Hong Kong Med J 2016 Jun;22(3):237–41 | Epub 6 May 2016
DOI: 10.12809/hkmj154712
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE
Mortality following primary total knee
replacement in public hospitals in Hong Kong
QJ Lee, FHKCOS, FHKAM (Orthopaedic Surgery);
WP Mak, MPHC, FPHKAN;
YC Wong, FHKCOS, FHKAM (Orthopaedic Surgery)
Joint Replacement Centre, Yan Chai Hospital, Tsuen Wan, Hong Kong
Corresponding author: Dr QJ Lee (leejasper@gmail.com)
Abstract
Introduction: More than 2000 total knee
replacements are performed each year in Hong Kong
and more than 10 000 patients are on the waiting list.
How safe is total knee replacement, however? The
aims of the study were to review the mortality of
primary total knee replacement in public hospitals in
Hong Kong and to identify risk factors for mortality
in a high-volume hospital.
Methods: All primary total knee replacements
performed in Hospital Authority hospitals and Yan
Chai Hospital from October 2011 to September 2014
were reviewed. Case-control analysis was performed
for risk factors of total all-cause mortality in total
knee replacement at Yan Chai Hospital.
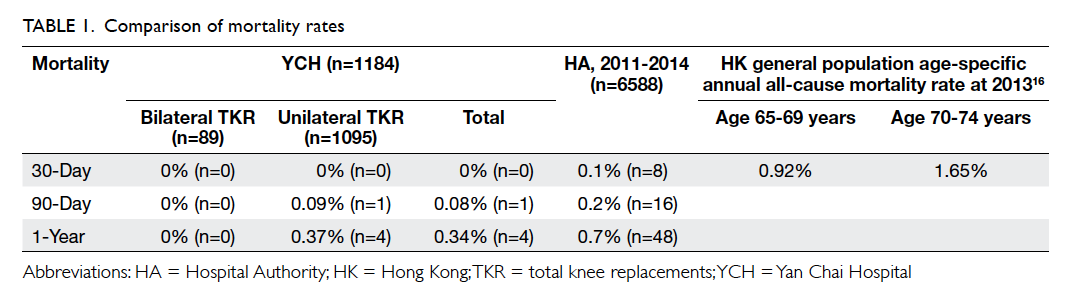
Results: There were 6588 patients in Hospital
Authority hospitals and 1184 in Yan Chai Hospital
(1095 unilateral and 89 bilateral total knee
replacement). The mean follow-up time of patients
in Yan Chai Hospital was 12.8 months. The mortality
at 30 days, 90 days and 1 year was 0%,
0.08%, 0.34% for Yan Chai Hospital; and 0.1%,
0.2%, 0.7% for Hospital Authority hospitals,
respectively. For Yan Chai Hospital, the mean operation-to-death interval was 21 months (range, 1-35
months). The mean age at death was 78 years and
main causes were malignancy (50%) and pneumonia
(21%). Predictors of mortality included age at
surgery, American Society of Anesthesiologists class 3, and preoperative range of motion. Hospital
surgery volume, preoperative co-morbidities, and
postoperative deep vein thrombosis were not
significant factors.
Conclusions: Mortality after primary total knee
replacement was low in public hospitals in Hong
Kong. Patients of older age or poorer general well-being
in terms of poor range of motion or American
Society of Anesthesiologists class 3 should be
in optimal health before surgery and counselled
about the higher mortality rate. A citywide joint
replacement registry may help monitor and analyse
postoperative total knee replacement mortality
specific to our locality.
New knowledge added by this study
- Preoperative range of motion may be predictive of mortality in primary total knee replacement.
- Proper preoperative optimisation of general health and counselling is necessary before primary total knee replacement.
Introduction
More than 2000 primary total knee replacements
(TKR) are performed in Hong Kong each year and
more than 10 000 patients are on the waiting list for
TKR at public hospitals. With an ever-increasing
waiting list, joint replacement centres with high
surgery volume have been set up in public hospitals.
More such centres are planned in the future to tackle
the ageing population and rising demand. As one of
the most popular elective ‘ultra-major’ surgeries,
how safe is primary TKR?
According to various knee replacement
registries, 30-day mortality of TKR ranges from
0.2% to 0.4%, 90-day mortality 0.4% to 0.7%, and
1-year mortality 1% to 2%.1 2 3 4 5 6 7 8 Risk factors for post-TKR mortality include age at operation, male sex,
too high or low body mass index, American Society
of Anesthesiologists (ASA) class 3 to 4, presence
of co-morbidities, and simultaneous bilateral
surgery.1 2 3 4 6 7 8 9 10 11 12 There are a lack of similar data for the
Asian population, however, and the risk of mortality
in a high-volume hospital has not been described
locally. The aims of the study were to review the
mortality of primary TKR in Hong Kong and to
identify risk factors of post-TKR mortality in a high-volume
hospital.
Methods
Data retrieval
All primary TKR performed in public hospitals
(Hospital Authority) and all primary TKR at the
authors’ institute (Yan Chai Hospital, YCH) from
October 2011 to September 2014 were reviewed.
Data retrieval for all public hospitals was performed
with the Clinical Data Analysis and Reporting System.
Procedure code for retrieval was “81.54 TOTAL
KNEE REPLACEMENT”. Data of patients at our institute were retrieved additionally with
Clinical Management System of the Hospital
Authority. The medical records of all deceased cases
before September 2015 were reviewed.
Data analyses
The primary outcome measures were 30-day, 90-day, and
1-year mortality. Correlation
coefficient between 30-day, 90-day, and 1-year
mortality and annual surgery volume of all
public hospitals was calculated with Pearson
test. From data of YCH, comparisons were made
between the mortality of unilateral TKR and
simultaneous bilateral TKR. Case-control analysis
was performed for possible risk factors of primary
TKR total mortality. A control group included non-mortality
cases of all simultaneous bilateral TKR
in the same period and all unilateral primary TKR
performed from October 2012 to March 2013. The
latter period was chosen to allow a 1-year ‘run-in’
time for the newly established joint replacement
centre that commenced operation in October 2011.
All bilateral cases were used due to their relative
scarcity. Chi squared test and Fisher’s exact test were
used for univariate analysis, and multiple logistic
regression was used for multivariate analysis. Final
model for multiple logistic regression was identified
by backward elimination. A P value of <0.05 was
considered statistically significant.
Results
There were 6588 primary TKR in 15 public hospitals
and 1184 primary TKR at YCH (1095 unilateral and
89 bilateral). The 30-day, 90-day, and 1-year mortality
was 0% (n=0), 0.08% (n=1), and 0.34% (n=4) for YCH
and 0.1% (n=8), 0.2% (n=16), and 0.7% (n=48) for
all public hospitals (YCH inclusive), respectively
(Table 1). There was no correlation between hospital
surgery volume and 30-day, 90-day, or 1-year
mortality among the 15 public hospitals (R=0.151,
P=0.578; R=0.031, P=0.910; R=0.032, P=0.972, respectively).
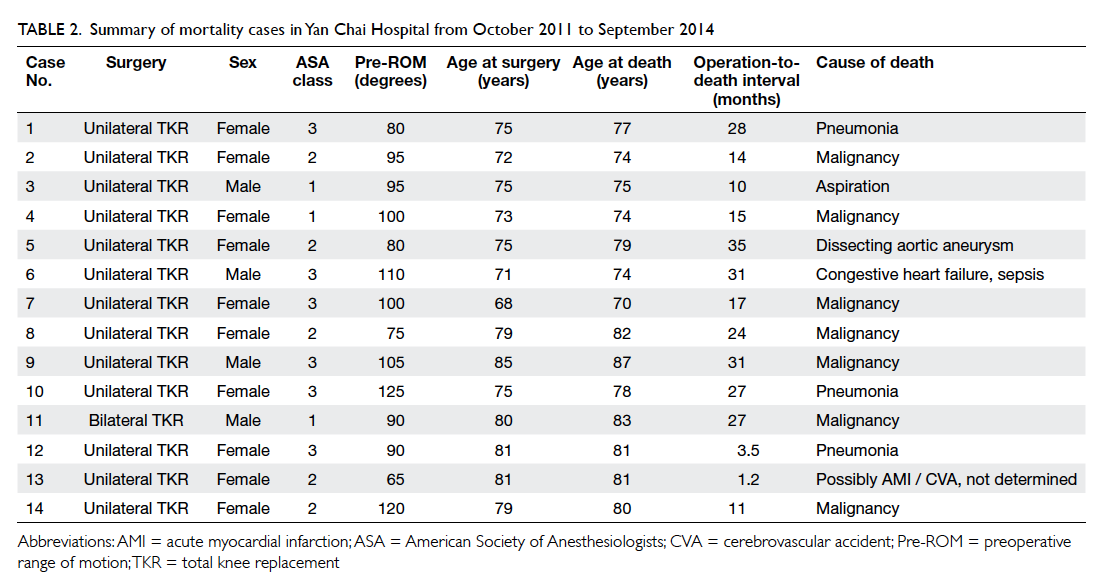
For cases at YCH, the mean follow-up time was
12.8 (range, 4-38) months, the mean operation-to-death
interval was 21 (1-35) months, and the mean
age at death was 78 (70-87) years. Main causes of
death were malignancy (50%) and pneumonia (21%)
[Table 2]. Significant predictors of total mortality
identified by univariate analysis included age at
operation, preoperative range of motion (ROM), and
ASA class 3; the former two were also confirmed by the
final model of multivariable analysis (Table 3). The
mean age at operation was 76 versus 68 years for
mortality and non-mortality cases while the mean
preoperative ROM was 95 versus 108 degrees, respectively.
Body mass index, co-morbidities, deep vein thrombosis (DVT) prophylaxis,
and postoperative DVT did not differ significantly
between the two groups. Preoperative Western
Ontario and McMaster Universities Arthritis Index
(WOMAC), Knee Society score (KSS), and function score (FS) were also not significantly
different. There was no significant difference in
30-day, 90-day, or 1-year mortality for bilateral TKR
versus unilateral TKR (Table 1).
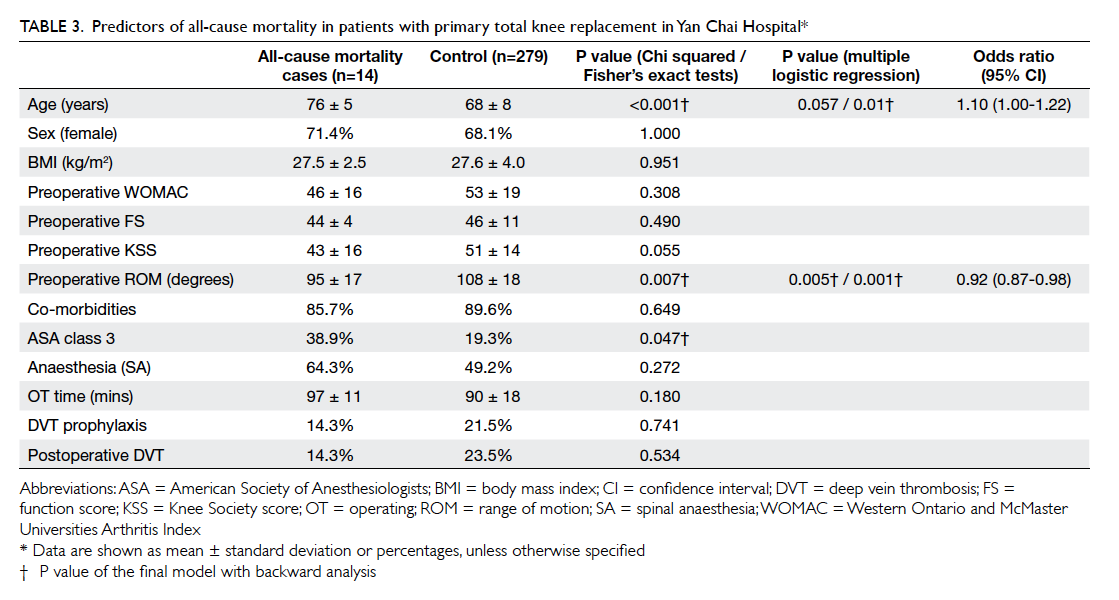
Table 3. Predictors of all-cause mortality in patients with primary total knee replacement in Yan Chai Hospital
Discussion
Mortality rate
The 30-day, 90-day, and 1-year mortality in Hong
Kong public hospitals was 0.1%, 0.2%, and 0.7%,
respectively. These compared favourably with data
of large national joint registries of other countries:
0.2% to 0.4%, 0.4% to 0.7%, and 1% to 2%, respectively.1 2 3 4 5 6 7 8 There is no definitive explanation for such findings but
several possibilities exist. First, TKR is still mostly
considered a ‘risky’ and major operation in Hong
Kong such that the popularity of such surgery
remains low compared with other countries. In
2013, the incidence of primary TKR was around
4 per 10 000 population in Hong Kong (estimated
from data of the present study) compared with 12
in the United Kingdom, 14 in Sweden, and 19 in
Australia.13 14 15 Lower operation incidence implies
stricter selection criteria for operation. Second, the
mortality of the general population of Hong Kong is
known to be among the lowest in the world16; our
findings may partly reflect the low mortality of the
general population. Third, easy access to medical
treatment in Hong Kong might facilitate timely
intervention of early complications, hence reducing
postoperative mortality. Whatever the explanation,
the lower mortality indicates that primary TKR in
Hong Kong are safe and conform to international
standards.
One-year mortality following primary TKR
in Hong Kong was lower than the mortality of the
general population of the same age16 (Table 1).
Similar findings have been shown by other studies.17
It has been suggested that strict selection criteria
for operation meant that those selected were of
better health than the general population. It was also
hypothesised that pain relief and restored function
would have a positive effect on a patient’s overall
health, hence a lower mortality in the long term.
Nevertheless, 1-year may be too short a period for
the latter effect to be obvious.
Mortality risk factors
In the present study, older age at operation was
identified as a significant risk factor. This is consistent
with findings in other studies.2 3 4 6 7 8 9 11 18 Some studies
have reported higher 30-day,2 3 4 higher 90-day,6 7 and even higher total mortality in the long term.9 11 With an ageing population and higher life expectancy,
there will be more patients with older age in future
who undergo TKR. To date, there is no consensus
on an age limit for the procedure. It is agreed that
patients in their 80s or even 90s could still benefit
from the surgery18 provided the associated higher
mortality is well explained and accepted.
The presence of co-morbidities was not a
significant predictor of mortality in the present
study. Rather, the poor control or the severity of
co-morbidities in terms of ASA class 3 was found
by univariate analysis to be a significant factor.
There is evidence that patients with only specific
co-morbidities such as cardiovascular disease will
have higher mortality.1 4 6 7 8 19 In addition, higher 30-day mortality,3 90-day mortality,6 and total mortality8 9 have been associated with higher ASA class.
The lack of significance of ASA class 3 in multivariate
analysis in our study suggests an underlying
confounding factor. Analysis by t test showed that
the age of patients with ASA class 3 was significantly
older (72 vs 67 years, P<0.001). Thus in the present
study, ASA class was confounded by age at surgery.
Preoperative ROM was also found to be a
significant factor by univariate and multivariate
analyses in the present study. This might be a
novel finding. The exact explanation for such
an association requires exploration by further
study. One possibility is that preoperative ROM
predicts postoperative ROM20 that in turn affects
postoperative ambulation and function. As
mentioned above, it was hypothesised that restored
ambulation and function can have a positive effect
on a patient’s overall health, hence a lower mortality.
There are studies which reported an association
between mortality and postoperative knee function.
The latter was in terms of preoperative ambulatory
status,8 postoperative ambulatory status, and
postoperative WOMAC pain score.11 No knee score
in the present study was found to be a significant
predictor of mortality, however. One explanation
could be that FS, WOMAC, and a large portion of
KSS are patient-reported outcomes whereas ROM
is an objective measurement; the more objective the
measurement, the better it might be in predicting a
secondary outcome such as mortality.
Although bilateral TKR has been found by
several studies to have a higher mortality rate,12 21 22 it
was not a significant predictor in the present study.
Our institute performed bilateral TKR in selected
patients with mild and well-controlled co-morbidities
and younger age. Also, the fast-track rehabilitation
protocol was used with an average length of hospital
stay of 9.6 days (authors’ unpublished data). The
results of analysis might reflect the equivalent
safety of bilateral TKR with careful patient selection
and fast-track rehabilitation. Many studies have
demonstrated equal mortality for bilateral TKR with
careful patient selection and a fast-track protocol.23 24
The present study has some limitations. First,
due to inconsistent documentation across all public
hospitals, data for case-control analysis for predictors
of mortality were obtained from patients at our
institute only. The smaller sample size limited the
power of analysis of the present study. Second, since
70% of the mortality of our institute occurred more
than 1 year after surgery and the mean operation-to-death
interval was 21 months, analysis for predictors
of mortality was performed on total mortality rather
than 30-day, 90-day, or 1-year mortality. The very
low early mortality in our institute and in Hong Kong
means that a more powerful analysis of mortalities
within 1 year may require a much larger sample size.
This calls for a citywide joint replacement registry
in which there is unified and detailed documentation
of preoperative patient parameters, operative details,
and postoperative outcome measurements. Such
registries have already been established nationwide
for 11 years in the United Kingdom13 and for 40 years
in Sweden.14 Third, data for other known significant
predictors of all-cause mortality, such as smoking and
alcoholism, were not analysed. These factors might
have confounded the present study. Since these
factors are not known to be associated with age or
preoperative ROM, the influence of these potential
confounders on the conclusion of the present study
should be insignificant. Lastly, the period chosen for
selection of the control group did not fully match the
death cases. This may have introduced confounding
factors or made the groups incomparable. Since there
was no change in the indications for surgery, surgical
practice or rehabilitation protocol during the study
period, and the sampled control should be representative
of the target population.
Conclusions
Mortality after primary TKR was low in public
hospitals in Hong Kong. Patients of older age or
poorer general health in terms of poor ROM or ASA
class 3 should be in optimal health before surgery and
counselled about the higher mortality rate. The role
of a pre-admission clinic and fast-track rehabilitation
in contributing to the lower mortality in our institute
should be further explored. A citywide joint
replacement registry may help monitor and analyse
post-TKR mortality specific to our locality.
Declaration
All authors have disclosed no conflicts of interest.
References
1. Hunt LP, Ben-Shlomo Y, Clark EM, et al. 45-Day mortality
after 467,779 knee replacements for osteoarthritis from
the National Joint Registry for England and Wales: an
observational study. Lancet 2014;384:1429-36. Crossref
2. Lie SA, Pratt N, Ryan P, et al. Duration of the increase in
early postoperative mortality after elective hip and knee
replacement. J Bone Joint Surg Am 2010;92:58-63. Crossref
3. Belmont PJ Jr, Goodman GP, Waterman BR, Bader JO,
Schoenfeld AJ. Thirty-day postoperative complications and
mortality following total knee arthroplasty: incidence and
risk factors among a national sample of 15,321 patients. J
Bone Joint Surg Am 2014;96:20-6. Crossref
4. Parvizi J, Sullivan TA, Trousdale RT, Lewallen DG. Thirty-day
mortality after total knee arthroplasty. J Bone Joint
Surg Am 2001;83-A:1157-61.
5. Pedersen AB, Mehnert F, Sorensen HT, Emmeluth
C, Overgaard S, Johnsen SP. The risk of venous
thromboembolism, myocardial infarction, stroke, major
bleeding and death in patients undergoing total hip and
knee replacement: a 15-year retrospective cohort study of
routine clinical practice. Bone Joint J 2014;96-B:479-85. Crossref
6. Singh JA, Lewallen DG. Ninety-day mortality in patients
undergoing elective total hip or total knee arthroplasty. J
Arthroplasty 2012;27:1417-1422.e1. Crossref
7. Gill GS, Mills D, Joshi AB. Mortality following primary total
knee arthroplasty. J Bone Joint Surg Am 2003;85-A:432-5.
8. Jämsen E, Puolakka T, Eskelinen A, et al. Predictors of
mortality following primary hip and knee replacement in
the aged. A single-center analysis of 1,998 primary hip and
knee replacements for primary osteoarthritis. Acta Orthop
2013;84:44-53. Crossref
9. Clement ND, Jenkins PJ, Brenkel IJ, Walmsley P. Predictors
of mortality after total knee replacement: a ten-year
survivorship analysis. J Bone Joint Surg Br 2012;94:200-4. Crossref
10. Thornqvist C, Gislason GH, Køber L, Jensen PF, Torp-Pedersen C, Andersson C. Body mass index and risk of
perioperative cardiovascular adverse events and mortality
in 34,744 Danish patients undergoing hip or knee
replacement. Acta Orthop 2014;85:456-62. Crossref
11. Lizaur-Utrilla A, Gonzalez-Parreño S, Miralles-Muñoz FA,
Lopez-Prats FA. Ten-year mortality risk predictors after
primary total knee arthroplasty for osteoarthritis. Knee
Surg Sports Traumatol Arthrosc 2015;23:1848-55. Crossref
12. Restrepo C, Parvizi J, Dietrich T, Einhorn TA. Safety of
simultaneous bilateral total knee arthroplasty. A meta-analysis.
J Bone Joint Surg Am 2007;89:1220-6. Crossref
13. 11th Annual Report. National Joint Registry for England,
Wales and Northern Ireland. UK: National Joint Registry;
2014: 73-121.
14. Annual Report 2013. The Swedish Knee Arthroplasty
Register; 2013: 2-55.
15. Australian Orthopaedic Association National Joint
Replacement Registry. Annual Report. Adelaide: Australian
Orthopaedic Association; 2014: 126-207.
16. The mortality trend in Hong Kong, 1981 to 2013. Hong
Kong Monthly Digest of Statistics; 2014: 4-10.
17. Lovald ST, Ong KL, Lau EC, Schmier JK, Bozic KJ,
Kurtz SM. Mortality, cost, and health outcomes of total
knee arthroplasty in Medicare patients. J Arthroplasty
2013;28:449-54. Crossref
18. Miric A, Inacio MC, Kelly MP, Namba RS. Can total knee
arthroplasty be safely performed among nonagenarians?
An evaluation of morbidity and mortality within a total
joint replacement registry. J Arthroplasty 2014;29:1635-8. Crossref
19. Robertsson O, Stefánsdóttir A, Lidgren L, Ranstam J.
Increased long-term mortality in patients less than 55
years old who have undergone knee replacement for
osteoarthritis: results from the Swedish Knee Arthroplasty
Register. J Bone Joint Surg Br 2007;89:599-603. Crossref
20. Parsley BS, Engh GA, Dwyer KA. Preoperative flexion.
Does it influence postoperative flexion after posterior-cruciate-retaining total knee arthroplasty? Clin Orthop
Relat Res 1991;(275):204-10.
21. Hu J, Liu Y, Lv Z, Li X, Qin X, Fan W. Mortality and
morbidity associated with simultaneous bilateral or staged
bilateral total knee arthroplasty: a meta-analysis. Arch
Orthop Trauma Surg 2011;131:1291-8. Crossref
22. Fu D, Li G, Chen K, Zeng H, Zhang X, Cai Z. Comparison
of clinical outcome between simultaneous-bilateral and
staged-bilateral total knee arthroplasty: a systematic review
of retrospective studies. J Arthroplasty 2013;28:1141-7. Crossref
23. Kim YH, Choi YW, Kim JS. Simultaneous bilateral
sequential total knee replacement is as safe as unilateral
total knee replacement. J Bone Joint Surg Br 2009;91:64-8. Crossref
24. Powell RS, Pulido P, Tuason MS, Colwell CW Jr, Ezzet
KA. Bilateral vs unilateral total knee arthroplasty: a
patient-based comparison of pain levels and recovery of
ambulatory skills. J Arthroplasty 2006;21:642-9. Crossref