Hong Kong Med J 2016 Feb;22(1):6–10 | Epub 9 Oct 2015
DOI: 10.12809/hkmj154568
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE
Excess mortality for operated geriatric hip fracture in Hong Kong
LP Man, MB, BS, MRCSEd;
Angela WH Ho, MB, ChB, FHKAM (Orthopaedic Surgery);
SH Wong, MB, BS, FHKAM (Orthopaedic Surgery)
Department of Orthopaedics and Traumatology, Caritas Medical Centre, Shamshuipo, Hong Kong
Corresponding author: Dr LP Man (mlp257@ha.org.hk)
Abstract
Introduction: Geriatric hip fracture places an
increasing burden to health care systems around the
world. We studied the latest epidemiology trend of
geriatric hip fracture in Hong Kong, as well as the
excess mortality for patients who had undergone
surgery for hip fracture.
Methods: This descriptive epidemiology study was
conducted in the public hospitals in Hong Kong. All
patients who underwent surgery for geriatric hip
fracture in public hospitals from January 2000 to
December 2011 were studied. They were retrieved
from the Clinical Management System of the
Hospital Authority of Hong Kong. Relevant data
were collected using the Clinical Data Analysis and
Reporting System of the Hospital Authority. The
actual and projected population size, and the age- and
sex-specific mortality rates were obtained from
the Census and Statistics Department of Hong Kong.
The 30-day, 1-year and 5-year mortality, and excess
mortality following surgery for geriatric hip fracture
were calculated.
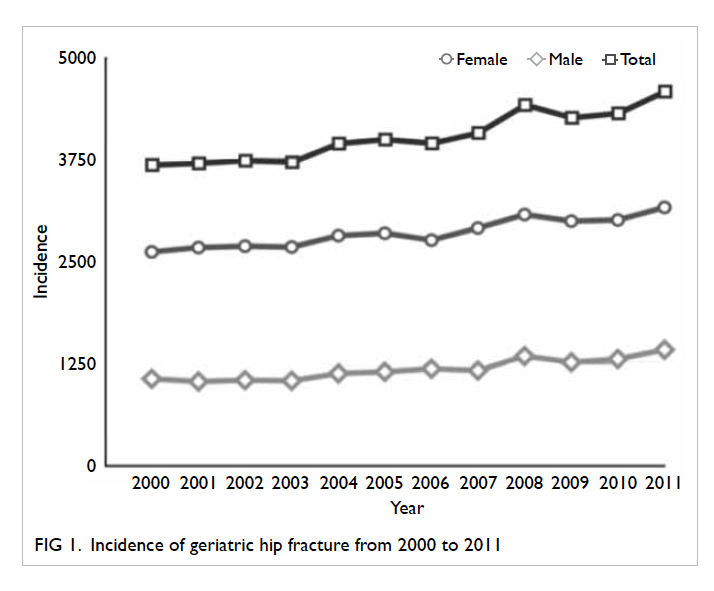
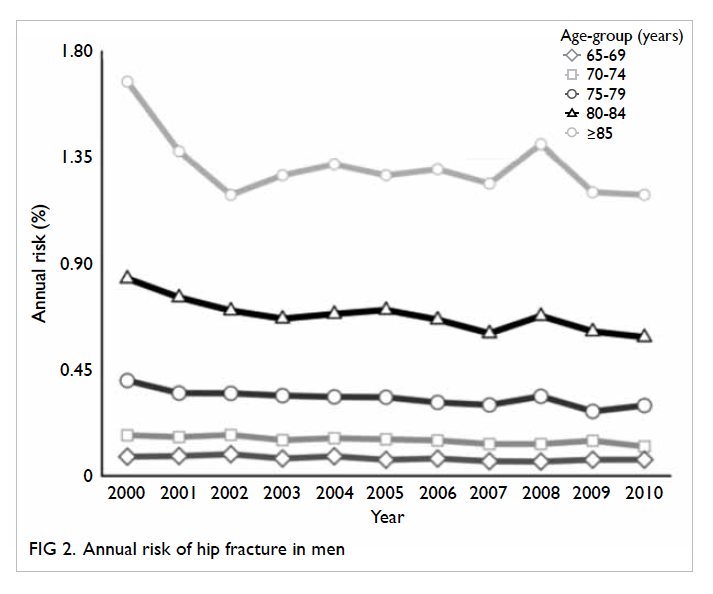
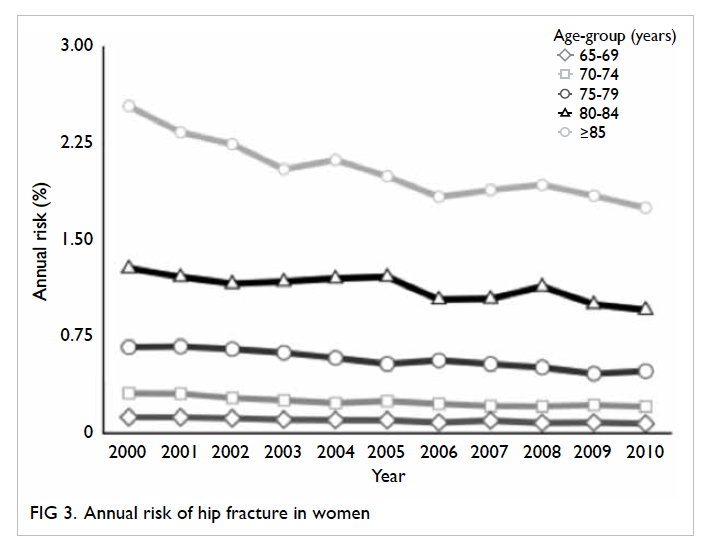
Results: There was a steady increase in the incidence
of geriatric hip fracture in Hong Kong. The annual
risk of geriatric hip fracture was decreasing in both
sexes. Female patients aged 65 to 69 years had the
lowest 1-year and 5-year mortality of 6.91% and
23.80%, respectively. Advancing age and male sex
were associated with an increase in mortality and a
higher excess mortality rate following surgery.
Conclusion: The incidence of geriatric hip fracture
is expected to increase in the future. The exact
reason for a higher excess mortality rate in male
patients remains unclear and should be the direction
for future studies.
New knowledge added by this study
- Advancing age and male sex were associated with an increase in mortality and a higher excess mortality rate in Hong Kong following surgery for hip fracture.
- The burden of geriatric hip fracture is expected to increase.
- Future studies should investigate the cause of an increased excess mortality in male patients who sustain a geriatric hip fracture.
Introduction
Geriatric hip fracture places an increasing burden
on health care service providers around the world.
Previous studies have shown that it is associated
with significant morbidity and mortality.1 2 3 With
the ageing population in many parts of Asia, it has
been estimated that over half of all hip fractures
will occur in Asia in 2050.4 Studies in France5 and the US6 have reported a drop in the incidence rate
of geriatric hip fracture in the elderly population.
This trend, however, has not been echoed by similar
studies in Korea7 and Japan.8 Epidemiological studies performed in Hong Kong in 2007 and 2012 showed
that, similar to western countries, there was a drop in
the incidence rate of hip fracture in the territory.9 10
Hong Kong has one of the longest life
expectancies in the world.11 The total number of
geriatric hip fractures is expected to increase. It
will therefore be important for policy-makers and
society as a whole to adequately forecast future
trends in the disease to prepare for the challenges
ahead. This study aimed to analyse the latest trend
in the epidemiology of geriatric hip fracture in Hong
Kong, as well as to investigate the mortality rate and
excess mortality rate in patients who underwent
surgery for geriatric hip fracture.
Methods
Approximately 98% of geriatric hip fractures are
managed in public hospitals run by the Hospital
Authority of Hong Kong.10 All patients admitted to
a public hospital in Hong Kong are assigned a code
in the Clinical Management System by the attending
doctor(s). The system also includes information
on age, sex, principal diagnosis, and period of
hospitalisation. Relevant data, including date of
death, were collected using the Clinical Data Analysis
and Reporting System (CDARS) from the Hospital
Authority. All cases between January 2000 and
December 2011 with a disease coding of acute hip
fracture (ICD-9-CM diagnosis codes 820.8, 820.09,
820.02, 820.03, 820.20, and 820.22) were retrieved.
Operations for geriatric hip fracture were defined as
a patient-episode with ICD-9-CM procedure code of
81.52, 51.51, 81.40, 79.15, 79.35, or 78.55.
Only patients with a disease code for acute
hip fracture and procedure code for geriatric hip
fracture were included in the current study. Patients
who were non-Chinese, who had an old fracture,
were managed non-operatively, had a second hip
fracture or complications of primary hip fracture
were excluded. Based on the date of death, we
analysed the 30-day and 1-year mortality regardless
of cause of death. Postoperative 5-year mortality rate
was calculated based on data from patients who underwent surgery from year 2000 to 2006.
Excess mortality is defined by the World
Health Organization as “Mortality above what
would be expected based on the non-crisis mortality
rate in the population of interest.”12 In this study, the
excess mortality rate was calculated by subtracting
the age- and sex-specific mortality from the age- and
sex-specified 1-year mortality of operated geriatric
hip fracture. The age- and sex-specific mortality rates
for the year 2006 were used for analysis. The actual
and projected population size, and the age- and
sex-specific mortality rates13 were obtained from the
Census and Statistics Department of the HKSAR
Government.
Results
From January 2000 to December 2011, the annual
number of patients admitted to public hospitals and
who underwent surgery for hip fracture increased
from 3678 to 4579. The annual incidence of geriatric
hip fracture during the study period is shown in
Figure 1. A slightly decreasing annual risk of hip
fracture was observed for both male and female
patients (Figs 2 and 3).
A total of 48 992 cases were retrieved after
excluding non-Chinese patients, old fractures,
cases managed non-operatively, second hip
fractures, repeated admission for the same fracture, and
complications of primary hip fracture.
Patient age ranged from 65 to 112 years with
a mean and median age of 82.1 and 82.0 years,
respectively. The overall 30-day and 1-year mortality
was 3.01% and 18.56%, respectively.
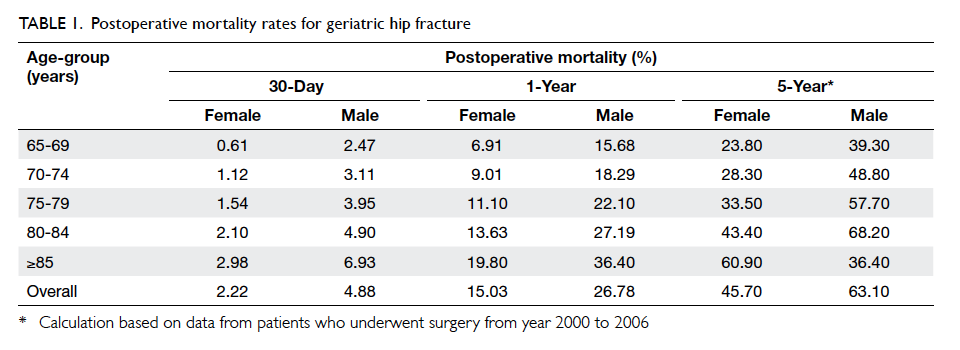
The age- and sex-specific mortality after 30
days, 1 year, and 5 years for operated hip fracture are
shown in Table 1. Female patients aged 65 to 69 years
had the lowest 1-year and 5-year mortality of 6.91%
and 23.80%, respectively. An increase in mortality
was observed with advancing age and male sex.
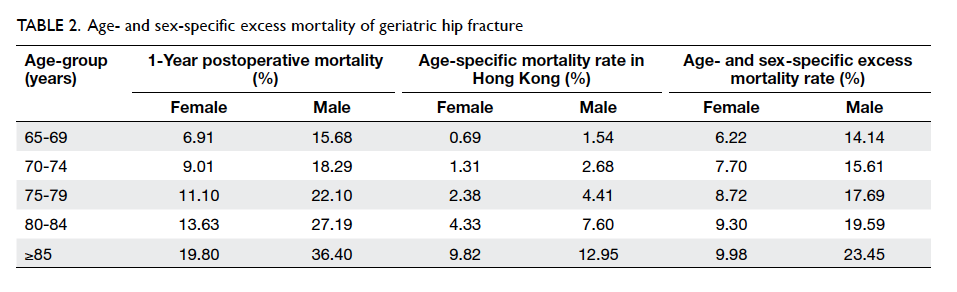
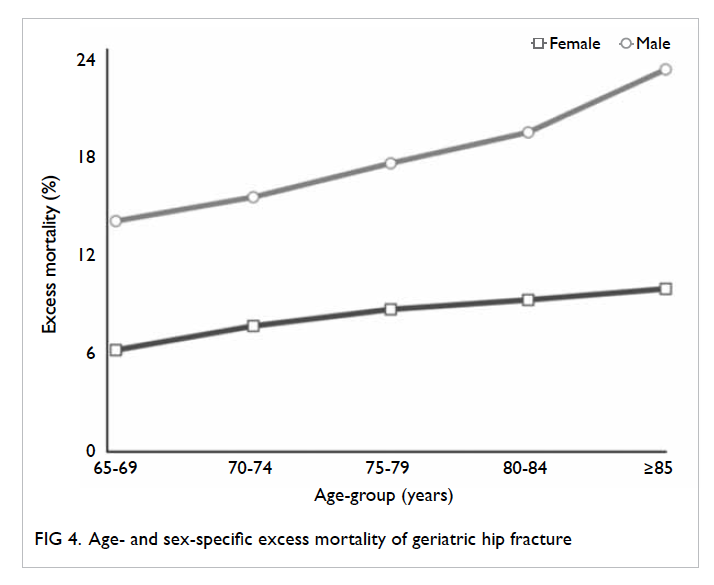
The excess mortality rate in different age and
sex groups is shown in Table 2 and Figure 4. Male
gender and increasing age were associated with
a higher excess mortality rate after operation for
geriatric hip fracture. The excess mortality for a male
patient aged ≥85 years was 23.45%.
Discussion
A slight decrease in the annual risk of geriatric hip
fracture was noted in this study. This trend echoes that
of similar studies in the territory and in some western
countries.5 6 10 Such a decrease has been postulated
to be related to improved availability of medical
intervention to prevent osteoporosis, increased
attention to menopause and hormonal replacement
therapy, changes in lifestyle, and community fall prevention
programmes. Nonetheless few studies
have been able to prove any causal relationship.
Surgery is generally offered to patients with
geriatric hip fracture in order to decrease the
morbidity and mortality associated with prolonged
immobilisation. In this study, patients who were
managed non-operatively were excluded as they
represented a very small proportion of patients
(estimated to be <1%) with poor pre-morbid medical
conditions and very high anaesthetic risk.
Despite the decreasing annual risk of geriatric
hip fracture, it is important to relate this to the ageing
population in the territory. Using the projected
percentage of elderly aged ≥65 years in Hong Kong,11
and assuming that the annual risk of hip fracture
remains the same, we estimate that there will be
more than 6300 cases of hip fracture in the year 2020.
In the year 2040, the annual incidence of geriatric
hip fracture will be more than 14 500, more than a
3-fold increase from 2011. Unless effective primary
prevention measures are put in place, the burden of
geriatric hip fracture on the public health system will
continue to increase. Policy-makers should invest in
the relevant specialties and departments in order to
tackle the inevitable challenges ahead.
To our knowledge this is the first study to
review the excess mortality of operated geriatric hip
fracture in the territory. A systematic epidemiological
review by Abrahamsen et al14 showed that the 1-year
excess mortality rate following hip fracture ranged
from 8.4% to 36%. In this study, the 1-year excess
mortality following surgery for geriatric hip fracture
ranged from 6.22% to 23.45%. Echoing the result of
Abrahamsen et al,14 we also identified that men had
a higher excess mortality rate after operation for
geriatric hip fracture. The reasons for this higher
excess mortality rate in males remain unclear. Endo
et al15 reported that male gender was a risk factor
for sustaining postoperative complications such as
pneumonia, arrhythmia, delirium, and pulmonary
embolism, even after controlling for age and the
American Society of Anesthesiologists rating, as
well as a higher mortality 1 year after hip fracture.
Another study by Wehren et al16 reported an
increased rate of death from infection in males for
at least 2 years after hip fracture, suggesting that
infection may contribute to the differential risk of
death.
There are limitations to the present study.
Patients with geriatric hip fracture who were treated
in the private sector were not included, although
they constituted only a small proportion of the
total number of cases. Chau et al10 reported that
approximately 98% of hip fractures were managed in
the Hospital Authority.
In the CDARS of the Hospital Authority, the
date of death was provided by the death registry of
the Immigration Department of Hong Kong. We
were unable to capture data for deaths that occurred
outside the territory. Under the laws of Hong Kong,
only deaths that occur in Hong Kong are registered
with the Deaths Registries. According to the Census
and Statistics Department, approximately 9% of
the elderly population resides in the mainland.17 As
Hong Kong residents are currently not eligible for
free or subsidised health services in the mainland,
we believe many elderly people will return to Hong
Kong for medical treatment.
Other risk factors that may contribute to the
excess mortality such as smoking and pre-morbid
health status were not included in the present
study. Further studies should also investigate the
incidence and mortality of other fragility fractures.
The effect of primary and secondary prevention
by anti-osteoporotic medications on the incidence
of geriatric hip fracture is also a potential area for
further study.
Conclusion
Geriatric hip fracture will continue to be a
major challenge for the health care system in the
foreseeable future. Despite the emphasis on early
surgery for geriatric hip fractures in recent years, the
risk of premature death remained high for patients
who underwent surgery for hip fracture. Future
studies should be directed to identify the causes of
this excess mortality and patients who are
at increased risk of premature death, so that early
interventions can be initiated to reduce their risk.
Acknowledgements
The authors would like to thank Mr Tony Kwok and
the CDARS team of Hospital Authority for their help
in data retrieval.
References
1. Mullen JO, Mullen NL. Hip fracture mortality. A
prospective, multifactorial study to predict and minimize
death risk. Clin Orthop Relat Res 1992;(280):214-22.
2. Omsland TK, Emaus N, Tell GS, et al. Mortality following
the first hip fracture in Norwegian women and men (1999-2008). A NOREPOS study. Bone 2014;63:81-6. Crossref
3. Randell AG, Nguyen TV, Bhalerao N, Silverman SL,
Sambrook PN, Eisman JA. Deterioration in quality of life
following hip fracture: a prospective study. Osteoporos Int
2000;11:460-6. Crossref
4. Cooper C, Campion G, Melton LJ 3rd. Hip fractures
in the elderly: a world-wide projection. Osteoporos Int
1992;2:285-9. Crossref
5. Maravic M, Taupin P, Landais P, Roux C. Change in
hip fracture incidence over the last 6 years in France.
Osteoporos Int 2011;22:797-801. Crossref
6. Brauer CA, Coca-Perraillon M, Cutler DM, Rosen AB.
Incidence and mortality of hip fractures in the United
States. JAMA 2009;302:1573-9. Crossref
7. Yoon HK, Park C, Jang S, Jang S, Lee YK, Ha YC. Incidence
and mortality following hip fracture in Korea. J Korean
Med Sci 2011;26:1087-92. Crossref
8. Hagino H, Yamamoto K, Ohshiro H, Nakamura T,
Kishimoto H, Nose T. Changing incidence of hip, distal
radius, and proximal humerus fractures in Tottori
Prefecture, Japan. Bone 1999;24:265-70. Crossref
9. Kung AW, Yates S, Wong V. Changing epidemiology
of osteoporotic hip fracture rates in Hong Kong. Arch
Osteoporos 2007;2:53-8. Crossref
10. Chau PH, Wong M, Lee A, Ling M, Woo J. Trends in hip
fracture incidence and mortality in Chinese population
from Hong Kong 2001-09. Age Ageing 2013;42:229-33. Crossref
11. Hong Kong Population Projections 2012-2041, Census
and Statistics Department. Available from: http://www.censtatd.gov.hk/. Accessed Jun 2015.
12. Definitions: emergencies. Available from: http://www.who.int/hac/about/definitions/en/. Accessed Jun 2015.
13. The mortality trend in Hong Kong, 1981 to 2013. Hong Kong
Monthly Digest of Statistics. November 2014, HKSAR: Census and Statistics Department. Available from: http://www.statistics.gov.hk/pub/B71411FB2014XXXXB0100.pdf. Accessed Jun 2015.
14. Abrahamsen B, va Staa T, Ariely R, Olson M, Cooper
C. Excess mortality following hip fracture: a systematic
epidemiological review. Osteoporos Int 2009;20:1633-50. Crossref
15. Endo Y, Aharonoff GB, Zuckerman JD, Egol KA, Koval KJ.
Gender differences in patients with hip fracture: a greater
risk of morbidity and mortality in men. J Orthop Trauma
2005;19:29-35. Crossref
16. Wehren LE, Hawkes WG, Orwig DL, Hebel JR,
Zimmerman SI, Magaziner J. Gender differences in
mortality after hip fracture: the role of infection. J Bone
Miner Res 2003;18:2231-7. Crossref
17. Characteristics of Hong Kong older persons residing in
the Mainland of China. Hong Kong Monthly Digest of
Statistics. September 2011. HKSAR: Census and Statistics
Department. Available from: http://www.statistics.gov.hk/pub/B71109FC2011XXXXB0100.pdf. Accessed Jul 2015.