEs involve per-rectal, genital,
or breast examinations, but may also include physical
contact with any other part of the patient’s body.
The majority of reports about patients’
perceptions of a medical chaperone have focused
on female patients3 4 5 6 7; those of male patients are less well studied.8 9 10 A potential discrepancy may exist
between the two groups. Santen et al10 reported
that in the US, a great majority of male
patients (88%) did not care about the presence of a
chaperone, while half of the female patients would
prefer to be chaperoned when examined by a male
physician, and a quarter when examined by a female
doctor. Moreover, previous studies have been largely
based on patient populations in English-speaking
countries. It has been suggested that the presence of
a chaperone is a ‘western concept’ that may receive a
different degree of emphasis or acceptance in other
parts of the world.11 To the best of our knowledge,
there has been no related report on patients in
Hong Kong. In this study, we investigated patients’
attitudes towards and experiences with the presence
of a medical chaperone, and in particular, the
relevant impact of patient and physician gender.
Methods
Study design
We conducted a cross-sectional questionnaire
survey of patients waiting for their consultations
at the Accident and Emergency Department and
the surgical out-patient clinic of a public teaching
hospital over a period of 2 weeks from late February to early March 2015. Participants were recruited irrespective of
age, gender or ethnicity, but were excluded if they
were under 18 years of age, or did not understand
English, Cantonese, or Mandarin. Participants from
the surgical out-patient clinic included both new
and follow-up patients from various subspecialties.
Informed patient consent and approval from the
Institutional Review Board of our institution were
obtained.
Survey instrument
The questionnaire, written in both English
and Chinese, comprised eight questions on
demographics, and 19 questions on previous
experiences with IPE, preferences for the presence
of a chaperone, influence of gender of the examining
physician, and the underlying reasons for their
preferences. Participants selected their answers
from predetermined options. In this study, IPE was
defined as breast, pelvic, genital, and/or per-rectal
examination. This was explained to the participants
at the beginning of the survey. Guidance on the
survey was provided by an investigator if requested
by the participant.
Statistical analyses
Data were analysed using the Statistical Package for
the Social Sciences (Windows version 22.0; SPSS
Inc, Chicago [IL], US). Descriptive analyses were
performed on demographic data and participant
responses. Patient ages were grouped into age ranges
(<40, 40-59, and ≥60) for analysis. The independent
variables were patient gender and other demographic
variables (eg age, education level). The dependent
variables were preference for the examining doctor’s
gender, presence of a chaperone with a male
examining doctor, gender of chaperone with a male
examining doctor, presence of chaperone with a
female examining doctor, and gender of chaperone
with a female examining doctor. Bivariate analyses
using the Chi squared test were performed to
compare the various independent variables against
the dependent variables. Other variables based
on participant responses—such as reasons behind
chaperone preferences, previous experience of IPE,
and tendency for litigation if felt harassed—were
analysed against other variables as appropriate.
Statistical significance was set at a probability level
of 0.05.
Results
Participant profile and demographics
Of a convenience sample of 183 patients, 33 declined
to participate and 150 patients were recruited. Of these
patients, 83 (55.3%) were from the Accident and
Emergency Department and 67 (44.7%)
were from surgical out-patient clinics. Recruitment
was done in both locations during the mornings or
afternoons of 23, 24 and 26 February, and 2 and 6
March 2015.
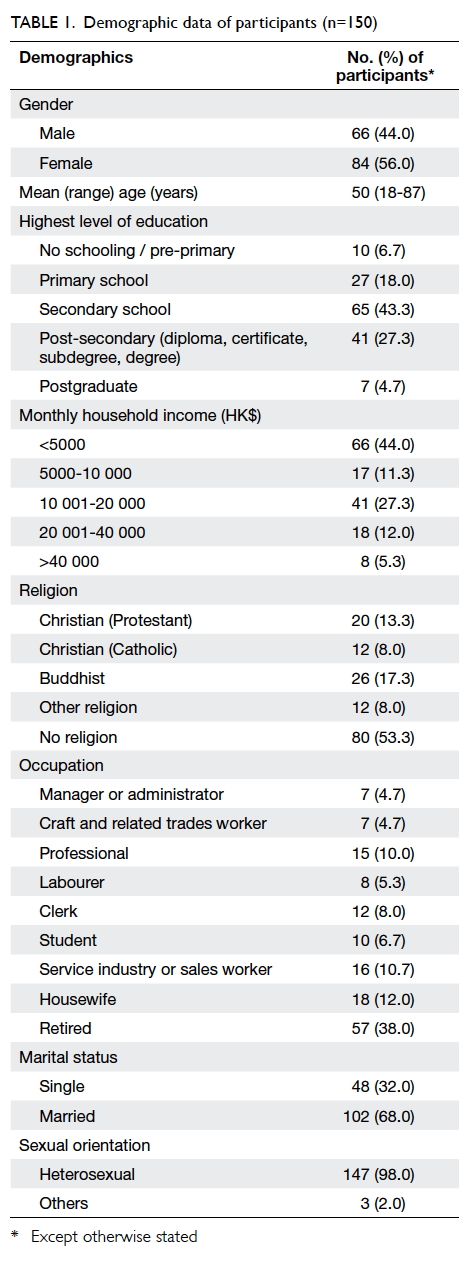
There were similar numbers of women (56.0%)
and men (44.0%). Their mean age was 50 (range,
18-87) years. The majority (75.3%) had completed
a secondary or higher level of education. Over half
(53.3%) were non-religious, and approximately 40%
were retired. The majority of men (63.6%, 42/66)
and women (71.4%, 60/84) were married. Almost all
participants (98.0%, n=147) declared themselves as
heterosexual (Table 1).
Perception of intimate physical examination and preference for physician gender
In addition to our definitions of IPE, significantly
more women than men also found chest examination
of the respiratory system to be intimate (44.0%,
37/84 women vs 13.6%, 9/66 men; P<0.01). Among
the entire sample, upper limb, lower limb, and
abdominal examinations were also considered to
be intimate by five (3.3%), 14 (9.3%), and 19 (12.7%)
participants, respectively. Overall, 42 (50.0%)
women preferred a female doctor for IPE; only
one (1.2%) preferred a male doctor (Table 2). The
only significant determining factor for women
preferring a female doctor for IPE was the absence
of prior experience of IPE (P=0.04); notable but non-significant
determining factors included younger age
(P=0.09) and being unmarried (P=0.10). For men, 42
(63.6%) participants did not have any preference for
physician gender and 21 (31.8%) would prefer a male
doctor (Table 2). No significant determining factors
for men preferring either a male or female doctor for
IPE were identified.
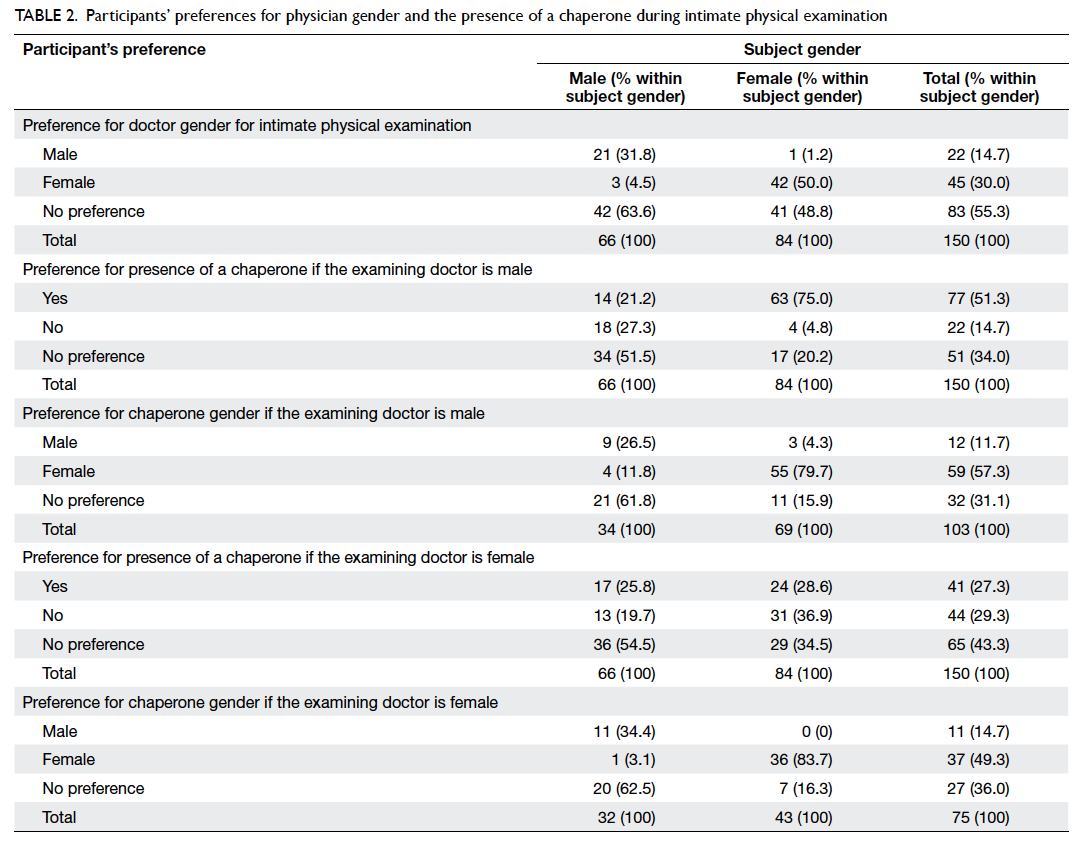
Table 2. Participants’ preferences for physician gender and the presence of a chaperone during intimate physical examination
Previous experiences of intimate physical
examination and general preferences for
chaperoned examination
Of the 150 participants, 115 (76.7%) reported
previous experience of IPE: 42 were men (63.6%
of male participants) and 73 were women (86.9%
of female participants). A large majority (90.7%,
136/150) of the participants considered the
presence of a chaperone appropriate during IPE,
and 84.0% (126/150) felt that doctors, irrespective of
gender, should always ask if the patient would like
a chaperone. This contrasted with the experience
of those who had had previous IPE of whom only
72.6% (53/73) of women and 35.7% (15/42) of men
reported having been chaperoned. For those whose
previous IPE was unchaperoned, 75.0% (15/20) of
women and 44.4% (12/27) of men would actually
prefer to be chaperoned. Interestingly, participants
with prior experience of IPE, irrespective of gender,
were significantly more likely to want a chaperone
when examined by a male doctor (57.4% with vs
28.6% without; P<0.01) but not a female doctor
(28.7% with vs 25.7% without; P=0.87) when
compared with those with no such experience. Most
participants (72.7%, 109/150) regarded health care
workers as suitable chaperones, and 52.7% (79/150)
would also consider a family member, and 20.0%
(30/150) a friend to be appropriate.
The most commonly cited reasons for
preferring a chaperone included the availability of an
objective account should any legal issue arise (61.3%,
92/150), protection against sexual harassment
by the doctor (48.0%, 72/150), and psychological
support (43.3%, 65/150) [Fig a]. The most commonly cited reasons for not having a chaperone included
embarrassment (34.7%, 52/150); significantly more
men (43.9%, 29/66) than women (27.4%, 23/84)
considered a chaperone’s presence embarrassing
(P=0.03). Furthermore, 26.0% of the participants
(39/150) felt that the presence of a chaperone would
undermine their privacy (Fig b).
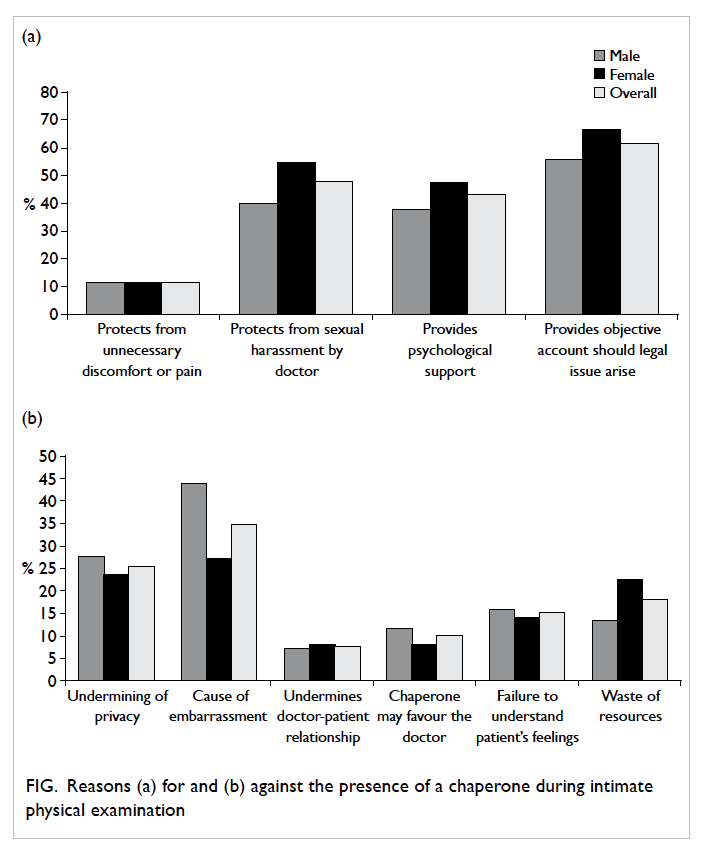
Figure. Reasons (a) for and (b) against the presence of a chaperone during intimate physical examination
Women’s preferences for chaperoned
intimate physical examination
The majority of women (75.0%, 63/84) would prefer
a chaperone to be present when being examined
by a male doctor, and 79.7% (55/69) of female
respondents preferred that chaperone to be female
(Table 2). Even when being examined by a female doctor, 28.6% (24/84) would still prefer to be
chaperoned (Table 2). Women aged between 40 and 59 years were significantly more likely than other
age-groups to prefer chaperoned IPE when examined
by a female doctor (P=0.04). Other demographic
factors—including education level, income, religion
and marital status—were not significantly associated
with any particular preferences.
Men’s preferences for chaperoned intimate
physical examination
More than half of the men had no specific preference,
regardless of physician gender. There was, however,
a proportion who would want to be chaperoned
when examined by a male (21.2%, 14/66) or female
(25.8%, 17/66) doctor (Table 2). Men who wished to be chaperoned when examined by a male doctor
were significantly more likely to also prefer being
chaperoned when examined by a female doctor
(P<0.01). Of note is that a great majority of the men
who preferred chaperoned IPE when examined by a
male doctor indicated that chaperones could provide
an objective account should a legal issue arise
(85.7%, 12/14). There were no significant differences
in terms of demographic variables between the ‘no
preference’, ‘no chaperone’, and ‘prefer chaperone’
groups, regardless of the examining doctor’s gender.
Discussion
Our results highlighted the different views of male
and female subjects in this locality. The majority of
our female patients would prefer to be chaperoned
when examined by a male doctor, and previous
experience of IPE appeared to enforce such a
tendency. This finding is consistent with those from
other countries.4 8 12 Interestingly, and somewhat
unexpectedly, a substantial minority of women would
still prefer to be chaperoned when examined by a
female doctor. Another noteworthy finding was that
male participants who preferred a chaperoned IPE
by a male doctor would also hold a similar preference
when examined by a female doctor, and that their
most commonly cited reason was the availability of
an objective account in case of medicolegal disputes.
This was despite concerns about personal privacy
and feelings of embarrassment.
Our findings compare well with the situation
in the United Kingdom13 and Australia14 where the majority of patients were aware of and would prefer
the practice. When compared with a similar study
conducted at the Emergency Department in the
US, however, we found that patients in
Hong Kong were more likely to prefer chaperoned
IPE when examined by a doctor of the opposite sex
(male patient–female doctor: 25.8% vs 2-3%; female
patient–male doctor: 75% vs 45-47%).3 Other studies
found that physician gender had a variable impact
on female patient’s preference for a chaperone.10
Our findings suggest a generally higher degree of
acceptance of, if not expectation for, the presence
of a medical chaperone in Hong Kong, although
differences in study setting, subject profile, and
study definitions of IPE limit the validity of such
comparisons.
The reported experiences of participants
who have had previous IPE indicate that their
expectations have not been met on a number of
occasions. Several reasons have been suggested
for the inadequate use of chaperones including,
inter alia, the shortage of nursing staff to act as
chaperones,15 and a general lack of awareness.16 This is certainly an area for improvement in our health
care setting. In this regard, it is important to note
that some patients would also consider examinations
of the abdomen and limbs to be intimate, and that
chaperones may still be preferred even when the
physician and patient are of the same gender. The
Code of Professional Conduct issued by the Medical
Council of Hong Kong states that ‘an intimate
examination of a patient is recommended to be
conducted in the presence of a chaperone to the
knowledge of the patient’.17 ‘Intimate examination’ is
not defined and there is no advice about the impact
of gender. The United Kingdom General Medical Council (GMC)
guidelines nonetheless specify that IPE may include
‘any examination where it is necessary to touch or
even be close to the patient’, and the requirement for
a chaperone should apply whether or not the patient
and doctor are of the same or opposite gender.1
Challenging situations may arise when there is
a shortage of staff or when the patient refuses the
presence of a chaperone. The GMC have provided
some detailed guidance.1
Our study has several limitations. First, the
number of participants was relatively small and our
findings may not be readily generalisable, particularly
outside the public hospital setting, where patients are
likely to be more familiar with their doctor and have
more control over which doctor sees and examines
them. The convenient sampling method that we
adopted may result in systematic bias, skewed
results, and potentially suboptimal generalisability
of our findings. Second, our definition of IPE
encompassed a range of different examinations, and
it might be possible that participants have different
preferences regarding each type. Third, our cohort
consisted of relatively few young subjects (only 15%
were aged <30 years) and this might have affected
our ability to demonstrate any impact of age. Last,
as to the reasons for participants’ preferences, our
questionnaire only provided a short list of options
rather than an open question and this could have
limited the range of responses. Future studies may
focus on patient’s preferences in specific settings
(eg primary care) as well as physician’s practice in
order to inform and promote public and professional
awareness in Hong Kong.
Conclusions
Patients in Hong Kong have a high degree of
acceptance towards the presence of a medical
chaperone. Both female and male patients prefer
such practice regardless of physician gender although
individual patients may value the practice differently.
Doctors are strongly encouraged to discuss the issue
openly with their patients and offer the presence of
a chaperone prior to any IPE; an alternative would
be to put up a sign asking patients to notify the
doctor or other staff if they prefer the presence of a
chaperone during IPE.
Declaration
All authors have disclosed no conflicts of interest.
References
1. General Medical Council. Good medical practice (2013).
Available from: http://www.gmc-uk.org/guidance/good_medical_practice.asp. Accessed 27 Nov 2015.
2. Wai D, Katsaris M, Singhal R. Chaperones: are we
protecting patients? Br J Gen Pract 2008;58:54-7. Crossref
3. Buchta RM. Adolescent females’ preferences regarding use
of a chaperone during a pelvic examination. Observations
from a private-practice setting. J Adolesc Health Care
1986;7:409-11. Crossref
4. Patton DD, Bodtke S, Homer RD. Patient perceptions of
the need for chaperones during pelvic exams. Fam Med
1990;22:215-8.
5. Fiddes P, Scott A, Fletcher J, Glasier A. Attitudes towards
pelvic examination and chaperones: a questionnaire survey
of patients and providers. Contraception 2003;67:313-7. Crossref
6. Simanjuntak C, Cummings R, Chen MY, Williams H, Snow
A, Fairley CK. What female patients feel about the offer of
a chaperone by a male sexual health practitioner. Int J STD
AIDS 2009;20:165-7. Crossref
7. Sinha S, De A, Jones N, Jones M, Williams RJ, Vaughan-Williams E. Patients’ attitude towards the use of a
chaperone in breast examination. Ann R Coll Surg Engl
2009;91:46-9. Crossref
8. Penn MA, Bourguet CC. Patients’ attitudes regarding
chaperones during physical examinations. J Fam Pract
1992;35:639-43.
9. Osmond MK, Copas AJ, Newey C, Edwards SG, Jungmann
E, Mercey D. The use of chaperones for intimate
examinations: the patient perspective based on an
anonymous questionnaire. Int J STD AIDS 2007;18:667-71. Crossref
10. Santen SA, Seth N, Hemphill RR, Wrenn KD. Chaperones
for rectal and genital examinations in the emergency
department: what do patients and physicians want? South
Med J 2008;101:24-8. Crossref
11. Van Hecke O, Jones K. The use of chaperones in general
practice: Is this just a ‘Western’ concept? Med Sci Law
2015;55:278-83. Crossref
12. Teague R, Newton D, Fairley CK, et al. The differing views
of male and female patients toward chaperones for genital
examinations in a sexual health setting. Sex Transm Dis
2007;34:1004-7. Crossref
13. Pydah KL, Howard J. The awareness and use of chaperones
by patients in an English general practice. J Med Ethics
2010;36:512-3. Crossref
14. Baber JA, Davies SC, Dayan LS. An extra pair of eyes: do
patients want a chaperone when having an anogenital
examination? Sex Health 2007;4:89-93. Crossref
15. Price DH, Tracy CS, Upshur RE. Chaperone use during
intimate examinations in primary care: postal survey of
family physicians. BMC Fam Pract 2005;6:52. Crossref
16. Vogel L. Chaperones: friend or foe, and to whom? CMAJ
2012;184:642-3. Crossref
17. Medical Council of Hong Kong. Code of Professional
Conduct. 2009. Available from: http://www.mchk.org.hk/Code_of_Professional_Conduct_2009.pdf. Accessed 30
Aug 2015.