Hong Kong Med J 2016 Apr;22(2):158–64 | Epub 20 Nov 2015
DOI: 10.12809/hkmj154549
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE
Evaluation of biological, psychosocial, and
interventional predictors for success of a smoking
cessation programme in Hong Kong
KS Ho, FHKAM (Family Medicine), FHKAM (Medicine);
Bandai WC Choi, MSocSc;
Helen CH Chan, MSocSc, MPH;
KW Ching, MB, BS, FHKAM (Family Medicine)
Integrated Centre for Smoking Cessation, Tung Wah Group of Hospitals;
(c/o) 17/F Tung Sun Commercial, 194-200 Lockhart Road, Wanchai, Hong
Kong
 Full
paper in PDF
Full
paper in PDF
Corresponding author: Dr KS Ho (rayhoks@yahoo.com.hk)
Abstract
Introduction: Predictors for smoking cessation have
been identified in different studies but some of the
predictors have been variable and inconsistent. In
this study, we reviewed all the potential variables
including medication, counselling, and others not
commonly studied to identify the robust predictors
of smoking cessation.
Methods: This historical cohort study was conducted in smoking cessation clinics in Hong Kong. Subjects who volunteered to come for free treatment between January 2010 and December 2011 were reviewed. Those under the age of 18 years, or who were mentally unstable or cognitively impaired were excluded. Counselling and quit-smoking medications were provided to the participants. The outcome measure was self-reported 7-day point prevalence abstinence rate at week 26.
Results: Univariate analysis showed that the
following were significant predictors of quitting:
(1) psychosocial variables such as feeling stressed,
feeling depressed, confidence in quitting, difficulty
in quitting, importance of quitting, Smoking Self-Efficacy Questionnaire score; (2) smoking-related variables
such as number of cigarettes smoked per day,
Fagerström Test for Nicotine Dependence score, number
of high-risk situations encountered; (3) health-related variable of having mental illness; (4) basic
demographics such as age, marital status, and
household income; and (5) interventional variables
such as counselling and pharmacotherapy. Multiple
logistic regression showed that the independent
predictors were age, having mental illness, daily
cigarette consumption, Fagerström Test for Nicotine Dependence score, reasons
for quitting, confidence in quitting, depressed mood,
external self-efficacy, intervention with counselling
and medications.
Conclusions: This clinic-based local study offers a
different perspective on the predictors of quitting.
It reminds us to adopt a holistic approach to deal
with nicotine withdrawal, to enhance external self-efficacy
to resist temptation and social influences, to
provide adequate counselling, and to help smokers
to cope with mood problems.
New knowledge added by this study
- A more holistic list of predictors of smoking cessation were included in this local clinic-based study, and differed from many other studies by population survey. Household income, marital status, gender, years of smoking, smoking cohabitant, perceived health, anxious mood, perceived importance, and difficulty in quitting were no longer predictors. Many of these are not modifiable. It is more important to enhance self-efficacy and to use counselling and medication to counter mood problems.
- In clinical practice, we should adopt a holistic approach to smoking cessation by providing more intensive counselling, managing withdrawal symptoms with medication, strengthening external self-efficacy to resist external temptation, and screening for mood problems.
Introduction
Smoking has long been identified as a major
global public health issue. It is the leading cause
of preventable death worldwide and kills about 6
million people each year.1 Although Hong Kong
has the lowest smoking prevalence among the
major cities of China, at 11.1% as reported in 2010,
it still accounts for about 5700 deaths annually,
approximately one fifth of all deaths per year. In 1998,
there were 1324 passive smoking–related deaths reported.2 3
According to the evidence-based MPOWER
measures introduced by the World Health
Organization4 to reduce the demand for tobacco,
to provide smoking cessation services and cessation
support in the public health care system, governments
around the world have put more emphasis on
smoking cessation programmes to reduce the
tobacco-related health risks.5 On 1 January 2007, the
Hong Kong Special Administrative Region (SAR)
Government enacted the Smoking (Public Health)
Ordinance and on 25 February 2009, tobacco tax was
increased by 50%. In 2009, the Tung Wah Group of
Hospitals (TWGHs) was commissioned by the Hong
Kong SAR Government to provide a community-based
smoking cessation service in Hong Kong.
The Integrated Centre on Smoking Cessation
(ICSC) of the TWGHs was set up in different
districts of Hong Kong, namely Shatin, Kwun Tong,
Sheung Shui, Tuen Mun, Mongkok, Wanchai,
Cheung Sha Wan, and Tsuen Wan to provide a
free smoking cessation service to Hong Kong
citizens. An integrated model of counselling and
pharmacotherapy was adopted.6 7
Identification of predictors and determinants
of success in smoking cessation is crucial for
smoking cessation service.8 Over the last decade,
health care professionals have endeavoured to identify
the predictors and characteristics of successful
quitters.9 Overseas studies have identified the
following: old age, high socio-economic status,10 11 12
male gender, younger age at smoking initiation,
previous quit attempts, being married, fewer
depressive symptoms, fewer anxiety symptoms,
lower prior tobacco consumption, lower score of
Fagerström Test for Nicotine Dependence (FTND),
no cohabitating smoker, and high cessation-related
motivation/confidence.8 10 11 12 13 14 Nonetheless, many studies have shown that these predictors are not
always consistent.11 15 This may be due to different methodologies and environments in different studies.
Some studies were population surveys based on
individual recall and did not include interventions.
In this study, we analysed all potential variables
and interventions. With a more comprehensive
list of variables, we hoped to identify some robust
independent predictors of successful quitters.
Methods
Study setting
Clients who attended an ICSC in different districts
in Hong Kong from 1 January 2010 to 31 December
2011 were recruited via smoking cessation hotlines,
referral from health care professionals, or self-referral.
All clients received counselling, and
pharmacotherapy was prescribed if the client agreed.
An average of four face-to-face counselling sessions
were conducted over the first 8-week intensive
treatment phase by registered social workers who
were all trained in tobacco cessation counselling.
Phone follow-up and counselling were also offered
during this treatment phase and between 9 and 12
weeks. The stage of change theory and motivational
interviewing techniques were adopted.16 17 18 Clients
were followed up by telephone at week 26 and
week 52 to ascertain abstinence from smoking. The
medications provided by ICSC included nicotine
replacement therapy (NRT) and non-NRT. The
former included nicotine patches, gum, lozenges,
and inhalers. Oral medications included varenicline
and bupropion. Medications were prescribed
according to the clients’ personal preference and
clinical conditions following a thorough explanation
by counsellors or medical officers. For example, NRT
gum would not be given to a client with dentures
and a patch would not be given to a client with skin
allergy.
Study design, participants, and data collection
This was a historical cohort study. All cases
commenced treatment between 1 January 2010 and
31 December 2011. The inclusion criteria of the
study were adults aged 18 years or above. Clients
who were mentally unstable or cognitively impaired
were excluded.
A structured questionnaire was used to collect
the following information: (i) socio-demographic
variables: age, gender, marital status, education,
monthly household income, number of people living
together; (ii) health-related variables: perceived
health, cessation advice by nurse, cessation advice by
doctor, cessation advice by any medical professional,
severe/chronic illness, mental illness; (iii) smoking-related
variables: age started smoking, years of
smoking, cohabitation with another smoker, number
of cigarettes smoked per day, FTND score,19 previous
quit attempt, number of previous quit attempts, time
of last attempt, reason to quit, high-risk situation;
(iv) psychosocial variables: self-perceived stress,
self-perceived depression, perceived importance,
difficulty and confidence in quitting (from a scale of
0-100), perceived source of social support, Smoking
Self-Efficacy Questionnaire (SEQ-12)20 21; and (v) intervention variables. Consent was obtained and
confidentiality was assured. The questionnaire was
self-administered and illiterate clients were given
help as appropriate. Completed forms were validated
by the counsellors.
Outcome measure
The outcome measure was self-reported 7-day point
prevalence abstinence rate at week 26. Clients who
were not able to be followed up or with an absent
response for smoking status were considered to have
not quitted.
Statistical analyses
Data management and analysis was performed
using the Statistical Package for the Social Sciences
(Windows version 22.0; SPSS Inc, Chicago [IL],
US). Univariate logistic regression was used for all
studied predictors. All predictors with a reported P
value of <0.10 were then included in multiple logistic
regression analysis. Backward elimination was used
in the multivariate analysis to identify independent
predictors of abstinence as well as to calculate the
adjusted odds ratio (AOR) and 95% confidence
interval. All statistical analyses were two-tailed tests
and a P value of <0.05 was considered statistically
significant.
Results
Demographics
A total of 4045 clients who attended the ICSC
during 1 January 2010 to 31 December 2011 were
reviewed and 3853 cases who met the inclusion
criteria were analysed. The gender ratio of male-to-female
was approximately 7:3. Their age ranged from 18
to 89 years with a mean of 42 years; mean duration
of smoking of this cohort was 20 years, and mean
cigarette consumption was 18 cigarettes per day
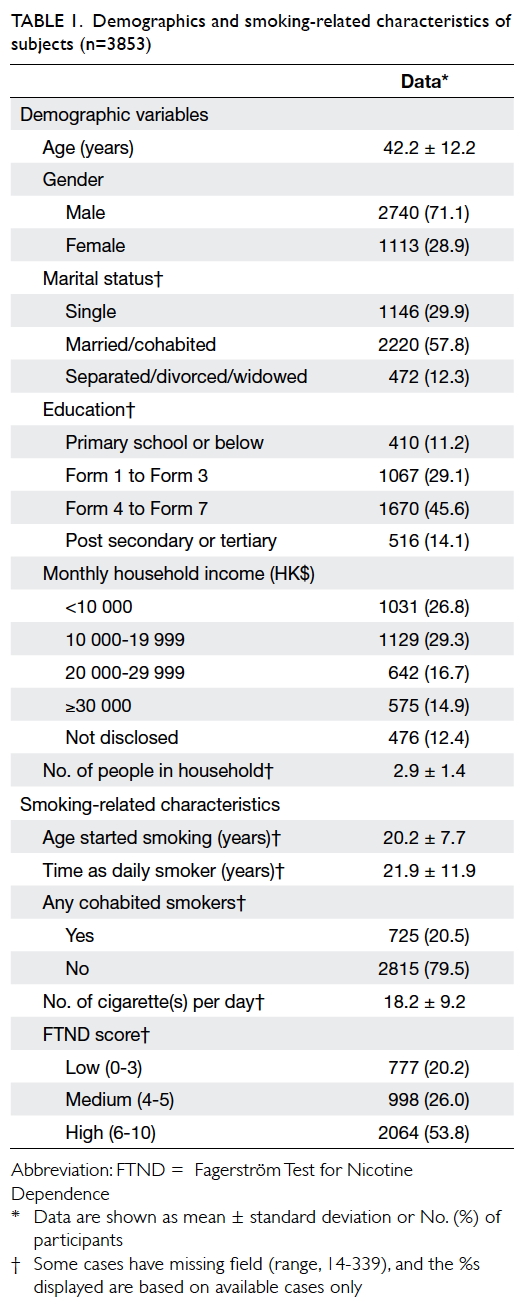
(Table 1).
Univariate logistic regression
The abstinence rate at week 26 was 35.1% (1353/3853).
Univariate analysis of basic demographic data
revealed that successful quitting was related to
older age, being married, and higher household
income (Table 2). Mental illness was significantly
related to failure to quit but chronic illness was not,
for examples, hypertension, diabetes, and chronic
obstructive pulmonary disease.
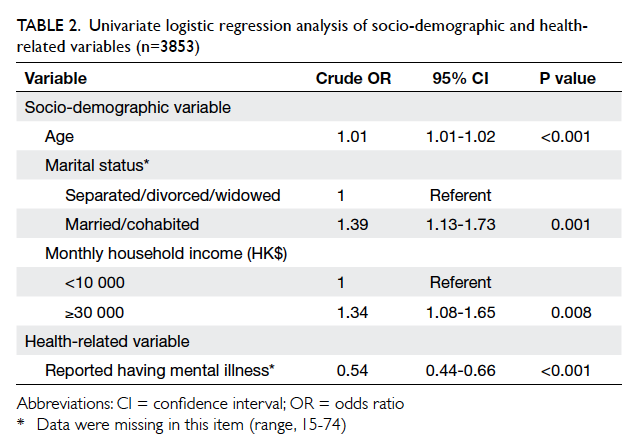
Table 2. Univariate logistic regression analysis of socio-demographic and health-related variables (n=3853)
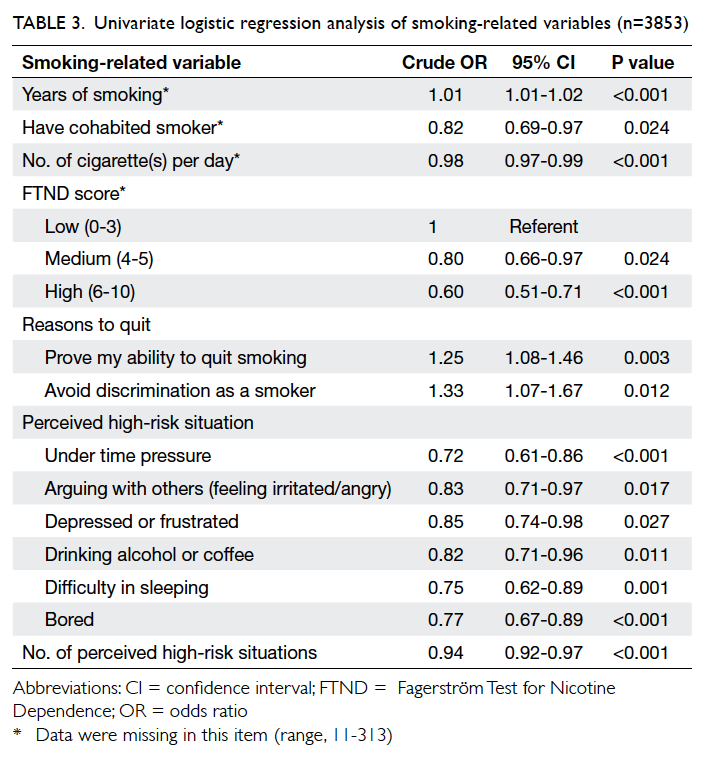
Analysis of smoking-related variables showed
that successful quitting was related to longer years
of smoking, not cohabiting with a smoker, lower
daily cigarette consumption, and lower FTND
score. Successful quitters were more likely to report
“prove my ability to quit smoking” and “avoid
discrimination as a smoker”. A higher number of
high-risk situations in quitting were negatively
related to quit rate. Significant individual high-risk
situations included “under time pressure”, “arguing
with others”, “depressed or frustrated”, “drinking
alcohol or coffee”, “difficulty in sleeping”, and “bored”
(Table 3).
The following psychosocial variables were
correlated to quitting: not feeling stressed, not feeling
depressed, high perceived importance of quitting,
low perceived difficulty in quitting, high confidence
in quitting, perceived support from spouse, and high
SEQ-12 score (Table 4). All interventional variables
were significant predictors of smoking abstinence:
number of face-to-face counselling sessions, over-the-phone counselling, and use of medication.
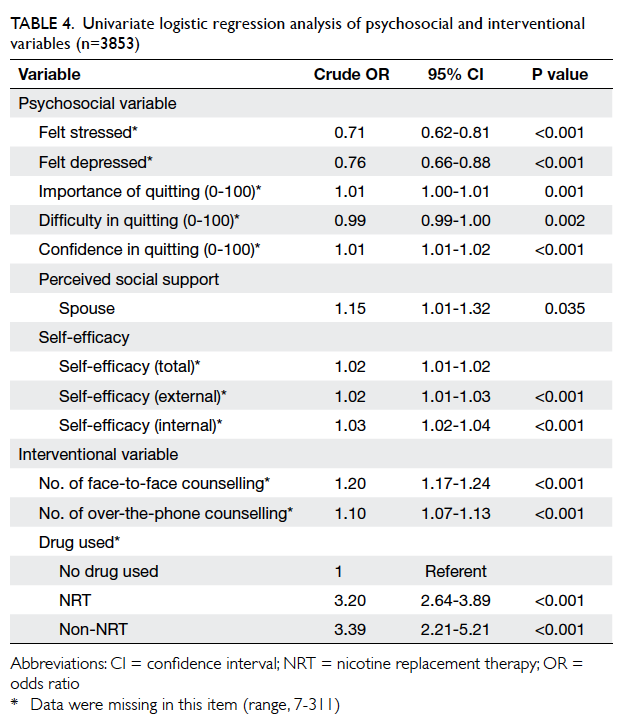
Table 4. Univariate logistic regression analysis of psychosocial and interventional variables (n=3853)
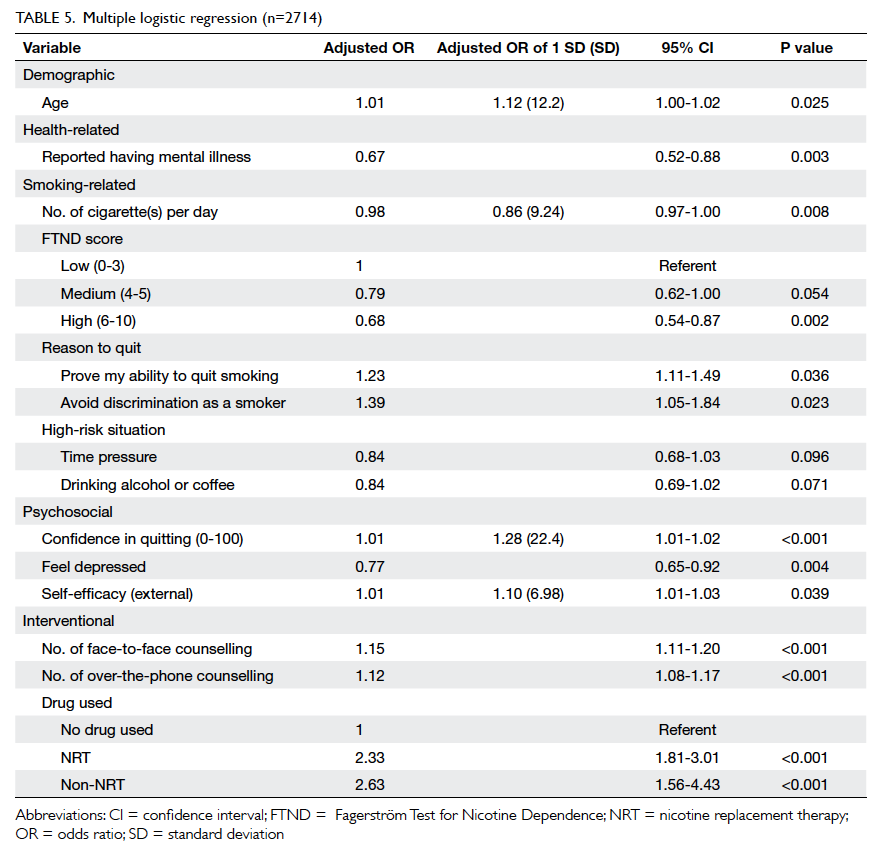
Multiple logistic regression
All items reported P<0.10 in the univariate logistic
regression analysis were included in the multiple
logistic model with backward elimination. Only
subjects with complete data in all fields of the
included items were analysed (n=2714). As shown
in Table 5, independent predictors of smoking
abstinence at week 26 were older age, quitting
based on “prove my ability to quit smoking”, high confidence in quitting,
high external self-efficacy, more counselling
sessions (both office and phone contact), and use
of medication. The following characteristics were
predictive of failure to quit: history of mental illness,
high daily cigarette consumption, high FTND score,
and feeling depressed.
Discussion
This is the first comprehensive study
of predictors of success for smoking cessation in a
local smoking cessation service. Age, mental health,
cigarette consumption, FTND score, reasons to quit,
confidence in quitting, depressive mood, self-efficacy,
sessions of office counselling, phone counselling, and
medication treatment were identified as predictors
among clients who volunteered to quit smoking.
In the univariate logistic analysis, most of the
predictors were consistent with other studies. In
many studies of predictors,15 22 results for gender, number of previous attempts, education level
and social status, years of smoking, and history of
depression have been inconsistent. In our study, a
more comprehensive list of potential predictors from
five domains (namely, demographics, health-related,
smoking-related, psychosocial, and interventional
variables) was included. After multiple logistic
regression analysis, many commonly reported
determinants/predictors were excluded. They
included perceived health, marital status,
cohabitation with a smoker, household income,
gender, years of smoking, perceived importance of
quitting or difficulty in quitting, feeling anxious, and
internal self-efficacy in quitting.
The effect of age appeared to be consistent
with the results of local23 24 and some international studies11 12 13 that older age was an independent predictor.25 Results for the predictive power of male gender have been controversial: some studies have
reported it as a predictor of cessation success,8 10 26 while others have found it to have no significant
effect or a negative effect.12 27 28 Our study could not confirm these findings. In addition, the role of marital
status, education, household income, and number of cohabitants were shown not to be predictive, contrary to some overseas studies.29 30 Nonetheless, consistent with many studies, cigarette consumption and FTND score were negatively correlated with quit rate.8 27 31
Extensive research indicates that individual
motivation, especially intrinsic motivation, is
predictive of the long-term cessation result.8 In
our study, two robust reasons to quit that could
significantly predict abstinence were “prove my
ability to quit smoking” and “avoid discrimination as
a smoker”. This seemed to correspond to the “self-control”
and “social influence” factors of Reasons for
Quitting scale.32 In Hong Kong, smoking in some
designated areas and public places is forbidden.
This may precipitate the “avoid discrimination as a
smoker” response. In service provision, operational
initiatives and promotion strategies may be tailored
to these two areas when motivating smokers to quit.
Perceived depressive mood (AOR=0.77)
and history of mental illness (AOR=0.67) greatly
enervated the success rate of quitting in our
participants. Similar results have been reported
in western countries as well as in Asia.8 33 34 35
This reinforces the importance of implementing
appropriate mental health screening and referral
in smoking cessation clinics. Presence of a chronic
illness was not shown to be predictive although this
may have been due to our relatively small sample size
for this group of clients or because ours was a cohort
of smokers who were motivated to quit. The effect
of chronic illness may thus be attenuated. Studies
have also shown that not all chronic diseases have
the same impact on smoking cessation.36 37
The link between self-efficacy and successful
quitting has long been established.22 38 Both external and internal self-efficacy in SEQ-12 scales have been found to be predictive in smoking cessation in western countries.21 In our study, after adjusting all potential
predictors, a high degree of confidence and external self-efficacy were predictive of cessation, while the
predictive ability of total and internal sub-score of SEQ-12 faded after adjustment. This is consistent
with a previous Hong Kong study.20 Manifestation of
cultural differences in self-efficacy during smoking cessation warranted further investigation. According
to the results in the current study, smoking cessation counselling should focus more on helping clients to
develop techniques to resist external temptation and to enhance external self-efficacy.
Consistent with overseas reviews of smoking
cessation counselling,15 39 our study indicated that the number of sessions of face-to-face counselling or phone support were strong predictors (AOR=1.15 and 1.12, respectively). Both kinds of medication (NRT and non-NRT) were also associated with successful smoking cessation. Most previous predictor studies have not included these parameters, however.
There are some limitations in our study. Since
this was a retrospective case review study of smokers
who were motivated to quit, the results cannot be
generalised to the whole smoking population. In
addition, in the process of multiple logistic regression,
only 2714 clients instead of all study subjects were
analysed. Interventional variables such as office
counselling, phone counselling, and medication
modality were not randomly allocated. Patient
compliance with medication was not evaluated,
thus information on the use of medication may be
biased. Another potential confounding factor was a
small amount of missing data for some predictors.
The effect of job nature and different chronic
illnesses was not included in this study because
of insufficient data; only chronic disease
as a group was analysed. Self-reported 7-day point
prevalence abstinence rate was not biochemically
validated although previous study has shown that
self-reported abstinence does not differ much to
abstinence according to biochemical validation.40
Conclusions
This local study has identified a number of predictors
of smoking abstinence at week 26 in clients who
volunteered to seek treatment from a smoking
cessation clinic. Most large-scale overseas studies
have been based on a population survey. This was
a large-scale comprehensive study performed in
a real-life smoking cessation programme in Hong
Kong. As such, it offers a better understanding of
the determinants of successful quitting. Although
some predictors have not been addressed and need
further study, this study highlights the need for a
holistic approach to the management of nicotine
withdrawal, and to enhance external self-efficacy
and motivation, to provide an adequate number of
counselling sessions and to help smokers cope with
mood problems.
References
1. WHO Report on the global tobacco epidemic. Geneva:
World Health Organization; 2013.
2. Lam TH, Ho SY, Hedley AJ, Mak KH, Peto R. Mortality
and smoking in Hong Kong: case-control study of all adult
deaths in 1998. BMJ 2001;323:361. Crossref
3. Hong Kong Council on Smoking and Health: Annual
Report 2011-2012. Hong Kong: Hong Kong Council on
Smoking and Health; 2012.
4. WHO Report on the global tobacco epidemic, 2008: The
MPOWER Package. Geneva: World Health Organization;
2008.
5. Wang L, Kong L, Wu F, Bai Y, Burton R. Preventing chronic
diseases in China. Lancet 2005;366:1821-4. Crossref
6. 2008 PHS Guideline Update Panel, Liaisons, and Staff.
Treating tobacco use and dependence: 2008 update U.S.
Public Health Service Clinical Practice Guideline executive
summary. Respir Care 2008;53:1217-22.
7. Reducing tobacco use: a report of the Surgeon General—executive summary. Nicotine Tob Res 2000;2:379-95. CrossRef
8. Caponnetto P, Polosa R. Common predictors of smoking
cessation in clinical practice. Respir Med 2008;102:1182-92. Crossref
9. Prochaska JO, DiClemente CC, Velicer WF, Ginpil S,
Norcross JC. Predicting change in smoking status for self-changers.
Addict Behav 1985;10:395-406. Crossref
10. Hymowitz N, Cummings KM, Hyland A, Lynn WR,
Pechacek TF, Hartwell TD. Predictors of smoking cessation
in a cohort of adult smokers followed for five years. Tob
Control 1997;6 Suppl 2:S57-62. Crossref
11. Monsó E, Campbell J, Tønnesen P, Gustavsson G, Morera
J. Sociodemographic predictors of success in smoking
intervention. Tob Control 2001;10:165-9. Crossref
12. Osler M, Prescott E. Psychosocial, behavioural, and
health determinants of successful smoking cessation: a longitudinal study of Danish adults. Tob Control
1998;7:262-7. Crossref
13. Hyland A, Borland R, Li Q, et al. Individual-level predictors
of cessation behaviours among participants in the
International Tobacco Control (ITC) Four Country Survey.
Tob Control 2006;15 Suppl 3:iii83-94. Crossref
14. Haas AL, Muñoz RF, Humfleet GL, Reus VI, Hall SM.
Influences of mood, depression history, and treatment
modality on outcomes in smoking cessation. J Consult Clin
Psychol 2004;72:563-70. Crossref
15. Iliceto P, Fino E, Pasquariello S, D’Angelo Di Paola ME,
Enea D. Predictors of success in smoking cessation among
Italian adults motivated to quit. J Subst Abuse Treat
2013;44:534-40. Crossref
16. Miller WR, Rollnick S. Talking oneself into change:
motivational interviewing, stages of change, and
therapeutic process. J Cogn Psychother 2004;18:299-308. Crossref
17. DiClemente CC, Prochaska JO. Toward a comprehensive,
transtheoretical model of change: stages of change and
addictive behaviors. In: Miller WR, Heather N, editors.
Treating addictive behaviors. 2nd ed. New York: Plenum
Press; 1998: 3-24.
18. Lai DT, Cahill K, Qin Y, Tang JL. Motivational interviewing
for smoking cessation. Cochrane Database Syst Rev
2010;(1):CD006936. Crossref
19. Heatherton TF, Kozlowski LT, Frecker RC, Fagerström KO.
The Fagerström Test for Nicotine Dependence: a revision
of the Fagerström Tolerance Questionnaire. Br J Addict
1991;86:1119-27. Crossref
20. Leung DY, Chan SS, Lau CP, Wong V, Lam TH. An evaluation
of the psychometric properties of the Smoking Self-Efficacy Questionnaire (SEQ-12) among Chinese cardiac
patients who smoke. Nicotine Tob Res 2008;10:1311-8. Crossref
21. Etter JF, Bergman MM, Humair JP, Perneger TV.
Development and validation of a scale measuring self-efficacy
of current and former smokers. Addiction
2000;95:901-13. Crossref
22. Li L, Borland R, Yong HH, et al. Predictors of smoking
cessation among adult smokers in Malaysia and Thailand:
findings from the International Tobacco Control Southeast
Asia Survey. Nicotine Tob Res 2010;12 Suppl:S34-44. Crossref
23. Yu DK, Wu KK, Abdullah AS, et al. Smoking cessation
among Hong Kong Chinese smokers attending hospital as
outpatients: impact of doctors’ advice, successful quitting
and intention to quit. Asia Pac J Public Health 2004;16:115-20. Crossref
24. Abdullah AS, Yam HK. Intention to quit smoking, attempts
to quit, and successful quitting among Hong Kong Chinese
smokers: population prevalence and predictors. Am J
Health Promot 2005;19:346-54. Crossref
25. Fiore MC, Novotny TE, Pierce JP, Hatziandreu EJ, Patel
KM, Davis RM. Trends in cigarette smoking in the United
States. The changing influence of gender and race. JAMA
1989;261:49-55. Crossref
26. Piper ME, Cook JW, Schlam TR, et al. Gender, race,
and education differences in abstinence rates among
participants in two randomized smoking cessation trials.
Nicotine Tob Res 2010;12:647-57. Crossref
27. Vangeli E, Stapleton J, Smit ES, Borland R, West R.
Predictors of attempts to stop smoking and their success
in adult general population samples: a systematic review.
Addiction 2011;106:2110-21. Crossref
28. Bjornson W, Rand C, Connett JE, et al. Gender differences
in smoking cessation after 3 years in the Lung Health Study.
Am J Public Health 1995;85:223-30. Crossref
29. Kim YJ. Predictors for successful smoking cessation in
Korean adults. Asian Nurs Res (Korean Soc Nurs Sci)
2014;8:1-7. Crossref
30. Chandola T, Head J, Bartley M. Socio-demographic
predictors of quitting smoking: how important are
household factors? Addiction 2004;99:770-7. Crossref
31. Abdullah AS, Ho LM, Kwan YH, Cheung WL, McGhee
SM, Chan WH. Promoting smoking cessation among the
elderly: what are the predictors of intention to quit and
successful quitting? J Aging Health 2006;18:552-64. Crossref
32. Curry S, Wagner EH, Grothaus LC. Intrinsic and extrinsic
motivation for smoking cessation. J Consult Clin Psychol
1990;58:310-6. Crossref
33. Kim SK, Park JH, Lee JJ, et al. Smoking in elderly Koreans:
prevalence and factors associated with smoking cessation.
Arch Gerontol Geriatr 2013;56:214-9. Crossref
34. Lasser K, Boyd JW, Woolhandler S, Himmelstein DU,
McCormick D, Bor DH. Smoking and mental illness: A
population-based prevalence study. JAMA 2000;284:2606-10. Crossref
35. Covey LS, Glassman AH, Stetner F. Depression and
depressive symptoms in smoking cessation. Compr
Psychiatry 1990;31:350-4. Crossref
36. Salive ME, Cornoni-Huntley J, LaCroix AZ, Ostfeld
AM, Wallace RB, Hennekens CH. Predictors of smoking
cessation and relapse in older adults. Am J Public Health
1992;82:1268-71. Crossref
37. Freund KM, D’Agostino RB, Belanger AJ, Kannel WB,
Stokes J 3rd. Predictors of smoking cessation: The
Framingham Study. Am J Epidemiol 1992;15:957-64.
38. Gwaltney CJ, Metrik J, Kahler CW, Shiffman S. Self-efficacy
and smoking cessation: a meta-analysis. Psychol
Addict Behav 2009;23:56-66. Crossref
39. Clinical Practice Guideline Treating Tobacco Use and
Dependence 2008 Update Panel, Liaisons, and Staff. A
clinical practice guideline for treating tobacco use and
dependence: 2008 update. A U.S. Public Health Service
report. Am J Prev Med 2008;35:158-76.
40. Patrick DL, Cheadle A, Thompson DC, Diehr P, Koepsell
T, Kinne S. The validity of self-reported smoking, a review
and meta-analysis. Am J Public Health 1994;84:1086-93. Crossref