Hong Kong Med J 2016 Apr;22(2):124–30 | Epub 11 Mar 2016
DOI: 10.12809/hkmj154706
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE CME
Mushroom poisoning in Hong Kong: a ten-year review
CK Chan, Dip Clin Tox (HKPIC & HKCEM), FHKAM (Emergency Medicine)1;
HC Lam, Dip Clin Tox (HKPIC & HKCEM), FHKAM (Emergency Medicine)1;
SW Chiu, MPhil (Biology), PhD2;
ML Tse, FHKCEM, FHKAM (Emergency Medicine)1;
FL Lau, FRCSEd, FHKAM (Emergency Medicine)1
1 Hong Kong Poison Information Centre, United Christian Hospital, Kwun
Tong, Hong Kong
2 School of Life Sciences, The Chinese University of Hong Kong, Shatin,
Hong Kong
Corresponding author: Dr CK Chan (chanck3@ha.org.hk)
Abstract
Introduction: Mushroom poisoning is a cause of
major mortality and morbidity all over the world.
Although Hong Kong people consume a lot of
mushrooms, there are only a few clinical studies and
reviews of local mushroom poisoning. This study
aimed to review the clinical characteristics, source,
and outcome of mushroom poisoning incidences in
Hong Kong.
Methods: This descriptive case series review was
conducted by the Hong Kong Poison Information
Centre and involved all cases of mushroom poisoning
reported to the Centre from 1 July 2005 to 30 June
2015.
Results: Overall, 67 cases of mushroom poisoning
were reported. Of these, 60 (90%) cases presented
with gastrointestinal symptoms of vomiting,
diarrhoea, and abdominal pain. Gastrointestinal
symptoms were early onset (<6 hours post-ingestion)
and not severe in 53 patients and all recovered after
symptomatic treatment and a short duration of
hospital care. Gastrointestinal symptoms, however,
were of late onset (≥6 hours post-ingestion) in
seven patients; these were life-threatening cases
of amatoxin poisoning. In all cases, the poisonous
mushroom had been picked from the wild. Three
cases were imported from other countries, and four
collected and consumed the amatoxin-containing
mushrooms in Hong Kong. Of the seven cases of
amatoxin poisoning, six were critically ill, of whom
one died and two required liver transplantation.
There was one confirmed case of hallucinogenic
mushroom poisoning caused by Tylopilus nigerrimus
after consumption of a commercial mushroom
product. A number of poisoning incidences involved
the consumption of wild-harvested dried porcini
purchased in the market.
Conclusion: Most cases of mushroom poisoning in
Hong Kong presented with gastrointestinal symptoms
and followed a benign course. Life-threatening
cases of amatoxin poisoning are occasionally seen.
Doctors should consider this diagnosis in patients
who present with gastrointestinal symptoms that
begin 6 hours or more after mushroom consumption.
New knowledge added by this study
- Local epidemiology data of mushroom poisoning presented between 1 July 2005 and 30 June 2015 that include the first case series of amatoxin poisoning in Hong Kong.
- Life-threatening amatoxin poisoning was caused by consumption of Amanita farinosa. This is the first report of this Amanita species in Hong Kong.
- A confirmed case of hallucinogenic mushroom poisoning was caused by imported Tylopilus nigerrimus.
- Public awareness of the high-risk behaviour of consuming self-picked wild mushrooms should be raised.
- A number of poisoning incidents involved the consumption of wild-harvested dried porcini purchased in the market.
- Doctors should suspect amatoxin poisoning in patients who present with gastrointestinal symptoms that begin 6 hours or more after wild mushroom consumption. Hong Kong Poison Information Centre can be consulted early to facilitate urgent mushroom identification and antidote treatment.
Introduction
Mushroom poisoning is a global phenomenon and
can be a source of major mortality and morbidity.
Although Hong Kong people consume a large volume
of mushrooms, there are few clinical studies and
reviews related to local mushroom poisoning.1 2 The
diagnosis of mushroom poisoning should be based
on clinical features, laboratory investigations, and
mushroom identification. Due to the lack of leftover
mushroom samples in most cases, emergency
physicians and clinical toxicologists usually have
to diagnose mushroom poisoning based on clinical
syndromes alone without mushroom identification
by mycologists. Diaz3 has reviewed and established
the classification of mushroom poisoning based on
the time of presentation and target organ systemic
toxicity. With respect to the time of presentation,
mushroom poisoning is categorised as early onset
(<6 hours), late onset (6-24 hours), or delayed onset
(>1 day). Early-onset toxicities include several
neurotoxic, gastrointestinal, and allergic syndromes.
Late-onset toxicities include hepatotoxic,
accelerated nephrotoxic, and erythromelalgia
syndromes. Delayed-onset toxicities include delayed
nephrotoxic, delayed neurotoxic and rhabdomyolytic
syndromes. Syndromic approaches guide earlier
diagnosis and facilitate empirical treatment.3
In Hong Kong, scattered cases of mushroom
poisoning are reported every year. In a report
published by the Centre for Health Protection (CHP),
there were 13 reported cases of wild mushroom
poisoning between January 2002 and May 2005.1
Symptoms occurred 0.5 to 5 hours post-ingestion and
included vomiting (100%), abdominal pain (100%),
diarrhoea (69%), nausea (56%), dizziness (50%),
sweating (37%), numbness (31%), palpitation (19%),
malaise (13%), fever (13%), and headache (6%).2 Of
these patients, seven required hospitalisation and
all of them completely recovered. Individual cases
of mushroom poisoning have been announced in
CHP press releases from time to time. In another
report, seven patients presented with mainly
gastrointestinal symptoms after wild mushroom
consumption between May 2007 and August 2010.2
There have been no reports of life-threatening wild
mushroom poisoning in Hong Kong before this case
series.
Since its establishment in 2005, the Hong
Kong Poison Information Centre (HKPIC) has
provided a 24-hour telephone consultation service
to health care professionals in Hong Kong for poison
information and clinical management advice. We are
actively involved in the diagnosis and management
of mushroom poisoning cases in local hospitals.
Supported by Prof SW Chiu from the School of Life
Sciences of The Chinese University of Hong Kong,
mycological identification can be provided whenever
mushroom samples are available in a poisoning
case. The objectives of this study were to review the
clinical features and mycological identifications in
mushroom poisoning cases recorded by the HKPIC.
Methods
Mushroom poisoning cases recorded by HKPIC
from 1 July 2005 to 30 June 2015 were retrospectively reviewed. Information on patient demographic
details, clinical presentation, sources of mushroom,
investigation results, mycological identification
results, and clinical outcome were obtained.
Descriptive statistics were used for data analysis.
Results
During the 10-year study period, there were 67 cases
of mushroom poisoning. All cases were reported
from hospitals of the Hospital Authority. All patients
were Chinese; 29 (43%) were male and 38 (57%) were
female. The median age was 47 (range, 2-86) years.
Of the 67 cases, 52 (78%) occurred between April and
September when the climate in Hong Kong is optimal
for mushroom growth. In 66 cases, the mushrooms
were intentionally consumed as delicacies. There
was one case of accidental ingestion, in which a
2-year-old boy ingested a wild mushroom in a park.
Ingestion with recreational, suicidal, or malicious
intent was not recorded in this case series.
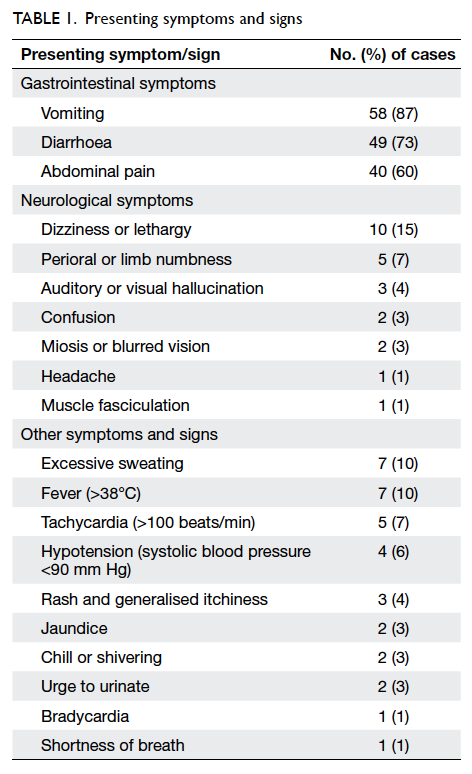
The most common clinical presentation was
gastrointestinal symptoms (Table 1). Symptoms mimicking gastroenteritis were the presenting
feature in 60 (90%) patients. The diagnosis of
these 60 patients included gastroenteritic mushroom
poisoning in 38, cholinergic mushroom poisoning in
five, food poisoning in eight, food allergy in two, and
seven cases of amatoxin poisoning.
Neurological symptoms were also commonly
reported: 20 (30%) patients presented with one or more symptoms
including dizziness, numbness, hallucination,
headache, or confusion (Table 1). Most of them (15
of 20 patients) presented with both neurological and
gastrointestinal symptoms. Four patients presented
with neurological symptoms including visual
hallucinations, dizziness, generalised weakness, and
malaise without gastrointestinal symptoms. They
were subsequently diagnosed with hallucinogenic
mushroom poisoning. One patient presented with
malaise, muscle fasciculation, and profuse sweating
that was diagnosed as cholinergic mushroom
poisoning.
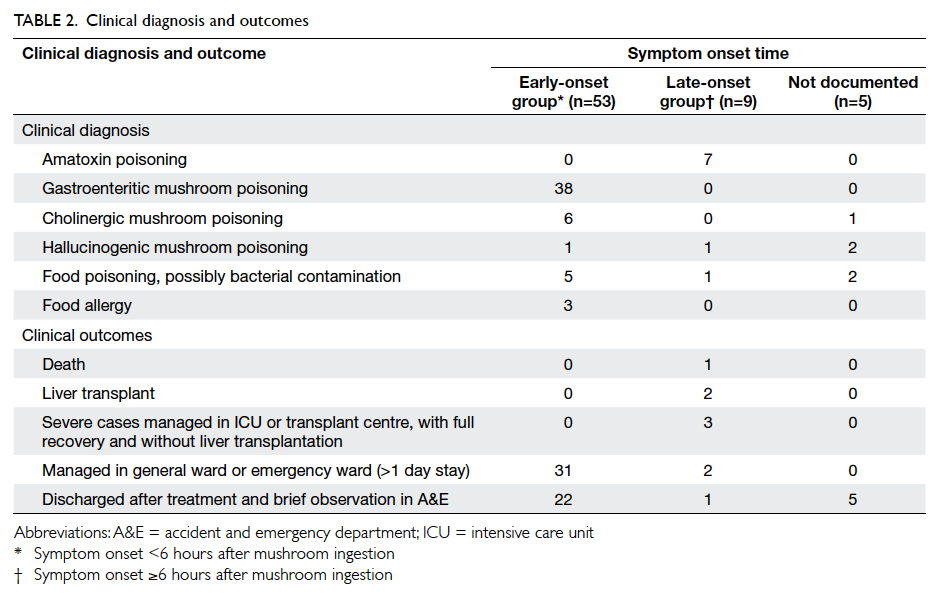
The symptom onset time was documented
in 62 patients (Table 2). Among them, 53 patients developed symptoms within 6 hours of mushroom
consumption (early-onset group). The median
time of symptom onset was 2 hours post-ingestion
(interquartile range [IQR], 2). Most patients (50 out
of 53) presented with early-onset gastrointestinal
symptoms. No severe clinical outcomes were
observed in this group of patients and all recovered
with symptomatic treatment and short duration of
hospital care.
Symptoms developed 6 hours or more after
mushroom consumption in nine patients (late-onset
group). The median time of symptom onset
was 11 hours post-ingestion (IQR, 2). This group
of patients represented potentially life-threatening
mushroom poisoning. All seven cases of amatoxin
poisoning in this case series were found in this
group. The remaining two cases included one case
of hallucinogenic mushroom poisoning caused by
Tylopilus nigerrimus, and one case of food poisoning.
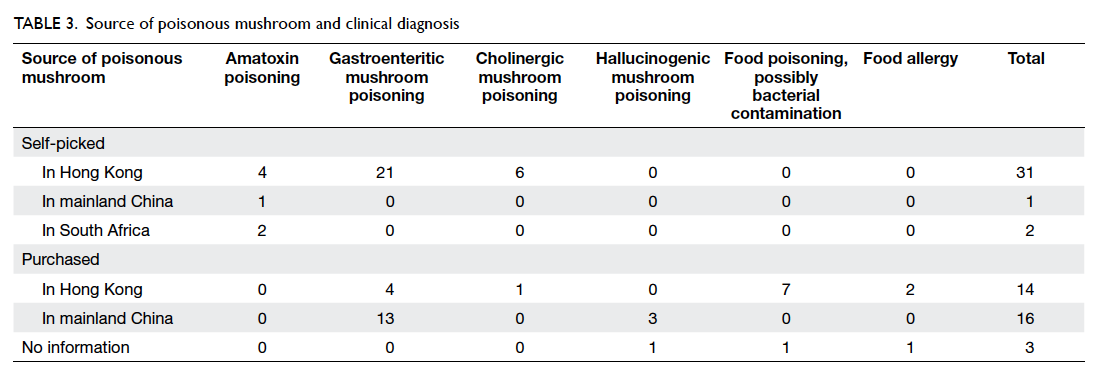
The source of poisonous mushrooms was
documented in 64 cases (Table 3). In 34 (51%) cases, the mushrooms were self-picked from a park,
hillside, or roadside. The locations were usually close
to the patient’s home. On the other hand, 14 (21%)
cases purchased the mushrooms in Hong Kong
and 16 (24%) purchased them in mainland China.
All patients with amatoxin poisoning collected the
mushroom from the wild. The source of mushrooms
was not documented in three (4%) cases.
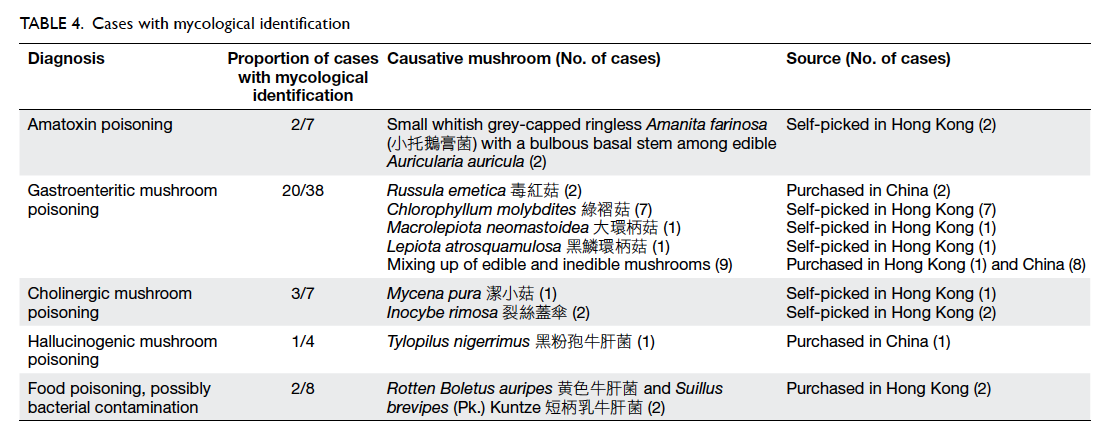
Mycological identification was achieved in 28
cases (Table 4). The diagnosis of amatoxin poisoning
was confirmed by the presence of amatoxin and/or
phallacidin in the urine of five patients.
Discussion
The aim of this study was to describe the pattern
of mushroom poisoning in Hong Kong. Four
mushroom poisoning syndromes, together with food
poisoning and food allergy, were identified to be the
cause of all mushroom poisoning cases in this study.
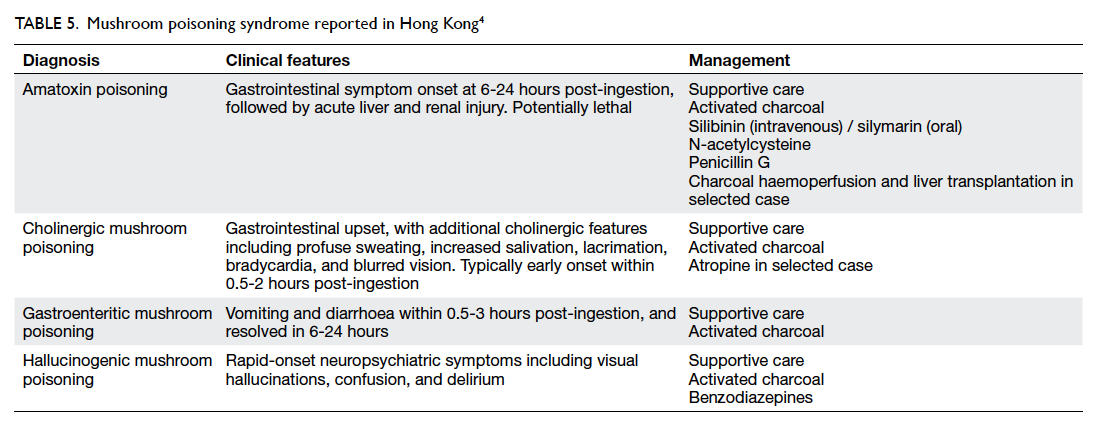
The typical clinical features and the management of
the four local mushroom poisoning syndromes are
summarised in Table 5.4
As an extensive urban city, commercially
sold cultivated mushrooms are easily available and
these are the mushrooms consumed by most Hong
Kong citizens every day. Nonetheless the Chinese
generally believes that wild-harvested products,
including mushrooms, have higher nutritional and
medicinal values. The risky behaviour of collecting
and consuming wild mushrooms was considered
to be rare in Hong Kong. This can be illustrated
by the relatively few reported cases of poisoning
during the study period. There are over 388 known
species of mushroom in Hong Kong,5 of which fewer
than 10% are edible, and a majority have unknown
edibility. Although mushrooms are macroscopic
organisms with visible morphological features, many
mushroom species share a similar appearance and
misidentification is common. There is no correlation
between a particular morphological feature and
poisonous nature of a mushroom species. Even
with genus Amanita, there are edible and inedible
species. There is no simple way to differentiate edible
and poisonous mushroom species. Even in expert
hands, mushroom identification frequently depends
on the microscopic features that can usually be seen
in a laboratory setting. Different edible and inedible
or poisonous mushroom species can share a similar
habitat and grow in close proximity in the wild.
Collection of mixed species often happens. Cooking
or other means of food processing cannot detoxify
a poisonous mushroom. With the report of life-threatening amatoxin poisoning from ingestion of local
wild mushrooms, Hong Kong citizens would be well
advised to stop the risky behaviour of consuming
self-picked mushrooms from the wild.
Consumption of poisonous mushrooms
can cause various signs and symptoms, such as
gastroenteritis, disturbances in central nervous
system, and liver failure.3 As mushroom identification
is usually not available early on in patient care,
doctors should treat their patients according to the
clinical syndrome (Table 54). An important predicting factor to consider is the latency from ingestion to
onset of symptoms. The finding of our case series
is compatible with overseas reports.3 6 Patients with
early-onset symptoms, typically within 6 hours
post-ingestion, all had a benign course of disease
(Table 2). The mainstay of treatment is supportive,
with intravenous fluids, antiemetic, antispasmodics,
or analgesic for those patients who present with
gastrointestinal symptoms.
Seven cases of amatoxin poisoning reported
in this case series confirms the existence of deadly
amatoxin-containing mushroom in our locality.
Poisonous Amanita species have long been found
in Hong Kong. Although local cases of amatoxin
poisoning have not been reported in Hong Kong
before 2013, it has been well-reported in mainland
China.7 8 9 According to a report published by
Guangzhou Municipal Centre for Disease Control
and Prevention, there were 92 cases of mushroom
poisoning with 13 deaths in the years 2002 to 2005.9
The reported species of mushroom involved in 70%
of cases were the amatoxin-containing mushroom
Amanita exitialis and the gastroenteritic mushroom
Chlorophyllum molybdites.9 For amatoxin poisoning,
the latency between ingestion and onset of
symptoms was typically 6 to 24 hours.3 For our seven
cases of amatoxin poisoning, this latency ranged
from 8 to 12 (median, 11) hours. There were four
male and three female patients, with a median age
of 44 (range, 29-74) years. All cases presented with
persistent vomiting and diarrhoea, deranged liver
function tests, and were able to give a history of wild
mushroom ingestion. Three were imported cases.
Two of them ate wild mushrooms in South Africa
and one patient ate wild mushrooms in China.
In four patients, wild mushrooms were picked
locally in the country park of the New Territories.
One imported case presented to hospital in Hong
Kong 5 days after wild mushroom consumption
and died of multi-organ failure soon after hospital
admission. The remaining six cases were managed
according to overseas experience in the treatment
of amatoxin poisoning.10 11 12 Treatment included
intravenous silibinin, oral silymarin, intravenous
N-acetylcysteine, oral multiple-dose activated
charcoal, high-dose intravenous penicillin, and early charcoal haemoperfusion. Two
local cases progressed to liver failure and required
liver transplantation. The remaining four cases
recovered with medical treatment. The diagnosis of
amatoxin poisoning was confirmed by the presence
of amatoxin and/or phallacidin in the urine in
five patients. Mycological examination identified
Amanita farinosa as the causative mushroom in a
local incident with two patients (Table 4). This is the
first report of this Amanita species in Hong Kong.
Hallucinogenic mushroom poisoning has
not been previously reported locally. The clinical
presentation of our four cases included dizziness,
headache, generalised weakness and numbness.
Three out of four patients presented with visual
hallucination. Although one patient did not report
any hallucinations, the patient was included as
a suspected case of hallucinogenic mushroom
poisoning based on compatible neurological
symptoms following consumption of porcini. The
symptom onset time was documented in two cases
and was 2 hours and 10 hours post-ingestion. The
source of mushroom was recorded in three cases as
mainland China. In only one case was mycological
identification performed (Table 4).
There were 13 cases of bolete poisoning in this
case series. All cases were related to consumption
of porcini. Porcini is considered to be a delicacy by
many mushroom lovers. It includes a number of
edible Boletus species, with Boletus edulis being the
best known. Not all Boletus are edible, however, and
mixing edible and inedible species is possible in wild
mushroom harvesting. There are reports of bolete
poisoning in English and Chinese literature.6 Bolete
consumption has been associated with outbreaks
of neuropsychiatric symptoms in Southwest China
(eg Yunnan province) in recent years.13 14 15 According
to these reports, consumption of inedible boletes
typically presented with gastrointestinal and
neurological symptoms including visual and auditory
hallucination. In our case series, two out of 13 cases
of bolete poisoning presented with neuropsychiatric
symptoms without gastrointestinal symptoms. The
two unrelated cases purchased mushrooms from
Yunnan province. The first patient presented with
numbness and weakness in all four limbs, dizziness,
and malaise after mushroom consumption. The
time of symptom onset was not documented and
symptoms resolved on the same day as mushroom
consumption. No mushroom sample was obtained
for identification. The second patient developed
dizziness, malaise, and visual hallucination 10 hours
after mushroom consumption. Her symptoms
resolved 48 hours post-ingestion. The causative
mushroom was identified as T nigerrimus, an inedible
bolete. Hallucinogenic mushroom poisoning caused
by T nigerrimus has not been reported in the English
literature.
In the cases of bolete poisoning, 11 out of 13
presented with gastrointestinal symptoms after
mushroom consumption. Four patients purchased
the mushrooms locally, and seven purchased the
mushrooms in China. In most cases, the mushrooms
were commercially packed as a product containing
wild-harvested boletes in dried slices. Mycological
identification was performed in 10 cases. These 10
cases represented six poisoning incidents. In five
incidents involving eight patients, the wild-harvested
porcini showed mixing up of edible porcini and
inedible boletes. In the remaining one incident, the
mushrooms were identified as an edible species,
although microscopic examination revealed them to
be rotten with dried worm and mold (Table 4). The diagnosis was food poisoning with possibly bacterial
contamination of spoiled mushroom in this incident.
Conclusion
Most cases of mushroom poisoning in Hong Kong
follow a benign course. Life-threatening cases of
amatoxin poisoning are occasionally seen. Doctors
should consider this diagnosis in patients who
present with gastrointestinal symptoms whose onset
is 6 hours or more after mushroom consumption.
In this review, all patients with amatoxin poisoning
picked the poisonous mushroom from the wild.
Wild mushroom picking and consumption should
be strongly discouraged.
References
1. Centre for Health Protection. Food poisoning associated
with wild mushroom. Communicable Disease Watch
2005;2:41-2.
2. Chan TY, Chiu SW. Wild mushroom poisonings in
Hong Kong. Southeast Asian J Trop Med Public Health
2011;42:468-9.
3. Diaz JH. Syndromic diagnosis and management of
confirmed mushroom poisonings. Crit Care Med
2005;33:427-36. Crossref
4. Hoffman RS, Howland MA, Lewin NA, et al. Goldfrank’s
toxicologic emergencies. 10th edition. New York: McGraw-Hill Education; 2015.
5. Chang ST, Mao XL. Hong Kong mushrooms. Hong Kong:
The Chinese University Press; 1995.
6. Schenk-Jaeger KM, Rauber-Lüthy C, Bodmer M,
Kupferschmidt H, Kullak-Ublick GA, Ceschi A. Mushroom
poisoning: a study on circumstances of exposure and
patterns of toxicity. Eur J Intern Med 2012;23:e85-91. Crossref
7. Jin LM, Li Q. 金連梅, 李群. [Analysis of food poisoning incidents during 2004 to 2007 in China] 2004-2007年全國食物中毒事件分析
[in Chinese]. [Disease Surveillance] 疾病監測 2009;24:459-61.
8. Guo SH, Liu FQ, Liu XY, Chen Y. 郭綬衡,劉富强,劉秀英,陳焱. [Analysis of food-borne disease incidents
in Jiangsu, Zhejiang, Hunan, Hubei and Hebei Province
during 2000 to 2002] 2000-2002年江蘇、浙江、湖南、湖北、河北五省食物源性疾病發病情况分析 [in Chinese].
[Practical Preventive Medicine] 實用預防醫學 2004;11:867-71.
9. Mao XW, Li YY, He JY, Jing QL. 毛新武,李迎月,何潔儀,景飲隆. [Investigation of mushroom poisoning in Guangzhou City from 2000 to 2005] 廣州市 2000-2005年蘑菇中毒調查 [in Chinese]. [China Tropical Medicine] 中國熱帶醫學 2007;7:166-7.
10. Ward J, Kapadia K, Brush E, Salhanick SD. Amatoxin
poisoning: case reports and review of current therapies. J
Emerg Med 2013;44:116-21. Crossref
11. Enjalbert F, Rapior S, Nouguier-Soulé J, Guillon S,
Amouroux N, Cabot C. Treatment of amatoxin poisoning:
20-year retrospective analysis. J Toxicol Clin Toxicol
2002;40:715-57. Crossref
12. Giannini L, Vannacci A, Missanelli A, et al. Amatoxin
poisoning: a 15-year retrospective analysis and follow-up
evaluation of 105 patients. Clin Toxicol (Phila) 2007;45:539-42. Crossref
13. Ji X, Ma Z, Zhu H, Pan YZ. 及曉,馬征,朱輝,潘軼竹.
[Report of two cases of mental disorder due to ingestion
of Boletus speciosus] 小美牛肝菌所致精神障礙2例 [in
Chinese]. [Clinical Journal of Psychiatry] 臨床精神醫學雜誌 2014;24:240.
14. Liu MW, Zhou H, Hao L, Zhang MQ. 劉明偉,周惠,郝麗,張明謙. [Analysis of 61 cases of boletus poisoning]
牛肝菌中毒61例分析 [in Chinese]. [Chinese Journal of
Misdiagnosis] 中國誤診學雜誌 2008;8:111.
15. Zhou YJ, Wei GL, Chen GH. 周亞娟,魏桂蘭,陳桂華.
[Investigation of Rhubarb boletus food poisoning] 一起黄粉牛肝菌食物中毒事件調查 [in Chinese]. [Occupational Health and Damage] 職業衛生與病傷2008;23:115-6.