Hong Kong Med J 2016 Apr;22(2):131–7 | Epub 12 Feb 2016
DOI: 10.12809/hkmj154595
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE
Participant evaluation of simulation training using crew resource management in a hospital setting in Hong Kong
Christina KW Chan, BSc, MPH1;
Eric HK So, FHKCA, FHKAM (Anaesthesiology)2;
George WY Ng, FHKCP, FHKAM (Medicine)3;
Teresa WL Ma, FRCOG, FHKAM (Obstetrics and Gynaecology)4;
Karen KL Chan, FHKCEM, FHKAM (Emergency Medicine)5;
LY Ho, FRCS (Urology), FHKAM (Surgery)1
1 Multidisciplinary Simulation and Skills Centre, Queen Elizabeth Hospital, Jordan, Hong Kong
2 Anaesthesiology and Operating Theatre Services, Queen Elizabeth Hospital, Jordan, Hong Kong
3 Intensive Care Unit, Queen Elizabeth Hospital, Jordan, Hong Kong
4 Department of Obstetrics and Gynaecology, Queen Elizabeth Hospital, Jordan, Hong Kong
5 Accident and Emergency Department, Queen Elizabeth Hospital, Jordan, Hong Kong
Corresponding author: Ms Christina KW Chan (mdssc_research@ha.org.hk)
Abstract
Introduction: A simulation team–based crew
resource management training programme was
developed to provide a unique multidisciplinary
learning experience for health care professionals in
a regional hospital in Hong Kong. In this study, we
evaluated how health care professionals perceive the
programme.
Methods: A cross-sectional questionnaire survey
was conducted in the Multidisciplinary Simulation
and Skills Centre at Queen Elizabeth Hospital in Hong
Kong. A total of 55 individuals in the departments of
Obstetrics and Gynaecology, Anaesthesiology and
Operating Theatre Services, Intensive Care Unit,
and Accident and Emergency participated in the study between
June 2013 and December 2013. The course content
was specially designed according to the needs of
the clinical departments and comprised a lecture
followed by scenarios and debriefing sessions.
Principles of crew resource management were
introduced and taught throughout the course by
trained instructors. Upon completion of each course,
the participants were surveyed using a 5-point Likert
scale and open-ended questions.
Results: The participant’s responses to the survey
were related to course organisation and satisfaction,
realism, debriefing, and relevance to practice.
The overall rating of the training programme was
high, with mean Likert scale scores of 4.1 to 4.3.
The key learning points were identified as closed-loop
communication skills, assertiveness, decision
making, and situational awareness.
Conclusions: The use of a crew resource
management simulation-based training programme
is a valuable teaching tool for frontline health care
staff. Concepts of crew resource management were
relevant to clinical practice. It is a highly rated
training programme and our results support its
broader application in Hong Kong.
New knowledge added by this study
- Our data support the use of crew resource management (CRM) in a simulation-based training programme as an effective means for teaching health care professionals in a public hospital setting in Hong Kong. Programmes may need to be customised for each specialty, however. Our results showed that this type of training is highly rated and accepted by frontline health care professionals.
- A key area for future improvement in health care providers is to teach and practise CRM. CRM has been recognised as an effective educational tool in health care organisations. Its broader application in Hong Kong should be encouraged.
Introduction
Simulation-based training is increasingly recognised
as a useful educational tool in health care
organisations.1 Within an acute care setting, these
tools are used for various training purposes, for
example, teaching technical2 and non-technical3 4
skills and rehearsing rare events.5 Simulation is
a technique “to replace or amplify real [patient]
experiences with guided experiences that evoke or
replicate substantial aspects of the real world in a
fully interactive manner”.6 With the application of
adult learning theory,7 simulation-based training
is usually designed to resemble the reality and
allows trainees to acquire knowledge, skills, and
competence in a safe and controlled environment.8 9
Studies have shown that teamwork plays an
important role in the prevention of adverse events
and errors.10 11 Simulation-based training programmes
that focus on crew resource management (CRM)
criteria have been found to effectively improve
teamwork skills. Such criteria emphasise teaching
of non-technical skills, such as communication,
leadership, assertiveness, and situational awareness,
thereby improving patient safety.12 13
Crew resource management is a risk-reduction
programme of the Hospital Authority (HA) in Hong
Kong and has run since 2009. Between 2009 and
2012, Pamela Youde Nethersole Eastern Hospital
piloted the classroom-based CRM programme
to approximately 2000 staff in the hospital.14 The
programme received positive feedback from staff
and the impact on patient safety was evident in the
programme evaluation. Thus, the HA decided that
a second-phase roll-out of CRM was necessary
because there was a need for team-based training.
Queen Elizabeth Hospital (QEH) and Tuen Mun
Hospital were the two public hospitals selected to
implement the second pilot programme of the CRM
focusing on specialty-based simulation training.
The Multidisciplinary Simulation and
Skills Centre (MDSSC) at QEH has developed a
simulation team–based CRM training programme.
This new training programme provides a unique
multidisciplinary learning experience for health
care professionals at QEH. The MDSSC used this
opportunity to evaluate how health care professionals
perceive the programme.
Methods
The train-the-trainer workshop
In order to roll out the second phase of the CRM
programme to QEH, HA engaged Safer Healthcare15
to advise on the development and delivery of CRM
training courses. A 3-day on-site CRM train-the-trainer
workshop was held at MDSSC between
March and April 2013. The workshop was intended
for doctors and nurses working at QEH who were
interested in teaching medical education and would
like to become a CRM-certified trainer. All workshops
were taught by experienced instructors from Safer
Healthcare.15 The content of the workshops included
reviewing the use of CRM in health care, delivering
the CRM principles, enhancing presentation skills,
and handling difficulties and challenges in team
debriefing. All trainees had the unique opportunity
to develop scenarios using CRM principles. A total
of 40 doctors and nurses were trained and certified
to teach CRM courses.
Curriculum design
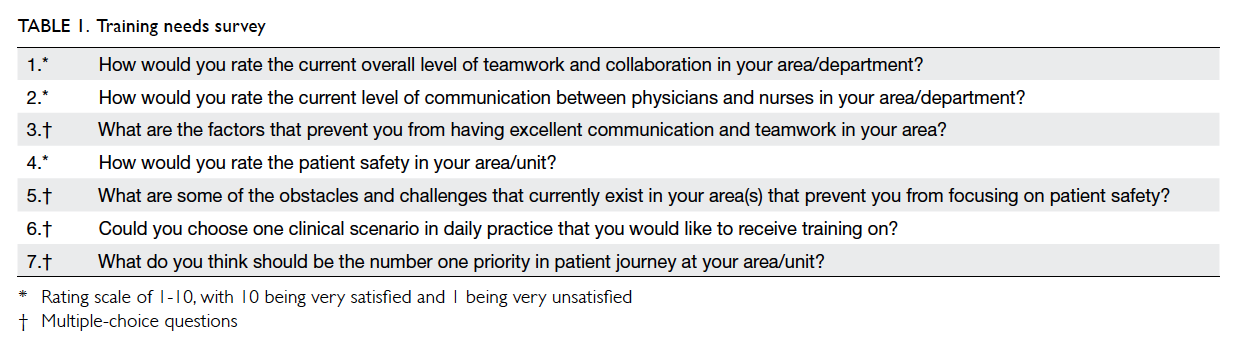
In order to determine the components of CRM
training most appropriate for frontline health
care staff, a survey was conducted of all frontline
health care staff in four selected high-risk areas
where teamwork is essential for satisfactory patient
outcome: Obstetrics and Gynaecology (O&G),
Anaesthesiology and Operating Theatre Services
(Anaes & OTS), Intensive Care Unit (ICU), and
Accident and Emergency (A&E). The survey was
designed to assess staff perception of teamwork and
patient safety, obstacles, and challenges encountered
in the workplace, and areas where training was
wanted. Some of the questions were based on the most
common reasons why medical errors occur among
the four specialties as well as from the literature.16 17 18 The survey consisted of seven multiple-choice and
rating-scale questions about teamwork, patient
safety, the obstacles and challenges in practice, and
training needs (Table 1).
The CRM curriculum for the four specialties
was first proposed by the course coordinators who
were the specialist consultants and associate consultants
from respective departments at QEH. The
course coordinators first identified their staffing needs
based on the results of the survey. They developed a
specialty-based training programme that addressed
their frontline staff learning needs and was related
to the type of sentinel and serious untoward events
reported. This would enable participants to learn
non-technical CRM skills and apply them in their
workplace when making clinical judgements and
performing procedures. The specialty-based training
programme comprised three components: a lecture,
games, and scenarios. Each scenario was customised
for each specialty in order to fulfil its learning
objectives, specific educational outcomes, and needs
of the department in order to enhance participants’
learning experience. All scenario practice sessions
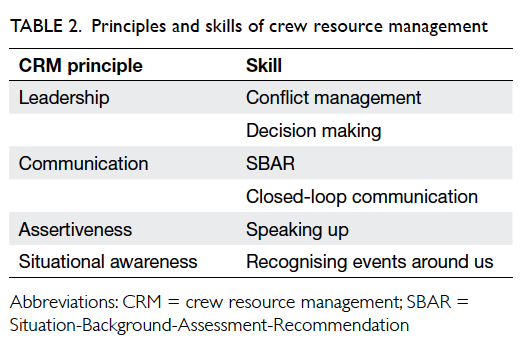
included CRM principles as defined in Table 2 and were chosen according to the needs at QEH.
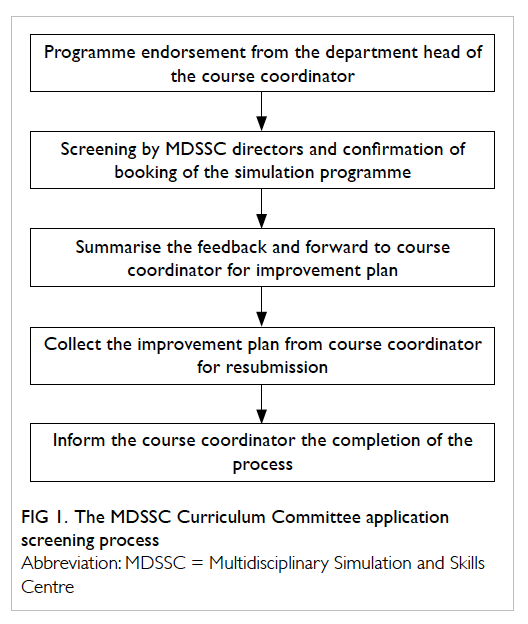
After the programmes had been endorsed
by the department head, the directors of MDSSC
reviewed and evaluated the programme. Feedback
and recommendations were given to course
coordinators so they could improve the quality of
the training, and ensure CRM components were
included and that the course supported the MDSSC’s
mission statement. The course coordinators made
changes according to the reviewers’ comments.
A confirmation of the booking date was given to
the course coordinators once the programme had
been endorsed by the reviewers. The evaluation of
a programme required approximately 2 weeks to
complete (Fig 1).
The training programme
The CRM training programme took place between
June and December 2013. The training began with
a lecture introducing the background of CRM. A
game was played afterwards and served as an ‘icebreaker’
and illustrated the importance of teamwork,
leadership, and decision making.
Next, simulation training was conducted with
two scenarios followed by a debriefing session.
Each scenario was performed by a group of four
to five health care frontline staff. Members of each
group participated in the debriefing after each
simulation scenario. The role of the trainer was to
lead a discussion about team strengths and areas for
improvement. This allowed participants to reflect on
their experience related to CRM skills and clinical
knowledge in the scenarios. Participants may also
have learnt new concepts and techniques that could
be applied in daily practice. All training was given
at MDSSC and conducted by experienced certified
CRM trainers.
Sample
Participants were recruited from four high-risk
departments at QEH through nominations based
on their availability. The study sample included
doctors and nurses working in the frontline area
of these four departments: O&G, Anaes & OTS,
ICU, and A&E. Each participant was assigned a
specific role during each scenario. The role could
be changed for different simulation scenarios. All
participants received the same educational content
and simulation opportunities.
Data collection
Participants evaluated the CRM simulation training
by anonymous completion of a questionnaire
that comprised six open-ended questions and 14
questions that were answered on a 5-point Likert
scale (1 = strongly disagree, 2 = disagree, 3 =
neutral, 4 = agree, 5 = strongly agree). Open-ended
questions focused on the areas of learning needs,
the specific areas where CRM can be implemented,
the learning points that were applicable to practice,
and recommendation of the programme to other
colleagues. The first section aimed to obtain
information about the training programme. The
open-ended questions were asked to elicit qualitative
responses related to learning and demographic
information. The evaluation was paper-based and
completed by participants at the end of the training
programme.
Statistical analysis
The data were tabulated using Microsoft Excel
and analysed using the STATA 13. Demographic
information of participants was reported as
frequency (%) and participant scores were reported
as mean ± standard deviation.
Results
Training needs analysis
A total of 380 frontline health care staff were invited
to participate in the training needs survey that was
completed by 319 (84%). The mean satisfaction rating
on a scale of 1 to 10 for overall level of teamwork and
collaboration, the current level of communication
between physicians and nurses, and patient safety on
their unit was 6.5, 6.2, and 7.1, respectively. Factors
that prevented frontline health care staff from
achieving excellent communication and teamwork
included different types of personality among
colleagues (n=92, 29%), too many things to attend to
at the same time (n=85, 27%), a culture that prevented
an individual from speaking out (n=73, 23%), lack of
a standard communication format (n=39, 12%), and
fear of being wrong (n=30, 9%). The obstacles and
challenges that prevented them from focusing on
patient safety included inadequate manpower (n=85,
27%), heavy workload (n=80, 25%), time pressure
(n=77, 24%), poor team communication (n=51, 16%),
and insufficient equipment (n=26, 8%). The top five
areas in which staff would like to receive training were
handling a difficult patient (n=118, 37%), handover
of critical cases (n=85, 27%), briefing and debriefing
(n=48, 15%), collapse in the operating theatre/ward
(n=42, 13%), and difficult airway (n=26, 8%). Good
leadership and decision making was considered by
86 (27%) of staff to be the top priority in patient care,
followed by good clinical skill and knowledge (n=78,
24%), good team communication (n=69, 22%),
more manpower (n=57, 18%), and better clinical
environment (n=29, 9%) [Fig 2].
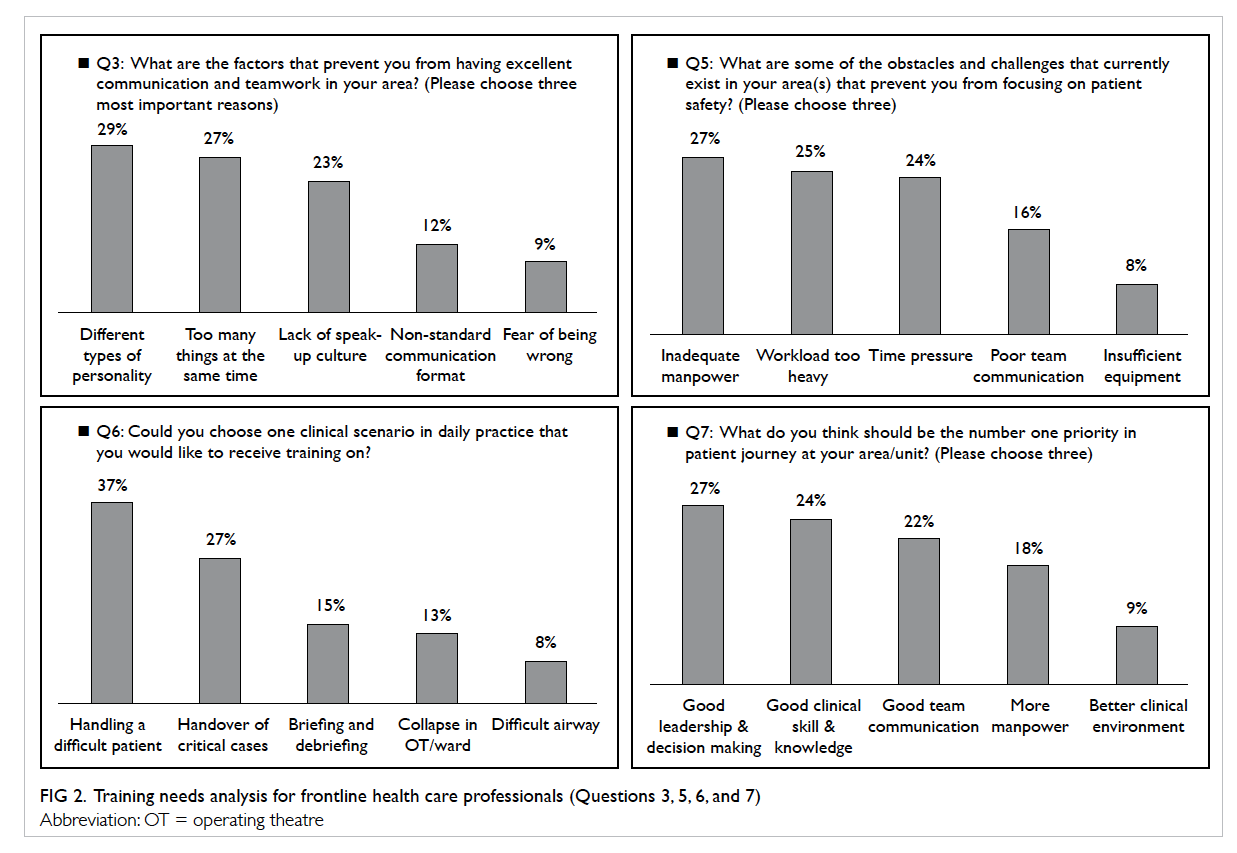
Figure 2. Training needs analysis for frontline health care professionals (Questions 3, 5, 6, and 7)
The training programme
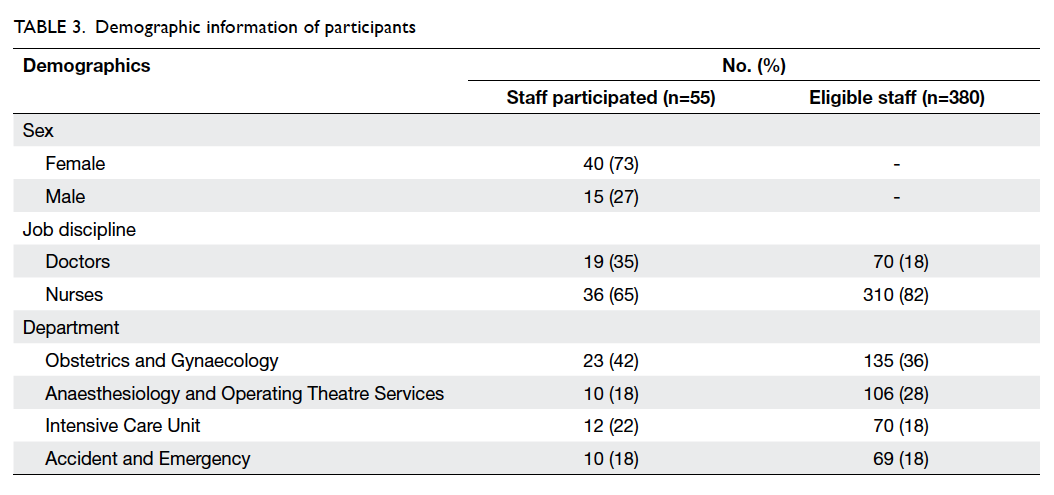
The number of frontline health care staff eligible for
the study in the O&G, Anaes & OTS, ICU, and A&E
departments was 135, 106, 70, and 69, respectively.
Among them, 55 (of whom 40 were female and
36 were nurses) were nominated to participate in
the study and completed the simulation training
programme. They included 23 participants from
O&G, 10 from Anaes & OTS, 12 from ICU, and 10
from A&E. The characteristics of these participants
are summarised in Table 3.
Likert-scale questions
Participant responses to the Likert-scale questions
were very positive, with mean scores of 4.1 to 4.3.
Almost all participants responded positively with
either ‘strongly agree’ or ‘agree’ to questions about
overall satisfaction with the training programme, the
applicability of the programme to area of practice,
and high standard and expertise of the trainers.
The question that received the lowest mean rating
was related to the ability of scenarios to facilitate
decision making. Nonetheless this question was still
considered ‘agree’ on a scale of 1 (strongly disagree)
to 5 (strongly agree). None of the questions were
rated ‘disagree’ or ‘strongly disagree’. Participant
ratings for all 14 questions are summarised in Table 4.
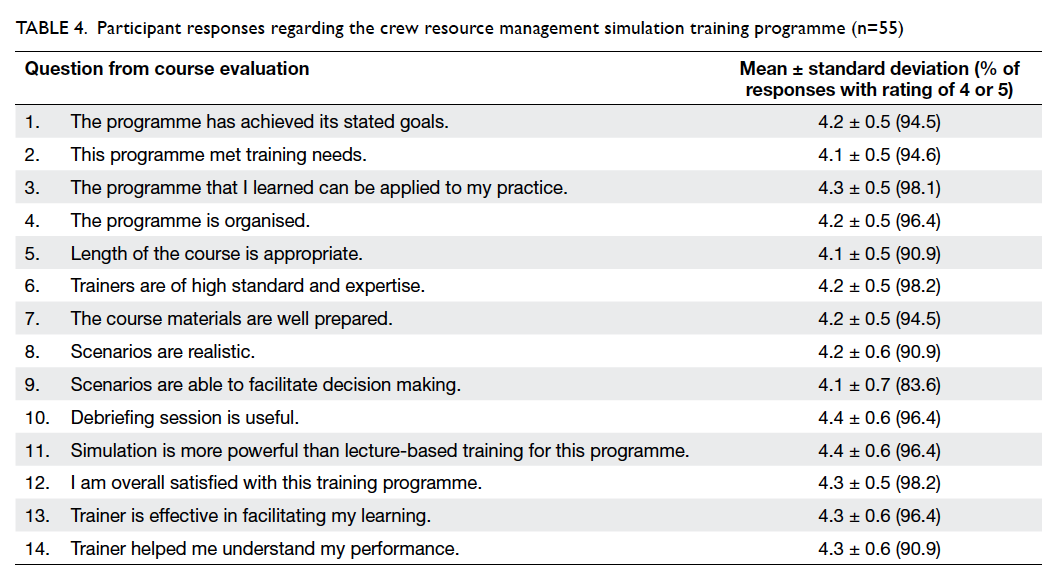
Table 4. Participant responses regarding the crew resource management simulation training programme (n=55)
Open-ended questions
For the open-ended questions, 85% (47/55) of
participants stated that they would recommend the
programme to other colleagues and 15% did not
respond to this question. Of the 55 participants, 11
commented on learning more about closed-loop
communication, situational awareness, assertiveness,
conflict resolution, decision making, and leadership.
Six participants commented positively on the
course itself. Specifically, comments were related to CRM
elements: “the CRM training is very useful to our
clinical work and even to our daily life” and “the
CRM videos are funny and useful”. The remaining
comments were “good”, “a pleasant experience”, and
“the programme was useful”.
When asked to list the learning points applicable
to work, participants most commonly responded
to the CRM elements, such as communication skills,
assertiveness, decision making, and situational
awareness.
Discussion
Training in non-technical skills is essential for health
care professionals to enhance patient safety and
teamwork.19 Hospital patients are normally treated
by a team having various disciplines; therefore, team
training is important to prevent human error.
High realism simulation is becoming widely
used in health care education.20 21 22 23 It creates a realistic
risk-free environment for learners to practise and
improve confidence in life-saving skills.
In our study, frontline health care staff
surveyed at MDSSC reacted positively to their initial
experience with CRM training, suggesting that this is
a favourable means by which to provide simulation-based
training. Almost all participants (91%-98%)
rated their level of agreement as high or very high for
overall course organisation, course content, trainer
performance, programme satisfaction, training
needs, and the usefulness of debriefing session.
These findings indicate that simulation-based CRM
training was well accepted by frontline health care
staff and they would likely benefit from simulation-based
scenarios, and is consistent with a previous
study.24
A number of participants stated that they would
recommend the programme to other colleagues.
Participants made very positive comments about
the CRM simulation-based training programme
and perceived CRM as an important means to
improve their teamwork skills. Although CRM can
be taught in a didactic approach, we believe that a
simulation approach has the advantage of motivating
participants to learn about teamwork skills and to
alter their behaviour, so reducing the risk of adverse
events. This type of training will help health care
professionals incorporate the CRM principles into
their daily practice.
To our knowledge, this is the first study to
specifically address the use of CRM in a tailor-made
specialty-based simulation training programme in
multiple clinical departments in a public hospital
in Hong Kong. Prior to this study, we distributed a
training needs survey to all frontline staff among the
four specialties that asked about their perception
of teamwork and learning needs. The results from
this survey provided a clear idea about the design
of scenarios. The topics and content were also
appropriate and could contribute to the development
of teamwork in a health care organisation. In terms
of teaching quality, all instructors were certified and
had completed the same CRM train-the-trainer
programme, thus teaching methods were consistent.
There are several limitations to this study.
First, it was undertaken in a single hospital
and analysed a simulation-based CRM training
programme specifically designed for each specialty.
Its generalisation to other CRM simulation-based
programmes in other multidisciplinary settings
may be limited. Second, the sample size was small.
Nonetheless this pilot study was designed to
determine staff perception of learning CRM rather
than to demonstrate efficacy. Furthermore, the
participants were recruited through nomination.
It is unclear whether those who were nominated
to participate may differ to those who were not
nominated (in terms of their characteristics). The
results may reflect a possible selection bias as
participants may be more inclined to participate
and learn from such a training programme. Other
limitations include the training needs survey that
was a self-report, not an objective assessment, and
was limited to the categories included in the survey.
The optional “other” response was rarely used by the
participants, however. Finally, although the survey
demonstrated a high level of acceptance of and
satisfaction with simulation-based CRM training,
this does not necessarily translate into improved
frontline health care performance. Further research
in this area is needed.
Conclusions
We have developed and rolled out a specialty-based
simulation CRM training programme in a
public hospital setting in Hong Kong. Our findings
demonstrate that CRM appeared to be highly valued
by participants and was applicable to their daily
practice. It also demonstrated that training needs
analysis may be useful to develop the content of a
simulation CRM training programme. The culture
of patient safety needs time to change however, and
this programme is just the first step in developing a
safety culture in health care organisations.
Acknowledgements
The MDSSC team would like to express its gratitude
to HA Head Office for their support and contribution
in this study. Without their support, the study could
not have been completed.
References
1. Cook DA, Hatala R, Brydges R, et al. Technology-enhanced
simulation for health professions education: a systematic
review and meta-analysis. JAMA 2011;306:978-88. Crossref
2. Boet S, Bould MD, Schaeffer R, et al. Learning fibreoptic
intubation with a virtual computer program transfers to
‘hands on’ improvement. Eur J Anaesthesiol 2010;27:31-5. Crossref
3. Yee B, Naik VN, Joo HS, et al. Nontechnical skills in
anesthesia crisis management with repeated exposure to
simulation-based education. Anesthesiology 2005;103:241-8. Crossref
4. Kneebone R, Nestel D, Wetzel C, et al. The human face of
simulation: patient-focused simulation training. Acad Med
2006;81:919-24. Crossref
5. Decarlo D, Collingridge DS, Grant C, Ventre KM. Factors
influencing nurses’ attitudes toward simulation-based
education. Simul Healthc 2008;3:90-6. Crossref
6. Gaba DM. The future vision of simulation in healthcare.
Simul Healthc 2007;2:126-35. Crossref
7. Speck M. Best practice in professional development for
sustained educational change. ERS Spectr 1996;14:33-41.
8. Kneebone RL, Scott W, Darzi A, Horrocks M. Simulation
and clinical practice: strengthening the relationship. Med
Educ 2004;38:1095-102. Crossref
9. Ziv A, Wolpe PR, Small SD, Glick S. Simulation-based
medical education: an ethical imperative. Simul Healthc
2006;1:252-6. Crossref
10. Manser T. Teamwork and patient safety in dynamic
domains of healthcare: a review of the literature. Acta
Anaesthesiol Scand 2009;53:143-51. Crossref
11. Künzle B, Kolbe M, Grote G. Ensuring patient safety
through effective leadership behaviour: a literature review.
Saf Sci 2010;48:1-17. Crossref
12. Kosnik LK. The new paradigm of crew resource
management: just what is needed to re-engage the
stalled collaborative movement? Jt Comm J Qual Improv
2002;28:235-41.
13. Risser DT, Rice MM, Salisbury ML, Simon R, Jay GD,
Berns SD. The potential for improved teamwork to
reduce medical errors in the emergency department.
The MedTeams Research Consortium. Ann Emerg Med
1999;34:373-83. Crossref
14. Hospital Authority Quality and Risk Management. Annual
Report (2012-2013). Hong Kong: Hospital Authority; 2013:
10-1.
15. Marshall DA, Manus DA. A team training program
using human factors to enhance patient safety. AORN J
2007;86:994-1011. Crossref
16. O’Daniel M, Rosenstein AH. Professional communication
and team collaboration. In: Hughes RG, editor. Patient
safety and quality: an evidence-based handbook for nurses.
Rockville (MD): Agency for Healthcare Research and
Quality (US); 2008.
17. Leonard M, Graham S, Bonacum D. The human factor:
the critical importance of effective teamwork and
communication in providing safe care. Qual Saf Health
Care 2004;13 Suppl 1:i85-90. Crossref
18. Manojlovich M, Antonakos CL, Ronis DL. Intensive care
units, communication between nurses and physicians, and
patients’ outcomes. Am J Crit Care 2009;18:21-30. Crossref
19. Gordon M, Darbyshire D, Baker P. Non-technical skills
training to enhance patient safety: a systematic review.
Med Educ 2012;46:1042-54. Crossref
20. Bruppacher HR, Alam SK, LeBlanc VR, et al. Simulation-based
training improves physicians’ performance in patient
care in high-stakes clinical setting of cardiac surgery.
Anesthesiology 2010;112:985-92. Crossref
21. Burkhart HM, Riley JB, Hendrickson SE, et al. The
successful application of simulation-based training in
thoracic surgery residency. J Thorac Cardiovasc Surg
2010;139:707-12. Crossref
22. Sexton JB, Makary MA, Tersigni AR, et al. Teamwork
in the operating room: frontline perspectives among
hospitals and operating room personnel. Anesthesiology
2006;105:877-84. Crossref
23. Seymour NE, Gallagher AG, Roman SA, et al. Virtual
reality training improves operating room performance:
results of a randomized, double-blinded study. Ann Surg
2002;236:458-63; discussion 63-4. Crossref
24. Blum RH, Raemer DB, Carroll JS, Sunder N, Felstein
DM, Cooper JB. Crisis resource management training
for an anaesthesia faculty: a new approach to continuing
education. Med Educ 2004;38:45-55. Crossref