DOI: 10.12809/hkmj144419
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
CASE REPORT
A rare but serious complication of continuous ambulatory peritoneal dialysis: delayed perforation of the colon by the Tenckhoff catheter
PY Chu, FRCR; KL Siu, FRCR
Department of Diagnostic Radiology, Tuen Mun Hospital, Tuen Mun, Hong Kong
Corresponding author: Dr PY Chu (idleadam@hotmail.com)
Case report
A 68-year-old male had end-stage renal failure
due to diabetes mellitus. He underwent Tenckhoff
catheter insertion in 2013 for continuous ambulatory
peritoneal dialysis (CAPD). The catheter was flushed
regularly once a week and was functional in the first
2 months following insertion.
The catheter became blocked 2 months
following insertion after an episode of CAPD
peritonitis. Peritoneal dialysate showed scanty
growth of Stenotrophomonas (Xanthomonas)
maltophilia. Kidney, ureter, and bladder X-ray (KUB)
was ordered to identify catheter tip position that
was subsequently revealed to be in the central part
of the pelvic cavity (Fig 1a). The cause of blockage was suspected to be omental wrap. Omentectomy
was planned and the Tenckhoff catheter was left
in situ; CAPD peritonitis was successfully treated
with antibiotics and the patient was discharged. The
peritoneal membrane was rested for 2 weeks and
the patient maintained on temporary twice-weekly
haemodialysis.
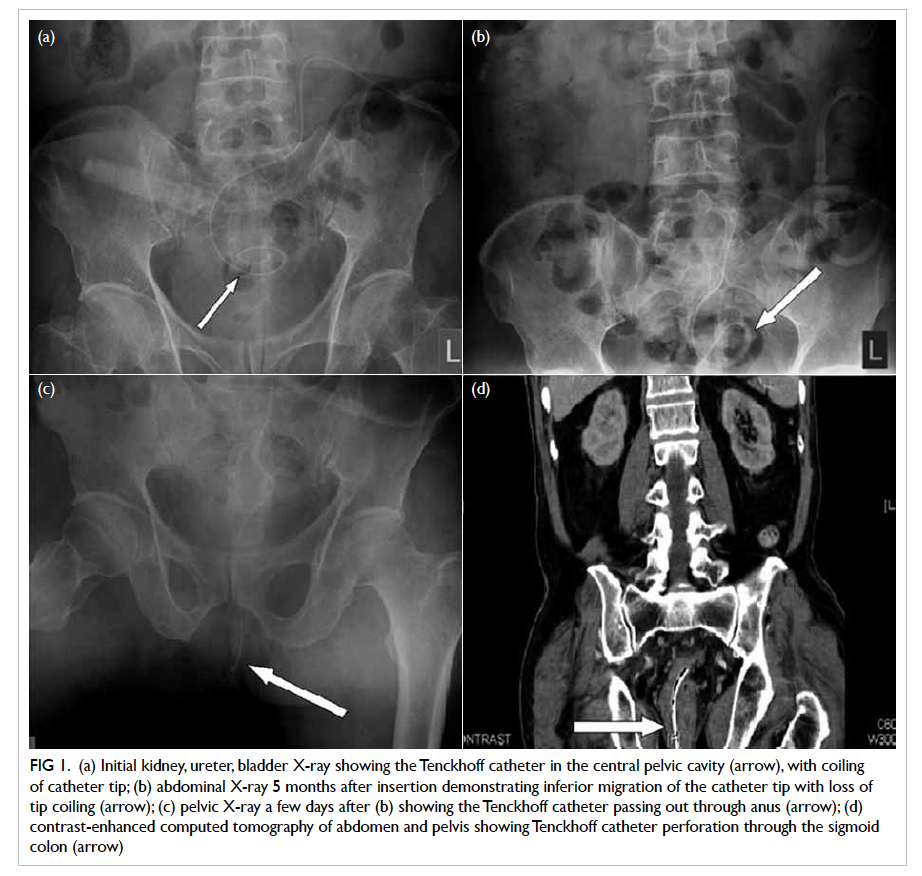
Figure 1. (a) Initial kidney, ureter, bladder X-ray showing the Tenckhoff catheter in the central pelvic cavity (arrow), with coiling of catheter tip; (b) abdominal X-ray 5 months after insertion demonstrating inferior migration of the catheter tip with loss of tip coiling (arrow); (c) pelvic X-ray a few days after (b) showing the Tenckhoff catheter passing out through anus (arrow); (d) contrast-enhanced computed tomography of abdomen and pelvis showing Tenckhoff catheter perforation through the sigmoid colon (arrow)
The patient was admitted to Tuen Mun Hospital
again in early 2014 because of fall. Computed
tomographic (CT) brain revealed a significant left
acute subdural haemorrhage. Urgent craniotomy
with clot evacuation was performed. At that time,
abdominal X-ray demonstrated inferior migration of
the catheter tip with loss of coiling of the distal tip
(Fig 1b). A few days later, the tip of Tenckhoff catheter was noticed in the anus of the patient. Follow-up KUB
confirmed the clinical finding (Fig 1c).
The patient had no symptoms or signs of
acute peritonitis. Contrast-enhanced CT abdomen
and pelvis confirmed perforation of the Tenckhoff
catheter through the sigmoid colon with the tip in
the anus (Fig 1d).
The contrast-enhanced CT demonstrated
Tenckhoff catheter perforation through the sigmoid
colon (Fig 2a) with soft-tissue fibrosis around the catheter at the site of the perforation (Fig 2b). There was no ascites or inflammatory fluid collection.
Contrast enema showed no evidence of contrast
extravasation.
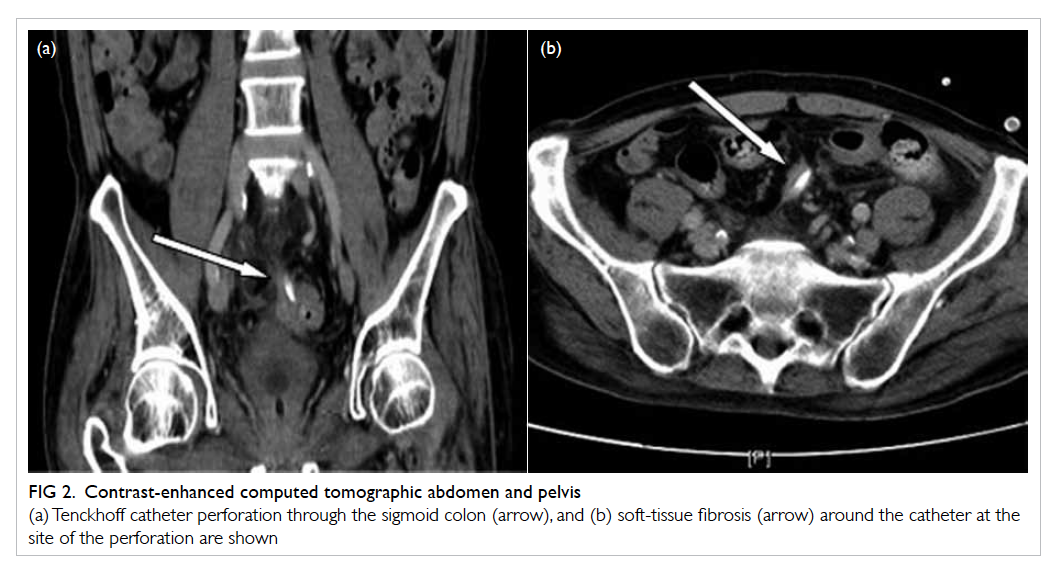
Figure 2. Contrast-enhanced computed tomographic abdomen and pelvis
(a) Tenckhoff catheter perforation through the sigmoid colon (arrow), and (b) soft-tissue fibrosis (arrow) around the catheter at the site of the perforation are shown
The patient became chair-bound after the head
injury. It was decided not to remove or reposition
the Tenckhoff catheter or perform omentectomy.
The rectal side of the catheter was cut short.
Discussion
The pathogenesis of late perforation of the bowel has
been proposed to involve intimate contact between
the peritoneal catheter and the intestinal wall.
The continuous pressure causes local ischaemia,
eventually leading to erosion, laceration, and frank
perforation.1 Lack of fluid in the peritoneal space
after cessation of CAPD predisposes to pressure-induced
necrosis because of loss of the fluid
cushion.2 3 In our patient, perforation was unlikely
when the catheter was in daily use because it did not
come into continuous close contact with the bowel
for any long period of time.4
In most previous studies, delayed perforation
of the bowel was associated with acute peritonitis.1 3 5 6
Kagan and Bar-Khayim1 reviewed the publications
from 1980 to 1995 and identified 24 cases of bowel
perforation during the study period. All cases were
associated with acute peritonitis, with 29% mortality
and significant morbidity. The age of patients ranged
from 22 to 80 years, with no gender predominance.
The time to bowel perforation also ranged broadly
from 0.5 to 96 months after initiation of dialysis.
Sigmoid was the most common site of perforation,
accounting for 14 of the 24 cases. Asymptomatic
delayed perforation of the bowel by Tenckhoff
catheter was rarely reported.7 8
Our patient had acute peritonitis in late 2013.
The KUB showed normal position of Tenckhoff
catheter (Fig 1a) . Since the Tenckhoff catheter was not functioning, omental wrap was suspected.
Later X-rays revealed progressive inferior
migration of the catheter and loss of coiling of the
catheter tip, suggesting perforation of the bowel (Figs 1b and 1c). The CT abdomen and pelvis confirmed
perforation of the sigmoid by the Tenckhoff catheter
in addition to soft-tissue fibrosis around the catheter
tip (Figs 1d and 2).
In our case, in addition to the lack of peritoneal
dialysis fluid, there were probably peritoneal
adhesions arising from previous peritonitis that
resulted in decreased bowel mobility. This in turn
created a predisposition to impingement of bowel
loops by the Tenckhoff catheter that subsequently
led to pressure erosion and perforation.
The patient had no clinical or radiological
evidence of peritonitis, possibly due to plugging of
the bowel perforation site by the catheter and later
sealed off by inflammatory adhesion and fibrosis.
Thus, there was no leakage of faecal material from
the sigmoid into the peritoneal cavity to incite
inflammation and consequent faecal peritonitis.
Occasionally the omentum can also surround and
wall off focal inflammation to prevent extension of
the inflammation to involve the rest of the peritoneal
cavity, as may be seen in the formation of phlegmon
or an abscess in ruptured acute peritonitis.
We present a rare but clinically important case
of delayed perforation of the bowel by Tenckhoff
catheter. According to this case report and several
reported cases, regular flushing of the dialysis
catheter and early removal if not in use (dysfunctional
or not required) may help prevent this complication.
Declaration
No conflicts of interest were declared by the authors.
References
1. Kagan A, Bar-Khayim Y. Delayed decubitus perforation of
the bowel is a sword of damocles in patients on peritoneal
dialysis [Letter]. Nephron 1996;74:232-3. Crossref
2. Brady HR, Abraham G, Oreopoulos DG, et al. Bowel
erosion due to a dormant peritoneal catheter in
immunosuppressed renal transplant recipients. Perit Dial
Int 1988;8:163-5.
3. Rambausek M, Zeier M, Weinreich T, Ritz E, Rau J, Pomer
S. Bowel perforation with unused Tenckhoff catheters.
Perit Dial Int 1989;9:82.
4. Parvin SD, Beaman M. Ileal erosion by the Tenckhoff
catheter. Perit Dial Bull 1985;5:82.
5. Valles M, Cantarell C, Vila J, et al. Delayed perforation
of the colon by a Tenckhoff catheter. Perit Dial Bull 1982;2:190.
6. Thibodeaux LC. Bowel perforation associated with
continuous ambulatory peritoneal dialysis. Nephron
1995;70:265. Crossref
7. Saweirs WW, Casey J. Asymptomatic bowel perforation by
a Tenckhoff catheter. Perit Dial Int 2005;25:195-6.
8. Balaji V, Digard N, Wise MH. Delayed bowel erosion due
to functioning chronic ambulatory peritoneal dialysis
catheter. Nephrol Dial Transplant 1996;11:368-9. Crossref

