Hong Kong Med J 2016 Jun;22(3):210–5 | Epub 22 Apr 2016
DOI: 10.12809/hkmj154602
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE
Is pain from mammography reduced by the use
of a radiolucent MammoPad? Local experience in
Hong Kong
Helen HL Chan, FHKCR, FHKAM (Radiology)1;
Gladys Lo, FHKCR, FHKAM (Radiology)1;
Polly SY Cheung, FCSHK, FHKAM (Surgery)2
1 Department of Diagnostic and Interventional Radiology, Hong Kong
Sanatorium & Hospital, Happy Valley, Hong Kong
2 Private practice, Hong Kong
Corresponding author: Dr Helen HL Chan (chanhlh@yahoo.com)
Abstract
Introduction: Screening mammogram can decrease
the mortality of breast cancer. Studies show that
women avoid mammogram because of fear of pain,
diagnosis, and radiation. This study aimed to evaluate
the effectiveness of a radiolucent pad (MammoPad;
Hologic Inc, Bedford [MA], US) during screening
mammogram to reduce pain in Chinese patients and
the possibility of glandular dose reduction.
Methods: This case series was conducted in a private
hospital in Hong Kong. Between November 2011
and January 2012, a total of 100 Chinese patients
were recruited to our study. Left mammogram was
performed without MammoPad and served as a
control. Right mammogram was performed with
the radiolucent MammoPad. All patients were then
requested to complete a simple questionnaire. The
degree of pain and discomfort was rated on a 0-10
numeric analogue scale. Significant reduction in
discomfort was defined as a decrease of 10% or more.
Results: Of the 100 patients enrolled in this study, 66.3% of women reported at least a 10% reduction in the level of discomfort with the use of MammoPad. No statistical differences between age, breast size, and the level of discomfort were found.
Conclusion: The use of MammoPad significantly
reduced the level of discomfort experienced during
mammography. Radiation dose was also reduced.
New knowledge added by this study
- Pain and discomfort associated with mammography is reduced with the use of MammoPad.
- The glandular dose for mammography is also reduced.
- MammoPad is now used in all our patients. There are fewer complaints about pain during mammography.
Introduction
Screening mammography is the only known
scientifically proven method that can decrease the
mortality of breast cancer.1 2 Although most women
are informed of the importance of mammography, a
significant number avoid this screening procedure.
The three most common reasons given are fear of
pain, fear of the mammogram results, and fear of
radiation.
Among these three reasons, pain and discomfort
appear to be the most common, especially in
those with a poor experience.3 Although
most pain occurs during breast compression,
reducing compression by the technician had no
significant effect on the discomfort of mammography.
Studies have quoted different methods to relieve
patient anxiety and to reduce pain and discomfort
during the procedure. These included a thorough
explanation of the procedure,4 topical application
of 4% lidocaine gel to the skin of the chest before
mammography,5 self-controlled breast compression
during mammography,6 and the use of a radiolucent
pad (MammoPad; Hologic Inc, Bedford [MA], US)
during mammography.7 8 Oral acetaminophen and
ibuprofen were shown to be of no significant effect
in relieving discomfort during mammography.
Poulos and Rickard9 reported that decreasing the
compression force did not significantly reduce
discomfort.
Asian patients might have more fibroglandular
tissue in their breasts that thus appear to have a
higher density on screening mammogram. Whether
or not they experience more discomfort during
mammography is unknown. MammoPad is a soft,
compressible cushion that provides a softer and
warmer surface for taking mammography. We believe
it may improve compliance with mammography
among Asian patients. We performed a prospective
study to evaluate the effectiveness of MammoPad
used during screening mammogram to reduce pain
in Asian patients. The possibility of glandular dose
reduction was also assessed.
Methods
Between November 2011 and January 2012, a
total of 100 patients were recruited to our study.
The inclusion criteria included Chinese women
who were asymptomatic and referred for routine
breast screening. Patients prescribed regular oral
contraceptive pills and those with a family history of
breast cancer were also included in our study. There
was no age limitation. The included participants
were 32 to 70 years old, with a mean age of 49.7
(± standard deviation, 7.3) years. Women with known
breast cancer, who presented with breast lump or had
prior breast surgery, were excluded. After obtaining
informed consent, screening mammogram was
performed with the standard craniocaudal (CC) and
mediolateral oblique (MLO) views. For each patient,
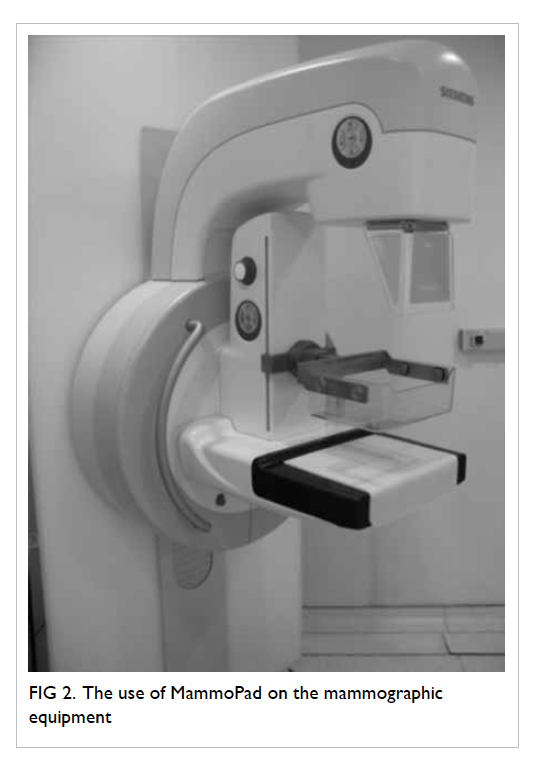
the left breast was imaged without MammoPad
and served as a control. The MammoPad was then
placed on the surface of the digital detector of the
mammographic equipment (Inspiration/Novation,
Siemens, Germany) and the right mammogram was
performed (Figs 1 and 2). The level of compression
was determined by the experienced mammographic
technician. On completion of the procedure, all
patients were requested to complete a simple
questionnaire (Appendix). The degree of pain and
discomfort (including coldness and hardness of the
mammogram compression device) was assessed by a
0-10 numeric analogue scale. Three patients refused
to participate in the study.
Declaration
All authors have disclosed no conflicts of interest.
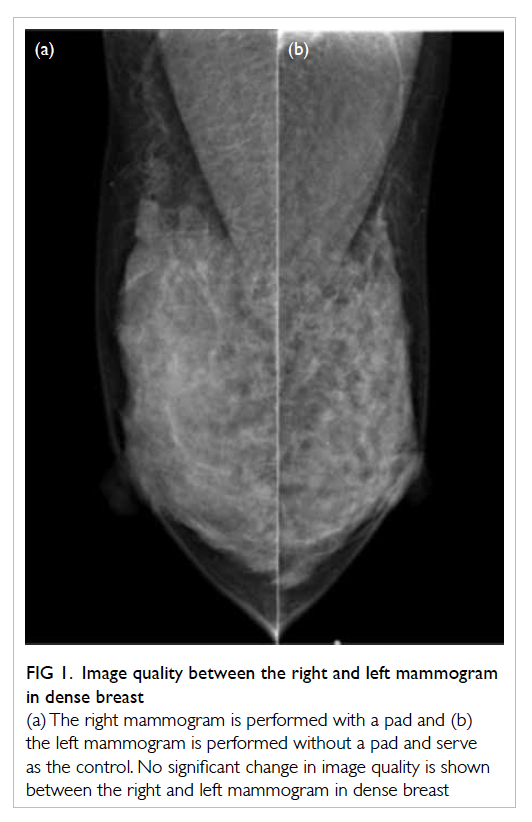
Figure 1. Image quality between the right and left mammogram in dense breast
(a) The right mammogram is performed with a pad and (b) the left mammogram is performed without a pad and serve as the control. No significant change in image quality is shown between the right and left mammogram in dense breast
The image quality of the mammograms with
and without MammoPad was assessed by two
experienced radiologists who had mammographic
training (one radiologist had >20 years of and another
radiologist >10 years of mammography reading
experience). The two radiologists were blinded as to
which side of the mammogram was performed with
and without MammoPad. Since the MammoPad
was radiolucent, its presence was not evident on the
mammogram.
The mammographic assessment was divided
into five categories:
(1) Symmetrical on both sides with satisfactory diagnostic image quality;
(2) Quality of right mammogram image slightly better than the left mammogram but with diagnostic accuracy unaffected;
(3) Quality of left mammogram image slightly better than the right mammogram but with diagnostic accuracy unaffected;
(4) Quality of right mammogram image much better than the left mammogram, affected the diagnostic accuracy, and required repeated mammogram; and
(5) Quality of left mammogram image much better than the right mammogram, affected the diagnostic accuracy, and required repeated mammogram.
(1) Symmetrical on both sides with satisfactory diagnostic image quality;
(2) Quality of right mammogram image slightly better than the left mammogram but with diagnostic accuracy unaffected;
(3) Quality of left mammogram image slightly better than the right mammogram but with diagnostic accuracy unaffected;
(4) Quality of right mammogram image much better than the left mammogram, affected the diagnostic accuracy, and required repeated mammogram; and
(5) Quality of left mammogram image much better than the right mammogram, affected the diagnostic accuracy, and required repeated mammogram.
Any disagreement about the findings was
resolved through consensus between the radiologists.
Statistical analysis
Significant reduction in discomfort of the
mammography was defined as a decrease in
discomfort by 10% or more. The mean differences
in continuous variables between the mammograms
with and without a pad were tested by paired sample
t test. The differences in the percentage of comfort
between groups in density, size, and age were tested
by Chi squared test. A two-tailed P value of <0.05
was considered statistically significant.
Results
Image quality
Among the mammograms compared, 92% of
the images from the two groups with or without
MammoPad had comparable image quality (Fig
1). Only 4% of images from the group without
MammoPad were found to have better image
quality. Another 4% of the images from the group
with MammoPad were noted to have better image
quality. In the 4% of image groups with image quality
differences (either right side better than the left side
or vice versa), two radiologists did not consider
diagnostic accuracy to be affected. The patients with
image quality differences of the right and left side
had follow-up mammograms without MammoPad
performed 1 year later. There was no mammographic
evidence of malignancy in these patients.
For pain and discomfort reduction
The Table shows the comparisons in pain reduction and other measures between the mammograms
with and without a pad. Using paired sample t test,
the mean (± standard deviation) scores for pain (5.7 ± 2.5 vs 4.2 ± 1.8), coldness
(4.0 ± 2.2 vs 2.2 ± 2.1), hardness (3.6 ± 2.4 vs 2.0 ±
2.1), and overall feeling (4.1 ± 2.3 vs 2.6 ± 2.1) were
significantly higher in the group without MammoPad
than the group with MammoPad (all P<0.001). The
thickness was higher in the group with MammoPad
when compared with the group without MammoPad
in both the CC view (57.8 ± 13.8 mm vs 53.1 ± 13.0
mm; P<0.001) and MLO view (54.2 ± 16.6 mm vs
50.9 ± 16.4 mm; P=0.019).
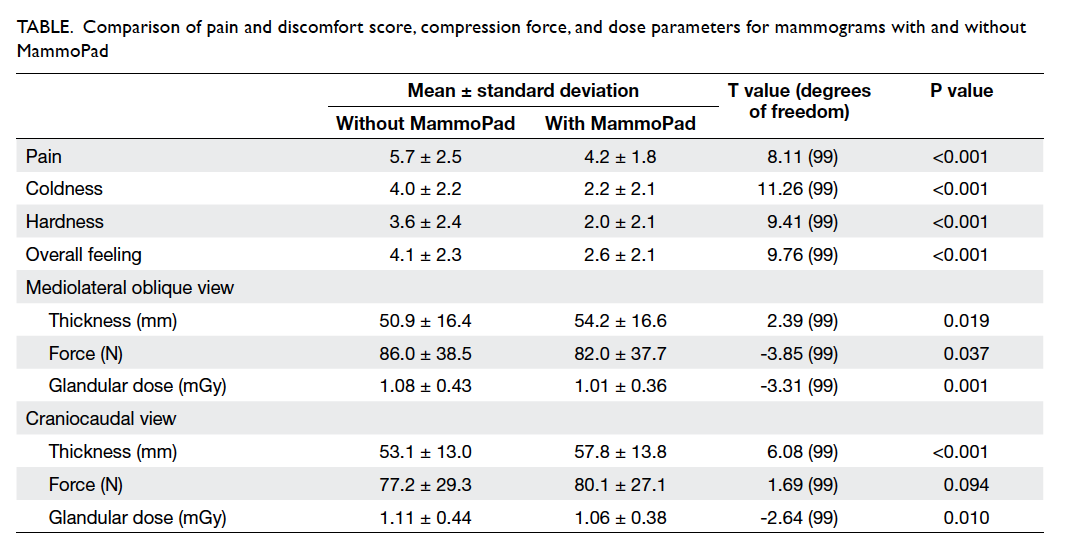
Table. Comparison of pain and discomfort score, compression force, and dose parameters for mammograms with and without MammoPad
Among the 100 patients, 90 of them had
previously undergone mammography of whom 64
(71.1%) reported the mammogram with a pad to
be ‘more comfortable’ or ‘much more comfortable’
than prior studies without a pad. Only 26 (28.9%)
patients reported that the level of discomfort for
mammogram with MammoPad was the same as
prior studies. There was no association between
patient age and comfort during mammography (Chi
squared value=5.81, degrees of freedom [df]=8, P=0.664; Fig 3). Patients with less breast density were more likely to report
‘much more comfortable’ than those patients with
high breast density (Chi squared value=10.3 [df=2],
P=0.006; Fig 4). There was no statistically significant
association between breast size and comfort
during mammography (Chi squared value=4.68
[df=4], P=0.322; Fig 5). All patients preferred using
MammoPad in future mammography.
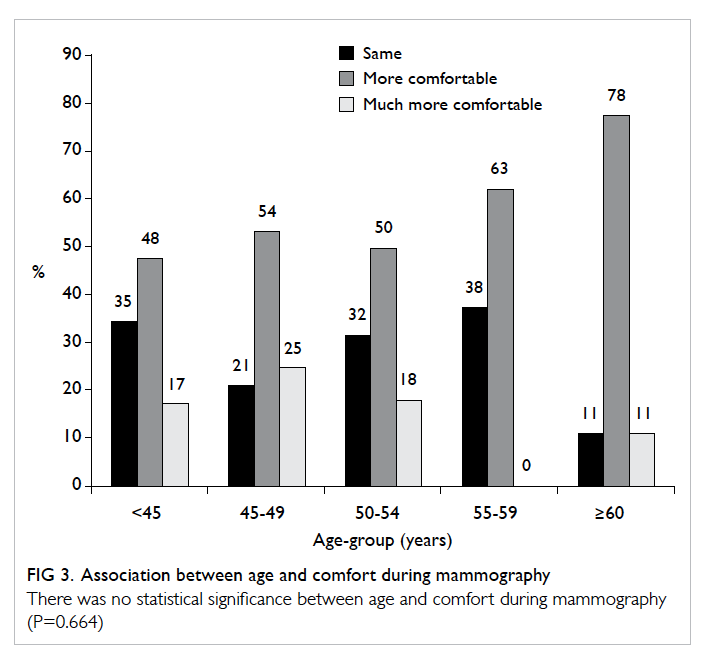
Figure 3. Association between age and comfort during mammography
There was no statistical significance between age and comfort during mammography (P=0.664)
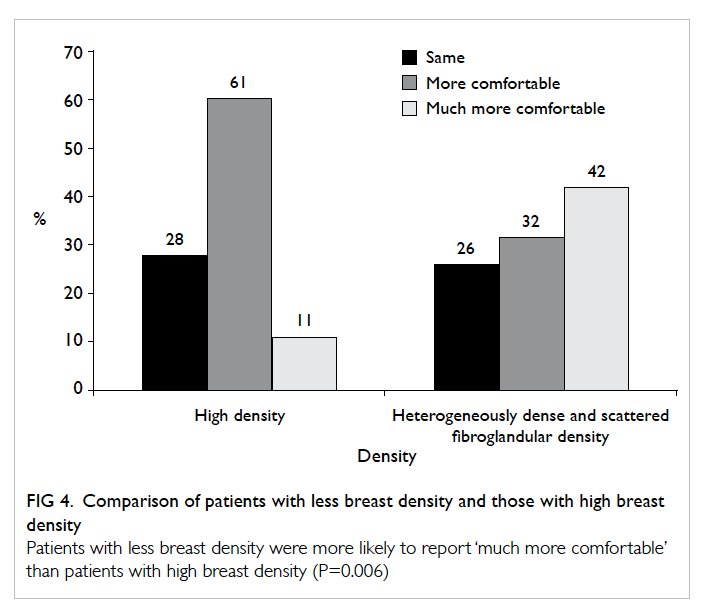
Figure 4. Comparison of patients with less breast density and those with high breast density
Patients with less breast density were more likely to report ‘much more comfortable’ than patients with high breast density (P=0.006)
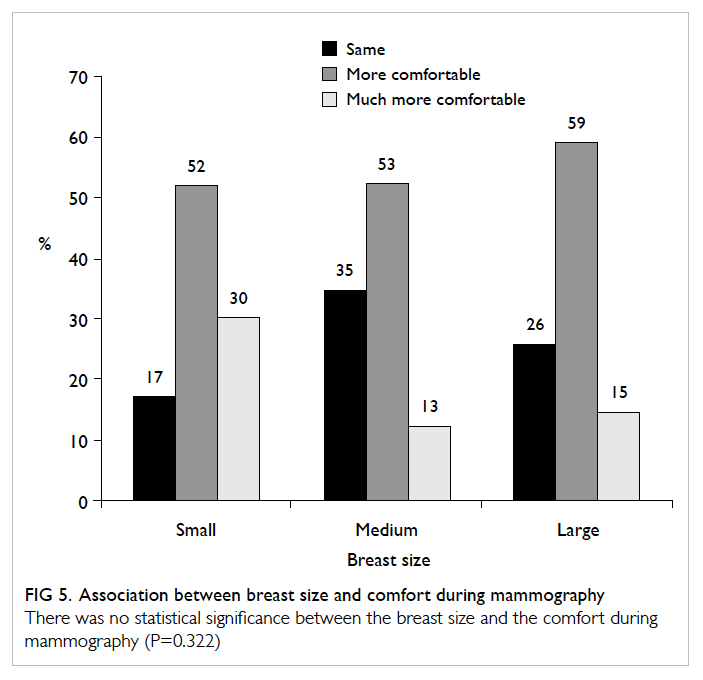
Figure 5. Association between breast size and comfort during mammography
There was no statistical significance between the breast size and the comfort during mammography (P=0.322)
For dosage reduction
The mean glandular dose was higher in the group without
MammoPad than the group with MammoPad in
both views (1.11 ± 0.44 mGy vs 1.06 ± 0.38 mGy for CC view,
and 1.08 ± 0.43 mGy vs 1.01 ± 0.36 mGy for MLO view). For the
group with MammoPad, there was a 4.5% decrease
in dose for the CC view and 6.5% decrease in dose
for the MLO view. The statistical significance was
P=0.01 and 0.001, respectively (Table).
For compression force
There was no statistically significant difference in
the mean compression force in the two groups in the CC
view (80.1 ± 27.1 N vs 77.2 ± 29.3 N; P=0.094).
Reduced compression force in the MammoPad
group was noticed in the MLO view (82.0 ± 37.7 N
vs 86.0 ± 38.5 N; P=0.037) [Table].
Discussion
Breast cancer is the third leading cause of cancer
death among females in Hong Kong, after colorectal
and lung cancers.10 In 2013, a total of 596 women
died from breast cancer, accounting for 10.5% of all
cancer deaths in females.10 Screening mammogram
is proven to be effective in the early detection of
breast cancer. Unfortunately, the utilisation of
screening mammogram in Hong Kong is limited,
partly because there is no government-subsidised
mammographic screening programme. Another
important factor is the discomfort experienced
during mammography.
Various studies have attempted to reduce the
pain and discomfort associated with mammography.
The most promising method to date appears to be
the radiolucent MammoPad. Tabar et al7 reported
that two thirds of women experienced a significant
reduction in pain when the radiolucent cushions
were used during mammography. Markle et al8
reported that use of a radiolucent cushion reduced
discomfort during screening mammogram in 73.5%
of patients.
In our study, we confirmed that the image
quality of the mammograms was unaffected by the
presence of the MammoPad. After review by the
radiologists, diagnostic accuracy was considered
unaffected in the 4% image groups with image
quality differences (either right side better than the
left or vice versa). The difference in image quality was
probably secondary to asymmetrical fibroglandular
tissue thickness in both breasts. In all, 66.3% of our patients reported at least a 10%
reduction in the level of discomfort with the use of
MammoPad. This finding was comparable with the
study performed by Tabar et al.7 In addition, there
was no obvious correlation between age, breast size,
and level of discomfort. Reduced compression force
in the group with MammoPad was noticed in the
MLO view, but not in the CC view.
Unlike the study performed by Dibble et al,11 we
encountered no problem with inadequate positioning
for the mammograms. This may have been because
our technicians were well-trained in the use of the
MammoPad prior to study commencement. No
mammograms required repetition.
With the use of MammoPad, Markle et al8
also reported a 4% decreased dose in the CC view,
but not the MLO view. In our study, there was
a 4.5% decrease in dose for the CC view and 6.5%
decrease in dose for the MLO view. These data were
statistically significant (P<0.05). With the use of the
MammoPad, the compression on breast tissue may
be more evenly distributed and account for the dose
reduction.
Although the improved comfort while using
the MammoPad and the dose reduction during
mammography are encouraging, our study has
several limitations. First, there might have been
patient selection bias. This study was performed
in a private hospital on Hong Kong Island. There
were no similar data available from public hospitals
elsewhere in Hong Kong so comparison was not
possible. In view of the small sample size, the results
might not be representative of the whole screening
population. As a result, there might have been an
inherent patient selection bias. This selection bias
might be minimised if a larger and representative
sample could be obtained. Second, since there is no
routine breast cancer screening programme in Hong
Kong, patients in this study were self-selected and
might be more motivated to undergo mammogram or
be more informed about such procedure. This might
in turn affect the pain and discomfort perception and
subsequent scores. In addition, the scoring system
for pain, coldness, and hardness was a 0-10 numeric
analogue scale system, which is a subjective scoring
system. Patient anxiety may result in a higher pain
score, and thus, a potential measurement bias might
exist. A thorough explanation before performing the
mammogram might help to reduce this bias.
The MammoPad was a single-use device with
obvious hygienic and safety advantages. In the United
States, the MammoPad can be recycled, although
this cannot be achieved in our unit at present. We
might explore the possibility of recycling the device
in future to decrease the environmental impact.
Conclusion
The use of MammoPad significantly reduced the
level of discomfort during mammography. This
should improve compliance with initial and follow-up
mammography. In addition, we demonstrated
radiation dose reduction in both CC and MLO
mammograms, which is another important benefit
of using MammoPad. We recommend the use of
MammoPad for screening mammography in all our
patients.
Acknowledgements
The authors thank Betty ML Hung and Carmen
KM Lam for their assistance in preparation of the
questionnaires and data analysis.
References
1. Weedon-Fekjær H, Romundstad PR, Vatten LJ. Modern
mammography screening and breast cancer mortality:
population study. BMJ 2014;348:g3701. Crossref
2. Broeders M, Moss S, Nyström L, et al. The impact of
mammographic screening on breast cancer mortality in
Europe: a review of observational studies. J Med Screen
2012;19 Suppl 1:14-25. Crossref
3. Elwood M, McNoe B, Smith T, Bandaranayake M, Doyle
TC. Once is enough—why some women do not continue
to participate in a breast cancer screening programme. N Z
Med J 1998;111:180-3.
4. Shrestha S, Poulos A. The effect of verbal information
on the experience of discomfort in mammography.
Radiography 2001;7:271-7. Crossref
5. Lambertz CK, Johnson CJ, Montgomery PG, et al.
Premedication to reduce discomfort during screening
mammography. Radiology 2008;248:765-72. Crossref
6. Kornguth PJ, Rimer BK, Conaway MR, et al. Impact of
patient-controlled compression on the mammography
experience. Radiology 1993;186:99-102. Crossref
7. Tabar L, Lebovic GS, Hermann GD, Kaufman CS,
Alexander C, Sayre J. Clinical assessment of a radiolucent
cushion for mammography. Acta Radiol 2004;45:154-8. Crossref
8. Markle L, Roux S, Sayre JW. Reduction of discomfort
during mammography utilizing a radiolucent cushioning
pad. Breast J 2004;10:345-9. Crossref
9. Poulos A, Rickard M. Compression in mammography
and the perception of discomfort. Australas Radiol
1997;41:247-52. Crossref
10. Hong Kong Cancer Registry. Top ten cancers in 2013.
Available from: http://www3.ha.org.hk/cancereg/Statistics.html. Accessed Mar 2016.
11. Dibble SL, Israel J, Nussey B, Sayre JW, Brenner RJ, Sickles
EA. Mammography with breast cushions. Womens Health
Issues 2005;15:55-63. Crossref